Abstract
Objectives
The aim of this study is to report the results of extracorporeal fixation in patients with mandibular condylar fractures and compare them with the clinical results of conservative treatment.
Materials and Methods
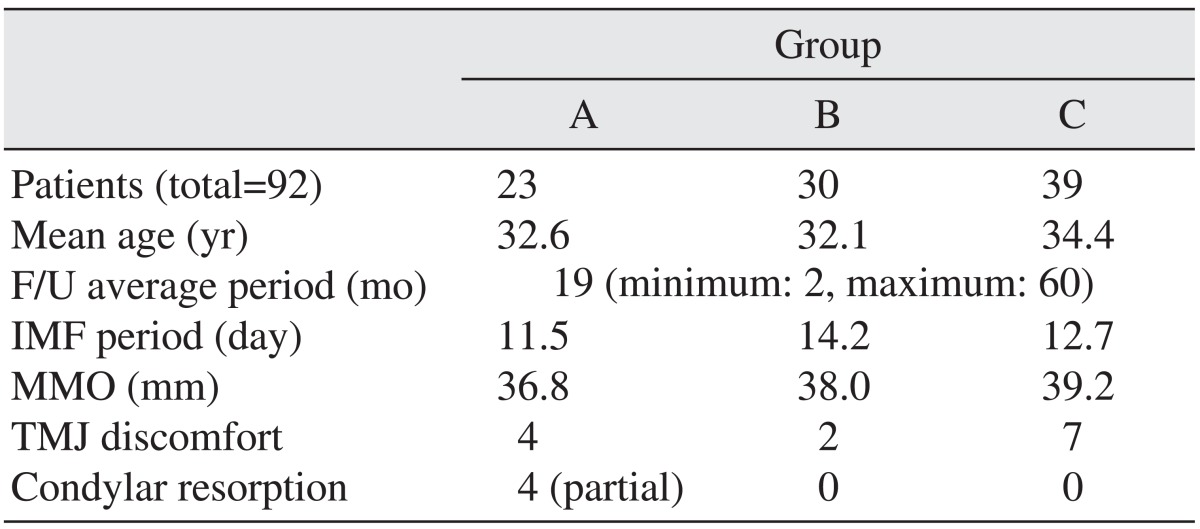
The medical records of 92 patients (73 male [M] : 19 female [F], age 13-69 years, mean 33.1 years) treated for condylar fractures at the Department of Oral and Maxillofacial Surgery in Sun Dental Hospital (Daejeon, Korea) from 2007 to 2012 were reviewed. Patients were divided into three groups: group A (23 patients; M : F=18 : 5, age 21-69 years, mean 32.6 years), treated with extracorporeal fixation; group B (30 patients; M : F=24 : 6, age 16-57 years, mean 21.1 years), treated by conventional open reduction; and group C (39 patients; M : F=31 : 8, age 16-63 years, mean 34.4 years), treated with the conservative method ('closed' reduction). Clinical and radiographic findings were evaluated and analyzed statistically.
Results
Occurrence of postoperative condylar resorption correlated with certain locations and types of fracture. In this study, patients in group A (treated with extracorporeal fixation) did not demonstrate significant postoperative complications such as malocclusion, mandibular hypomobility, temporomandibular disorder, or complete resorption of condyle fragments.
Conclusion
In superiorly located mandibular condyle fractures, exact reconstruction of condylar structure with the conventional open reduction technique can be difficult due to the limited surgical and visual fields. In such cases, extracorporeal fixation of the condyle using vertical ramus osteotomy may be a better choice of treatment because it results in anatomically accurate reconstruction and low risk of complications.
Condylar fractures account for 25%-35% of all mandibular fractures1. Mandibular condyles are anatomically susceptible to fractures because external force tends to focus on the region2. Such fractures cause occlusal dysfunction, temporomandibular joint (TMJ) dysfunction, mandibular movement dysfunction, and facial deformities; therefore proper treatment of condylar fractures is essential in preventing such problems.
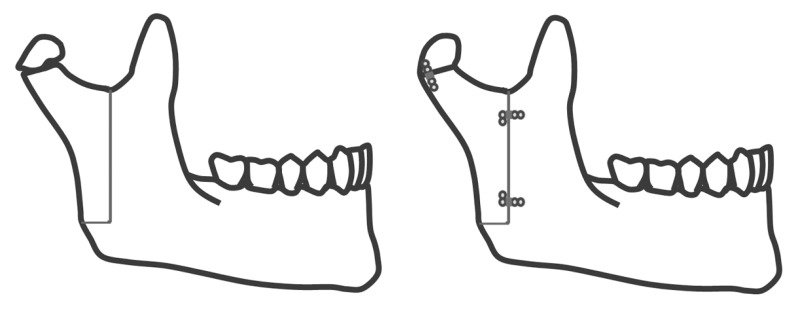
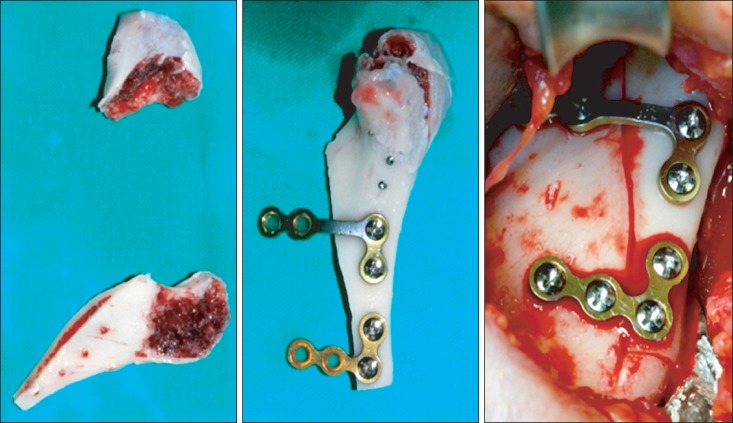
Treatment modalities are divided into two broad categories: conservative treatment and open reduction. Treatment choice depends heavily on the surgeon's preference and the selection criteria are still under debate. Those in favor of open reduction stress the importance of anatomical reconstruction and early recovery of mandibular function3,4,5. In 1983, Zide and Kent6 proposed guidelines for absolute and relative indications for open reduction. However in cases of superiorly positioned fractures with antero-medial displacement of condyle fragments, the standard approach can be difficult. Many studies report difficulty in access, visualization, fixation, and the dangers of harming nearby structures, such as the parotid gland or facial nerve7. Extracorporeal fixation utilizing vertical ramus osteotomy, first performed in 1981, could be a method to resolve these problems8.(Figs. 1, 2) Since then, a number of studies on extracorporeal fixation have been published9,10,11.
This study aims to compare and analyze mandibular condyle fracture patients treated with different modalities in order to assess the clinical application of extracorporeal fixation.
Among patients who visited at the Department of Oral and Maxillofacial Surgery in Sun Dental Hospital (Daejeon, Korea) for mandibular condyle fracture between January 2007 and September 2012, 92 patients (73 males and 19 females, 33.1±13.3 years of age) who had follow-up data available (minimum 2 months, maximum 60 months, average 19 months) were selected. The patients were divided into 3 groups: group A, treated by extracorporeal fixation (n=23, 18 males and 5 females); group B, treated by standard open reduction (n=30, 24 males and 6 females); and group C, treated with intermaxillary fixation only (n=39, 31 males and 8 females). Clinical and radiographic exams were performed on all of the selected patients. Of the 92 patients, 11 had bilateral condylar fractures. Seven of the bilateral condylar fracture patients were treated with conventional open reduction because of favorable fracture location and/or non-displaced fracture fragments. The other 4 patients were treated with extracorporeal fixation because of high fracture location and/or significant displacement of fracture fragments.
The inclusion criteria for open reduction are as follows: 1) inability to achieve occlusion with closed reduction, 2) invasion of the joint space by a foreign body or fractured bony segment, 3) decreased maximum mouth opening (MMO, under 30 mm) with or without mechanical locking, 4) severely displaced condylar fracture with disarticulation of the condyle from the glenoid fossa, and 5) loss of vertical dimension due to bilateral condylar fracture.
In some cases, conventional open reduction was converted to extracorporeal reduction during the procedure.
Patient treatment data such as surgical method, period of intermaxillary fixation, maximal mouth opening, and occurrence of TMJ disorder were collected from medical records. TMJ pain upon mandibular function was assessed through patient interviews.
Preoperative, immediately postoperative, and follow-up panoramic X-rays were used to compare fracture sites and contralateral normal sites. A line was drawn from the superior-most point of the condylar head 'A' bisecting the condylar neck. From this line, a second perpendicular line to the inferior-most point of the mandibular notch 'B' was drawn, and the distance between the intersection point 'C' and 'A' were measured.(Fig. 3) This value was used to describe the amount of condylar head resorption on the fractured side, which was graded as severe (>2/3 of the normal condylar head), moderate (1/3-2/3), or mild (<1/3). Radiographic analysis was performed using ViewRex (Techheim Co., Ltd., Seongnam, Korea) software.
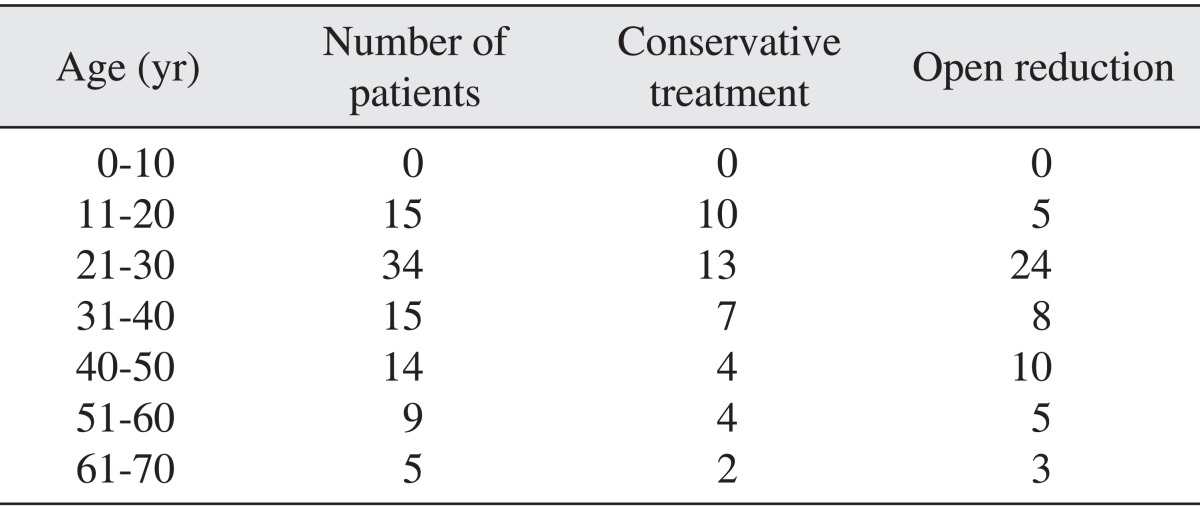
Conservative treatment was preferred for patients under 20 years. Table 1 shows the distribution of treatment choices according to patient age.
Conservative treatment was preferred for condylar head and condylar neck fractures. Extracorporeal fixation was used in condylar head and condylar neck fractures when medially dislocated fragments caused mechanical locking of the mandible. In condylar base fractures, the more inferior the position of the fracture and the further the fragment displacement, the more conventional open reduction was preferred. Condylar fractures were classified according to Lindahl's classification3.
The average postoperative intermaxillary fixation period (group A) was 11.5 days, while the average fixation periods for open reduction patients (group B) and conservative treatment patients (group C) were 14.2 and 12.7 days, respectively.
Group A, B, and C patients had an average MMO of 36.8 mm, 38.0 mm, and 39.2 mm, respectively. Two patients in group A had a limited MMO of less than 30 mm.
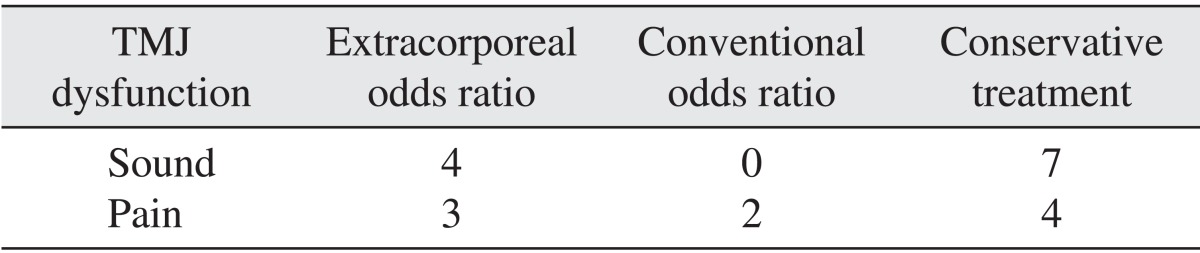
In group A, 4 of the 23 patients reported TMJ click, and 3 complained of pain along with click. None of the group B patients had TMJ click postoperatively, but 2 complained of pain. In group C, 7 of the 39 patients complained of TMJ click and 3 also complained of pain.(Table 2)
In group A, 4 of the 23 patients exhibited moderate resorption (1/3-2/3) of the treated condylar head, and 3 of these 4 patients were advanced in age.(Fig. 4) The remaining 19 patients showed no resorption.(Fig. 5) There was a correlation between age and condylar resorption. Comminuted fractures demonstrated significantly higher condylar resorption compared with simple fractures (P=0.001). There were no significant differences between patients who had a short intermaxillary fixation (IMF) period (<2 weeks) and patients who had a long IMF period (≥2 weeks) (P=0.421). Condylar head fractures did not exhibit significantly higher condylar resorption than fractures in other locations (P=0.735). No group B or C patients demonstrated resorption of the condylar head. All results are shown in Table 3.
While conservative treatment was preferred in younger patients and those with smaller fragments or less fragment dislocation, open reduction was preferred in cases involving larger fragments and greater fragment displacement. MMO and lateral excursion movement increased in the following order: group A < group B < group C. However, since extracorporeal fixation was used in patients with larger fracture fragments and greater displacements, direct comparison of surgery outcomes has little significance. TMJ dysfunctions, such as click and pain, were not correlated with specific procedures. According to radiographic analysis, 4 patients in group A showed moderate condylar head resorption (1/3-2/3 of the condylar head). Condylar head resorption was not observed in patients in group B or C.
Mandibular condyle fractures are classified as intracapsular, extracapsular, or subcondylar according to the vertical location of fracture, and as undeviated, deviated, or dislocated according to the location of fractured fragments. Such classifications play an important role in treatment planning.
Numerous studies have evaluated the selection criteria for open reduction and conservative treatment of condylar fracture12,13,14. According to Eckelt's study15 comparing open reduction and conservative treatment, open reduction patients treated with interfragmentary screw (lag screw) fixation had better outcomes than those treated conservatively. Open reduction should always be considered, unless condylar fracture is incomplete or fragments are not displaced, as it allows for anatomical reconstruction and early functional recovery.
Zide and Kent6 reported that condylar displacement into the middle cranial fossa, an inability to reconstruct proper occlusion, and lateral luxation of the condylar head are absolute indications for open reduction. However, many clinicians and surgeons still seem to prefer conservative treatment. This is most likely due to the difficulty accessing and visualizing fracture sites using the conventional intraoral approach, and the risks the extraoral approach entails, such as harming critical anatomical structures (e.g., the facial nerve or intermaxillary artery). Recent advancements in fixation materials, endoscope technology, and surgical tools such as right-angle drills and drivers have made intraoral access and visualization more convenient, allowing for less invasive surgical procedures. Along with such technological advancements, indications for open reduction have grown broader than before.
Reduction of condylar fracture is more challenging when fractures are superiorly located and fragments are displaced. Moreover, in the case of unfavorable fractures, the medial pterygoid muscle pulls the fractured fragment of the condylar head antero-medially. According to Mikkonen et al.11, reduction of a medially displaced condyle fragment is very difficult using the submandibular approach, and detachment of the condylar head is sometimes required for satisfactory repositioning of this fragment because the lateral fragment can obstruct the surgeon's view and manipulation of the displaced medial fragment.
For treatment of superiorly located condylar fractures with medially displaced fragments, Nam8 introduced 'Nam's method', which includes vertical ramus osteotomy, extraoral reduction and fixation of the fractured condyle to the osteotomy fragment, and re-fixation of the ramus. This technique allows for anatomically accurate reduction of fragments. However, this extracorporeal fixation procedure requires detachment of all soft tissue from the medial fragment, including the blood supply, and the resulting complications are a major concern for many clinicians and oral surgeons.
Bell and Kennedy16 performed vertical ramus osteotomy on monkeys, detached all soft tissue from the medial fragment, and re-fixated the osteotomy fragment to the mandible. Resorption and deposition of bone tissue with formation of a new functional condylar head were observed. The newly formed condylar head, however, was composed of histologically abnormal tissue.
Daniels et al.17 performed free bone grafts and reported resulting histological changes.
Boyne9 reported significant condylar resorption in patients treated with extracorporeal fixation. In their study, condylar resorption occurred within the first 2 years of surgery and then remained stable for up to 15 years. Changes in occlusion were not observed9.
Mikkonen et al.11 published a follow-up study involving 9 male condylar fracture patients treated with extracorporeal fixation, and reported shortening and deformation of the affected condyles; however, nearly complete TMJ function was observed without any permanent complications.
In 2009, Gupta and Sahoo18 reported a 2-11 years follow-up study including 18 condylar fracture patients treated with extracorporeal fixation who experienced satisfactory occlusal stability and functional recovery. One of the 18 patients showed complete resorption of both condylar fragments, but recovery of occlusion and mandibular movement were satisfactory.
Davis et al.19 reported a success rate of 70% in a study involving 11 free graft procedures on 10 condylar fracture patients. Three patients experienced condylar resorption within 9 months.
In this study, 4 of 23 patients treated with extracorporeal fixation exhibited moderate condylar resorption within 6 months, but stabilized after that. All 4 cases involved comminuted fractures with medially displaced fragments, thus making rigid fixation using miniplates difficult.
Three patients with condylar resorption also had a short IMF period, ranging from 6 to 9 days.
In 2012, Adeyemi et al.20 reported earlier satisfactory healing in the patients with a long IMF period (4 to 6 weeks).
Condylar resorption is likely due to avascular necrosis related to detachment of soft tissue from the medial fragment medial fragment. While many studies on extracorporeal fixation report histologic changes, postoperative histologic analysis was not performed in this study because histologic samples were not attained from patients. Some studies reported mandibular dysfunction and TMJ disorder after the extraoral fixation method was used. Detachment of the TMJ capsule is the suspected cause of loss of function of TMJ ligaments and medial pterygoid muscle fibers in these cases. In spite of the moderate condylar resorption shown in some of the patients in the present study, there were no subjective complaints of TMJ pain or mandibular dysfunction. Further study on the fate of detached ligaments and medial pterygoid muscles is under way.
In all extraoral approach procedures, scar formation is of great interest to both surgeons and patients. There were no complaints related to scar formation in this study. This is likely due to the surgeon's esthetic considerations in choosing an appropriate approach site, meticulous procedure, and the use of medication to prevent scar tissue formation.
There is always the risk of facial nerve damage from extraoral approaches. While the location of facial nerve branches varies from patient to patient, knowledge of general anatomy and statistical data on the distribution of the facial nerve21, along with meticulous operative technique, should help prevent facial nerve-related complications. In this study, 3 patients showed signs of facial nerve weakness, but all of them recovered within 3 months of surgery.
In this study, TMJ ankylosis or complete resorption of the condyle did not occur after extracorporeal fixation. Therefore, if conventional open reduction and fixation of condylar fracture is difficult, extracorporeal fixation should be considered as an alternative treatment. Surgeons should also consider predictors of condylar resorption such as age and comminuted fracture when selecting appropriate treatment.
References
1. Ellis E 3rd, Moos KF, el-Attar A. Ten years of mandibular fractures: an analysis of 2,137 cases. Oral Surg Oral Med Oral Pathol. 1985; 59:120–129. PMID: 3856795.

2. da Fonseca GD. Experimental study on fractures of the mandibular condylar process (mandibular condylar process fractures). Int J Oral Surg. 1974; 3:89–101. PMID: 4209422.

3. Lindahl L. Condylar fractures of the mandible. I. Classification and relation to age, occlusion, and concomitant injuries of teeth and teeth-supporting structures, and fractures of the mandibular body. Int J Oral Surg. 1977; 6:12–21. PMID: 402318.
4. Ellis E 3rd, Throckmorton G. Facial symmetry after closed and open treatment of fractures of the mandibular condylar process. J Oral Maxillofac Surg. 2000; 58:719–728. PMID: 10883686.

5. Baker AW, McMahon J, Moos KF. Current consensus on the management of fractures of the mandibular condyle. A method by questionnaire. Int J Oral Maxillofac Surg. 1998; 27:258–266. PMID: 9698171.
6. Zide MF, Kent JN. Indications for open reduction of mandibular condyle fractures. J Oral Maxillofac Surg. 1983; 41:89–98. PMID: 6571887.

7. Raveh J, Vuillemin T, Lädrach K. Open reduction of the dislocated, fractured condylar process: indications and surgical procedures. J Oral Maxillofac Surg. 1989; 47:120–127. PMID: 2913244.

8. Nam IW. The condylar head and upper condylar neck fractures treated by Nam's method(III). J Korean Acad Oral Surg. 1981; 7:81–90.
9. Boyne PJ. Free grafting of traumatically displaced or resected mandibular condyles. J Oral Maxillofac Surg. 1989; 47:228–232. PMID: 2921657.

10. Ellis E 3rd, Reynolds ST, Park HS. A method to rigidly fix high condylar fractures. Oral Surg Oral Med Oral Pathol. 1989; 68:369–374. PMID: 2797732.

11. Mikkonen P, Lindqvist C, Pihakari A, Iizuka T, Paukku P. Osteotomy-osteosynthesis in displaced condylar fractures. Int J Oral Maxillofac Surg. 1989; 18:267–270. PMID: 2509578.
12. Brandt MT, Haug RH. Open versus closed reduction of adult mandibular condyle fractures: a review of the literature regarding the evolution of current thoughts on management. J Oral Maxillofac Surg. 2003; 61:1324–1332. PMID: 14613090.

13. Hidding J, Wolf R, Pingel D. Surgical versus non-surgical treatment of fractures of the articular process of the mandible. J Craniomaxillofac Surg. 1992; 20:345–347. PMID: 1464684.

14. Ellis E 3rd. Method to determine when open treatment of condylar process fractures is not necessary. J Oral Maxillofac Surg. 2009; 67:1685–1690. PMID: 19615583.

15. Eckelt U. Tension bolt osteosynthesis for fractures of the mandibular condyle. Dtsch Z Mund Kiefer Gesichtschir. 1991; 15:51–57. PMID: 1814666.
16. Bell WH, Kennedy JW 3rd. Biological basis for vertical ramus osteotomies--a study of bone healing and revascularization in adult rhesus monkeys. J Oral Surg. 1976; 34:215–224. PMID: 815526.
17. Daniels S, Ellis E 3rd, Carlson DS. Histologic analysis of costochondral and sternoclavicular grafts in the TMJ of the juvenile monkey. J Oral Maxillofac Surg. 1987; 45:675–683. PMID: 3302188.

18. Gupta MV, Sahoo CNK. Extracorporeal fixation of displaced mandibular condylar fracture: viable option. Med J Armed Forces India. 2009; 65:229–231.
19. Davis BR, Powell JE, Morrison AD. Free-grafting of mandibular condyle fractures: clinical outcomes in 10 consecutive patients. Int J Oral Maxillofac Surg. 2005; 34:871–876. PMID: 15955668.

20. Adeyemi MF, Adeyemo WL, Ogunlewe MO, Ladeinde AL. Is healing outcome of 2 weeks intermaxillary fixation different from that of 4 to 6 weeks intermaxillary fixation in the treatment of mandibular fractures. J Oral Maxillofac Surg. 2012; 70:1896–1902. PMID: 22793957.

21. Greene MW, Hackney FL, Van Sickels JE. Arthroscopy of the temporomandibular joint: an anatomic perspective. J Oral Maxillofac Surg. 1989; 47:386–389. PMID: 2647939.

Fig. 3
Measurement technique for condylar resorption. (A: superior point of condyle, B: inferior point sigmoid notch, C: cross point)
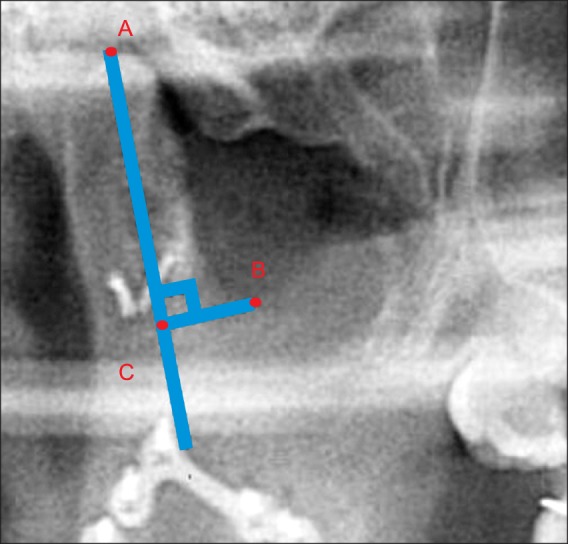
Fig. 4
Moderate resorption of the condyle after extracorporeal fixation. A. A 71-year-old female patient who was expected to have a lower turnover rate. B. A 50-year-old male patient comminuted fracture. C. A 44-year-old male patient fixed with wiring.

Fig. 5
No resorption of the condyle after extracorporeal fixation. A. Preopera-tive panoramic X-ray. A 30-year-old male patient with bilateral condylar head fractures. B. Preoperative computed tomography. C. Postoperative panoramic X-ray. D. Panoramic X-ray after 5 years. E. Clinical photo showing a maximum mouth opening of 38 mm without deviation.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download