Abstract
There are some difficulties in approaching and removing the lesion in infratemporal fossa because of its anatomical location. After wide excision of tumor lesion, it is also difficult for reconstruction of mandibular condyle and cranium base on infratemporal fossa. Besides, there are some possibilities of cerebrospinal fluid leakage, intracranial infection and bone resorption. It is also challenging for functional reconstruction that allows normal mandibular movement, preventing mandibular condyle from invaginating into the skull. In this report, we present 14-month follow-up results of a patient who had undergone posterior segmental mandibulectomy including condyle and infratemporal calvarial bone and mandible reconstruction with free vascularized costochondral rib and calvarial bone graft to restoration of the temporomandibular joint area.
Go to : 
It is difficult to remove tumor lesions that extend to the infratemporal fossa, mandibular condyle, and cranial base. These lesions usually cause cerebrospinal fluid (CSF) leakage, intracranial infection, and bone resorption. There are many reconstructive surgeries to use for these cases, including temporalis myofascial flap1 and alloplastic total joint replacement2,3. Here, vascularized costochondral and calvarial bone grafts were used. These techniques cost less than the temporalis myofascial flap method and more effectively prevent the mandibular condyle from penetrating into the skull.
Ten months after surgery, the patient has good healing prognosis without any complications. We anticipate that vascularized costochondral and calvarial bone grafts can be widely used for many head and neck reconstruction surgeries.
Go to : 
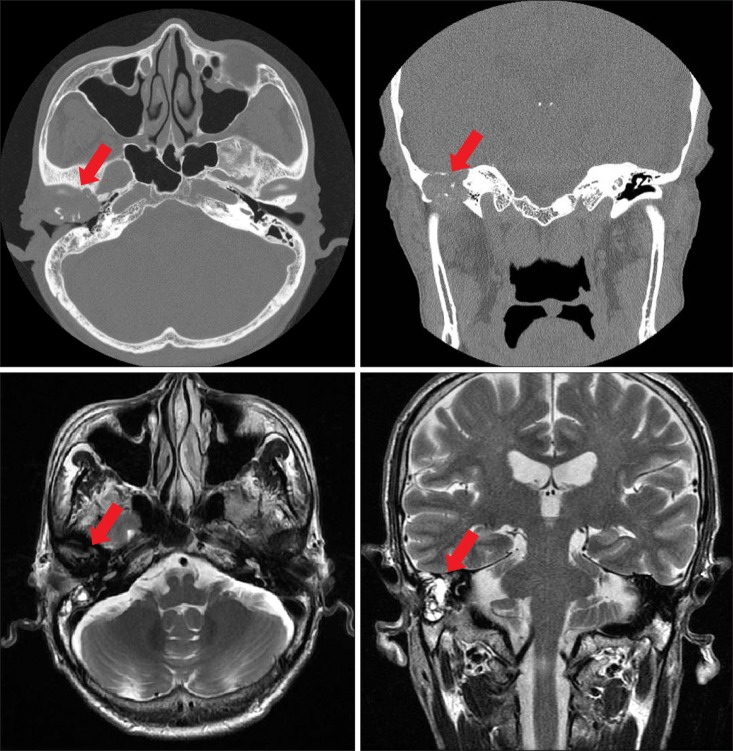
A 69-year-old male complained of a rapidly growing mass on the right mastoid region and otalgia. An immediate incisional biopsy was performed and giant cell tumor was diagnosed. The patient had no medical treatment history or systemic disease. The tumor invaded the right temporal bone and cranial base but there was no invasion of the mandibular condyle noted on computed tomography and magnetic resonance imaging.(Fig. 1) Positron emission tomography revealed no neck lymph node invasion or distant metastasis.
During surgery, a lateral facial approach was used. Tumor tissue on the external auditory canal, temporal bone, and skull base was removed. The mandibular condyle, which had no tumor invasion, was also removed with a wide prophylactic excision due to the aggressive behavior of this tumor. The dura mater was exposed during tumor mass excision. Hemostat material (Surgicel; Johnson & Johnson, Piscataway, NJ, USA) and a hypotensive diuretic agent (Mannitol; CJ Healthcare, Seoul, Korea) were used for bleeding control. No CSF leakage was noticed.
A 3.5×3.0 cm piece of ipsilateral pedicled monocortical parietal bone was harvested (Fig. 2), placed beneath the dura mater, and fixed with 2 mini plates (Jaeil Medical Corp., Seoul, Korea) 4 & 6-hole to reconstruct the infratemporal fossa. Condylectomy was performed at the sigmoid notch level, and the ipsilateral posterior temporal muscle was split into a temporomandibular joint (TMJ) and sutured to the retrodiscal tissue.
The ipsilateral fourth rib was harvested. The internal mammary artery and vein were identified.(Fig. 3) The chondral part of the rib was trimmed to mimic the anatomic appearance of a mandibular condyle head. Microvascular anastomosis was performed to link the internal mammary artery to the facial artery and the internal mammary vein to the external jugular vein.
The harvested rib bone was attached to the lateral side of the mandible and fixed with 3 lag screws (Jaeil Medical Corp., Seoul, Korea) at -15, 16, and 20 mm bicortically. Intermaxillary fixation was performed with 8 intermaxillary fixation (IMF) screw (Jaeil Medical Corp.) and 018 stainless steel boxing wire.
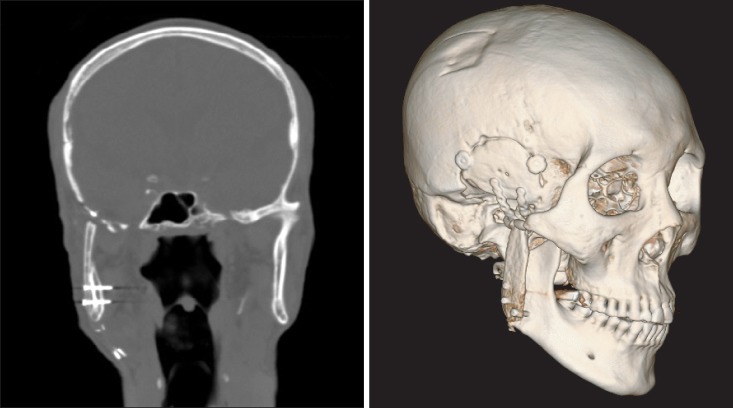
The IMF boxing wire was removed 4 weeks after surgery, when physical training was initiated for another 4 weeks. Maximal mouth opening was 15 mm (between the upper and lower incisor edge), the occlusion was stable, and no mandible deflection was noticed during mouth opening. Ten months after surgery, maximal mouth opening was 33 mm with mild deflection to the right side and stable occlusion. A three-dimensional computed tomography showed no remarkable bone resorption on the costochondral graft site.(Fig. 4)
Go to : 
Reconstruction of the mandibular condyle, disc, and temporal fossa is important. This process is classified into 2 categories-autogenous TMJ reconstruction and prosthetic TMJ reconstruction.
There are many methods for autogenous TMJ reconstruction, including deep circumflex iliac artery free flap, second meta-tarsal free flap, sterno-clavicular free flap, and costochondral free flap. In 1975, Rose et al.4 reported a pedicled vascularized rib graft fused to the posterior surface of the kyphotic spine for reinforcement. In 1989, Poole5 first reported treatment of hemifacial microsomia in children using vascularized free costochondral grafts. This method is now popular for maxillofacial reconstruction. We reconstructed the mandibular condyle with the ipsilateral fourth costochondral free flap because it is anatomically and histologically similar to the original TMJ6.
Different mechanical properties show different prognosis. The temporal fossa consists of a thin cortical layer that cannot resist three stress of mastication. Titanium or alloy can be used to reconstruct the mandibular condyle and fossa because they are non-resorbable and can resist the stress of mastication.
Titanium alloy could have been used to reconstruct a temporal fossa for stable occlusion with minimal post-op change and low risk of ankylosis. However, the high cost of alloplastic materials limited this surgical plan.
Calvarial bone is membranous, thicker than temporal bone, and more resistant to bone resorption. For these reasons, it is considered an ideal autogenous bone for reconstructing the temporal fossa7.
Some degree of TMJ ankylosis is reported regardless of if autogenous or prosthetic materials are used6. More TMJ ankylosis is reported in growing patients than adult patients, and most patients do not need disc reconstruction after disc resection6. There is no reported difference in prognosis regarding the use of abdominal fat, full-thickness skin, temporalis muscle, or buccal fat pad grafts6,8,9,10.
So far, the patient shows good healing and maximal mouth opening of 33 mm with mild deflection to the right side. We hope this procedure can be widely used for other reconstruction surgeries on the head and neck area.
Go to : 
References
1. Speculand B. The origin of the temporalis muscle flap. Br J Oral Maxillofac Surg. 1992; 30:390–392. PMID: 1450163.

2. Driemel O, Braun S, Müller-Richter UD, Behr M, Reichert TE, Kunkel M, et al. Historical development of alloplastic temporomandibular joint replacement after 1945 and state of the art. Int J Oral Maxillofac Surg. 2009; 38:909–920. PMID: 19464145.

3. Westermark A, Hedén P, Aagaard E, Cornelius CP. The use of TMJ Concepts prostheses to reconstruct patients with major temporomandibular joint and mandibular defects. Int J Oral Maxillofac Surg. 2011; 40:487–496. PMID: 21273046.

4. Rose GK, Owen R, Sanderson JM. Transposition of rib with blood supply for the stabilisation of a spinal kyphosis. J Bone Joint Surg Br. 1975; 57:112.
6. Bayat M, Badri A, Moharamnejad N. Treatment of temporomandibular joint ankylosis: gap and interpositional arthroplasty with temporalis muscle flap. Oral Maxillofac Surg. 2009; 13:207–212. PMID: 19806372.

7. Hopper RA, Zhang JR, Fourasier VL, Morova-Protzner I, Protzner KF, Pang CY, et al. Effect of isolation of periosteum and dura on the healing of rabbit calvarial inlay bone grafts. Plast Reconstr Surg. 2001; 107:454–462. PMID: 11214061.

8. Chossegros C, Guyot L, Cheynet F, Blanc JL, Cannoni P. Full-thickness skin graft interposition after temporomandibular joint ankylosis surgery. A study of 31 cases. Int J Oral Maxillofac Surg. 1999; 28:330–334. PMID: 10535529.
9. Gaba S, Sharma RK, Rattan V, Khandelwal N. The long-term fate of pedicled buccal pad fat used for interpositional arthroplasty in TMJ ankylosis. J Plast Reconstr Aesthet Surg. 2012; 65:1468–1473. PMID: 22695714.

10. Mercuri LG, Ali FA, Woolson R. Outcomes of total alloplastic replacement with periarticular autogenous fat grafting for management of reankylosis of the temporomandibular joint. J Oral Maxillofac Surg. 2008; 66:1794–1803. PMID: 18718385.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download