Abstract
The present report describes the case of a patient who underwent maxillary sinusitis right after dental implant installation with sinus lifting. Computed tomography scan revealed a dental implant (#16) was protruded inside the right maxillary sinus and confirmed the obstruction of ostium. A symptom remission was gained with the dual approaches combined by functional endoscopic sinus surgery and an intra-oral approach. Fully recovered function and healing of sinus were identified after 10 months follow-up. We report the case of sinusitis caused by protrusion of implants with sinus floor lift procedures and propose that practitioners should be aware of the possible its complications and management.
Rehabilitation of masticatory function after dental implants are placed in the partial or full edentulous area has become routine; however, implantation can occasionally be compromised by anatomical limitations as well as the status of alveolar bone and surrounding soft tissue. Implantation around the posterior maxilla area is often challenging because of alveolar bone resorption, sinus pneumatization or other reasons1. To overcome these problems, maxillary sinus lifting and sinus bone grafting are often recommended, although these procedures have uncommon complications such as maxillary sinusitis and infection. Inadequate maxillary bone thickness, along with poor surgical planning and lack of experience, is also associated with protrusion of implants into the maxillary sinus2,3 or grafting material migration to the paranasal sinuses (PNS)4,5. Generally, intraoral approaches such as Caldwell-Luc approach, inferior meatal osteotomy or oro-antral fistula closure have been popular options for the treatment of post-op sequelae. However, these techniques have been insufficient for full recovery of maxillary sinus function. For complete recovery of maxillary sinus function and rapid resolution of sinusitis, functional endoscopic sinus surgery (FESS) is recommended, which is favored over the Caldwell-Luc approach because of positive outcomes such as shorter hospital stay and lower morbidity6. We report a case of maxillary sinusitis related to failed osteotome sinus elevation technique as well as successful management with FESS in combination with an intra-oral approach.
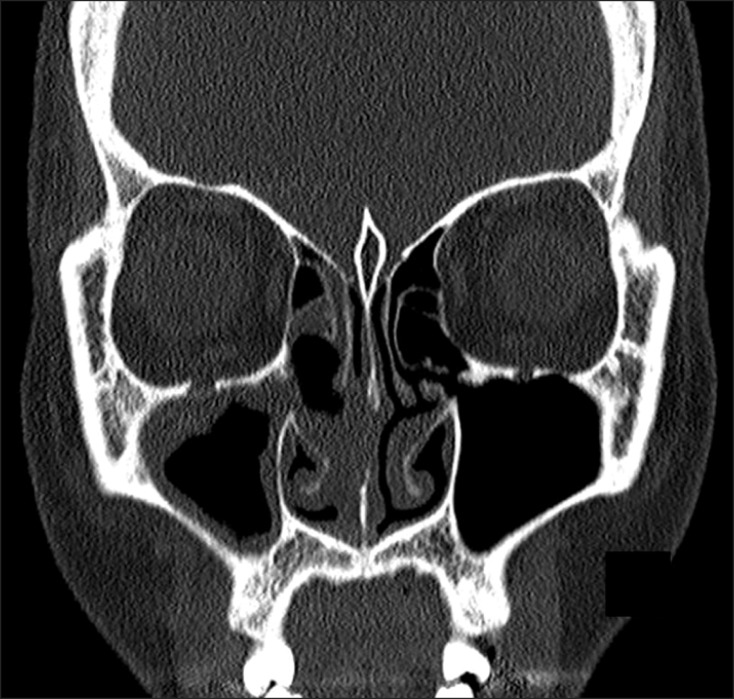
A 39-year-old female was referred to our dental department due to considerable pain in the right zygoma area with headache in the right temporal region. The patient had a history of extraction of #16 approximately 5 months prior due to a vertical crack, and underwent single dental implant installation with the osteotome technique for #16 in a local dental clinic 3 days prior to presentation. Panoramic view revealed that the single implant was protruding into the right maxillary sinus and the radiopacity of the sinus was increased.(Fig. 1) Medical therapy was administered, including empirical antibiotics (penicillin, clindamycin), non-steroidal anti-inflammatory drugs, expectorants and antihistamines, which were prescribed to mitigate symptoms; however, the patient showed no improvement after 4 weeks of follow-up, and the persistence of signs and symptoms of discomfort indicated that further investigation was needed. Coronal view computed tomography (CT) revealed definite signs of sinusitis with opacification of the right maxillary sinus as well as ethmoidal sinus, and confirmed that a dental implant was protruding approximately 5 mm into the sinus with a displaced bone fragment from the sinus floor at the apical portion of the implant.(Fig. 2) It was unclear whether bone grafting had been performed. Water's view also revealed increased density and haziness in the right maxillary sinus.(Fig. 3) Based on this evidence of obstruction of the ostium of the right nasal cavity and infection of the mucocele of the right maxillary sinus, we consulted an otolaryngologist and concluded that an intra-oral approach alone would not be sufficient to remove the mucocele and potentially scattered graft particles. Implant removal was also considered because the fixture was loose; therefore, FESS was performed in combination with an intra-oral approach under general anesthesia followed by admission of the patient. The operation was conducted by cooperative team approach, including an oral-maxillofacial surgeon and otolaryngologist. After the endoscope was inserted into the nose, cotton soaked with epinephrine was applied to the middle meatus for 5 minutes, then cotton was removed. The middle turbinate was widely excised so that pus and infected bone graft particles could be flushed from the sinus cavity. The ostium was exposed by removal of the uncinate process in the middle meatus to access to ostium and the ethmoidal sinus. Edematous, hyperplastic nasal mucosa within the sinus was enucleated after the natural ostium was surgically enlarged (Fig. 4), then the sinus was irrigated with normal saline until no additional free-floating particles were observed. During this procedure, removal of the sinus mucosa of the maxillary was not attempted. Implant removal and primary closure of the oro-antral fistula were performed.(Fig. 5) The patient received polyvinyl acetal absorbent nasal packing for 1 week, no complications occurred and symptoms improved gradually over the healing period. The radiopaque phase of the sinus cavity was remarkably decreased in the right maxillary sinus 1 week postoperatively, though mucosal thickening was still observed.(Fig. 6) However, full recovery of the sinus was evidenced on transverse dental CT at the 10-month follow-up visit.(Fig. 7)
In many cases of maxillary sinusitis, dysfunction of mucociliary clearance is a major clinical problem. The stagnation of secretions and obstruction of excretion from and ventilation within the maxillary sinus are predisposing factors for sinus infection7. The area between middle turbinate and lateral nasal wall often has the anatomical variance; therefore, edema of the mucosa can result in obstruction of the ostium and dysfunction of mucociliary function. Maxillary sinus floor lift has been reported to cause postoperative sinusitis8. The elevation of the Schneiderian membrane could affect a sinus homeostasis and lead to sinusitis by temporal obstruction of a physiological sinus drainage through the ostio-meatal unit (OMU)9. Mucosal inflammation caused by misplaced implants can similarly cause mucosal inflammation and stenosis of the OMU with detrimental effects on sinus ventilation. Recommended treatment for dental implant-related sinusitis typically involves surgical restoration for proper drainage and ventilation of the sinus, interrupting the described sequence of events that lead to sinus infection.
FESS is a relatively recent surgical procedure used in the treatment of maxillary sinusitis. It widens the OMU to facilitate sinus secretion from the PNS into the nasal cavity, as the patient's normal anatomical structures are preserved10. FESS is able to treat OMU alterations and remove displaced dental implants, though it does not allow for removal of implants that protrude into the sinus, as in the present case2. Intraoral approaches are a more suitable method for addressing oro-antral fistulas and removing implants from within the sinus, but they cannot repair OMU alterations and other aspects of sinusitis7. Simple elimination of the irritating stimulus, such as exposed or displaced implant, could also be considered. Reports in the literature indicated that implant exposure greater than 4 mm from the sinus floor can give rise to sinusitis or rhinosinusitis11. In this report, the implant fixture was removed due to not only the exposed length (5 mm), but also the significant lack of initial stability.
Though further studies are needed to evaluate the efficacy of FESS in treating recalcitrant implant-related sinusitis and its ability to prevent recurrence, the combination of FESS and an intra-oral approach should be considered a useful option for the restoration of normal naso-sinus homeostasis2. The authors report favorable results of this dual approach in the treatment of maxillary sinusitis following implantation with sinus lifting. Dental surgeons performing similar procedures should be aware of the possible complications that can arise from foreign debris invading the maxillary sinus.
References
1. Lee JK, Um HS, Chang BS. Retrospective study on the survival rate of the sinus perforated implants. J Korean Acad Periodontol. 2006; 36:891–900.
2. Ueda M, Kaneda T. Maxillary sinusitis caused by dental implants: report of two cases. J Oral Maxillofac Surg. 1992; 50:285–287. PMID: 1542071.

3. Quiney RE, Brimble E, Hodge M. Maxillary sinusitis from dental osseointegrated implants. J Laryngol Otol. 1990; 104:333–334. PMID: 2370457.

4. Galindo P, Sánchez-Fernández E, Avila G, Cutando A, Fernandez JE. Migration of implants into the maxillary sinus: two clinical cases. Int J Oral Maxillofac Implants. 2005; 20:291–295. PMID: 15839124.
5. Felisati G, Lozza P, Chiapasco M, Borloni R. Endoscopic removal of an unusual foreign body in the sphenoid sinus: an oral implant. Clin Oral Implants Res. 2007; 18:776–780. PMID: 17868385.

6. Chen YW, Huang CC, Chang PH, Chen CW, Wu CC, Fu CH, et al. The characteristics and new treatment paradigm of dental implant-related chronic rhinosinusitis. Am J Rhinol Allergy. 2013; 27:237–244. PMID: 23710961.

7. Chiapasco M, Felisati G, Zaniboni M, Pipolo C, Borloni R, Lozza P. The treatment of sinusitis following maxillary sinus grafting with the association of functional endoscopic sinus surgery (FESS) and an intra-oral approach. Clin Oral Implants Res. 2013; 24:623–629. PMID: 22404380.

8. Timmenga NM, Raghoebar GM, van Weissenbruch R, Vissink A. Maxillary sinusitis after augmentation of the maxillary sinus floor: a report of 2 cases. J Oral Maxillofac Surg. 2001; 59:200–204. PMID: 11213989.

9. Pignataro L, Mantovani M, Torretta S, Felisati G, Sambataro G. ENT assessment in the integrated management of candidate for (maxillary) sinus lift. Acta Otorhinolaryngol Ital. 2008; 28:110–119. PMID: 18646572.
10. Yang SN. The Inflammatory disease of the maxillary sinus associated with tooth extraction and implant. J Korean Dent Assoc. 2008; 46:727–733.
11. Raghoebar GM, van Weissenbruch R, Vissink A. Rhino-sinusitis related to endosseous implants extending into the nasal cavity. A case report. Int J Oral Maxillofac Surg. 2004; 33:312–314. PMID: 15287319.
Fig. 1
Panoramic view taken 5 days after right maxilla sinus bone grafting and #16 implantation revealed dental implant protrusion into the right maxillary sinus.

Fig. 2
Paranasal sinuses computed tomography revealed mucosal thickening and opacification with air bubbles in the right maxillary sinus and the protrusion of an implant fixture into the sinus, along with a bony fragment (arrow).

Fig. 3
Water's view computed tomography revealed increased density and haziness in the right maxillary sinus.

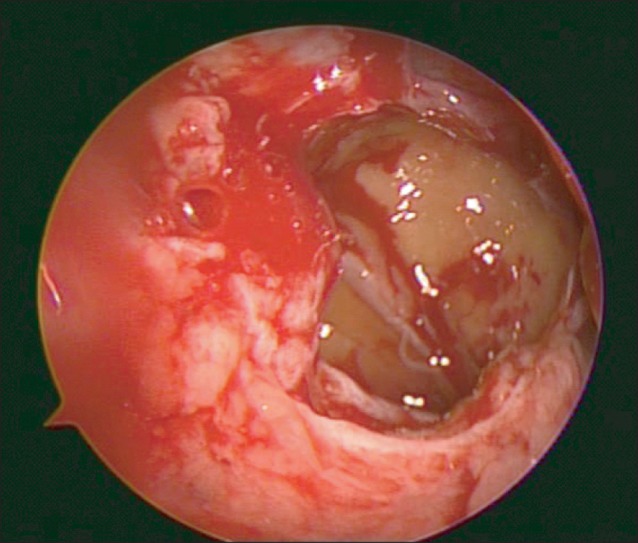
Fig. 5
An intra-oral approach allowed for the removal of the mobile dental implant and closure of the oro-antra fistula.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download