Abstract
Objectives
We compared resorbable plates with titanium plates for treatment of combined mandibular angle and symphyseal fractures.
Materials and Methods
Patients with mandibular angle and symphysis fractures were divided into two groups. The control (T) group received titanium plates while the experimental (R) group received resorbable plates. All procedures were carried out under general anesthesia using standard surgical techniques. We compared the frequency of wound dehiscence, development of infection, malocclusion, malunion, screw breakage, and any other technical difficulties between the two groups.
Results
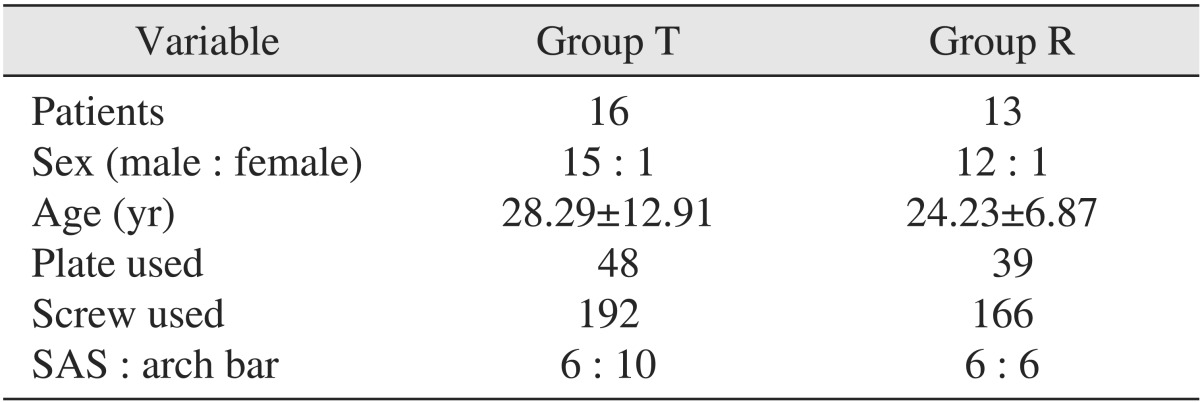
Thirteen patients were included in the R group, where 39 resorbable plates were applied. The T group consisted of 16 patients who received 48 titanium plates. The mean age in the R and T groups was 28.29 and 24.23 years, respectively. Primary healing of the fractured mandible was obtained in all patients in both groups. Postoperative complications were minor and transient. Moreover, there were no significant differences in the rates of various complications between the two groups. Breakage of 3 screws during the perioperative period was seen in the R group, while no screws or plates were broken in the T group.
Mandible fractures are very common injuries to the facial skeleton1,2. Titanium plates have been used for over two decades to achieve internal rigid fixation of mandibular fractures. Many advantages such as bio-compatibility, rigidity, ease of application, and few reported complications have achieved reliable results3. Titanium plates, however, may require additional surgery for removal4.
One advantage of a resorbable plating system over a conventional titanium plating system is that resorbable plates do not require subsequent removal, and thus a second surgery is not needed5.
However, they have less strength than metallic plates6. Unlike titanium plating systems, resorbable plating systems have not been used on a large scale for the fixation of mandibular fractures.
Although studies have evaluated the efficacy of resorbable plating on isolated mandibular angle and symphysis fractures7,8,9, no studies have specifically evaluated the effectiveness of a resorbable plating system in the treatment of combined angle and symphysis fractures.
The purpose of this study was to compare the resorbable plating system with the conventional titanium plating system for treatment of combined fractures in the mandibular angle and symphysis in terms of fracture union, restoration of function, frequency of complications, and specific technical challenges.
This study was conducted at the oral and maxillofacial surgery department of Gachon University Gil Medical Center, Incheon between January 2011 and December 2012. Based on the retrospective observational nature of the study and the operaexclusion of private personal information of protected health information from the data set, this study was exempt from institutional review board's review.
Patients with combined fractures of the mandibular angle and symphysis were included, while patients with contraindications to general anesthesia, comminuted fractures, metabolic bone disorders, or pathologic fractures were excluded. The data recorded included patient gender, age, etiology, state of bone union, and various complications.
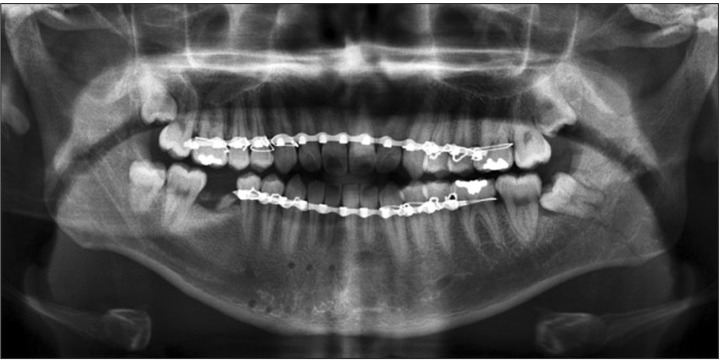
We evaluated radiographs with respect to the condition of the reduction, dislocation, and fracture union. Panoramic X-ray views and computed tomography scans were carried out along with the baseline investigations.
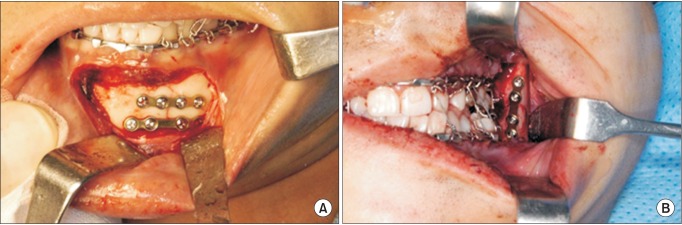
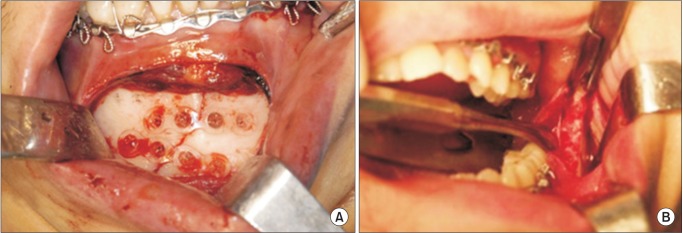
The surgery was carried out by the same surgical team and the operation technique was the same for most patients. After access and identification of the fracture, fixation of the bone segments was obtained through two 4-hole miniplates on the symphysis area and a single 4-hole miniplate on the angle area, as described in Champy et al.10.(Figs. 1, 2) Intermaxillary fixation (IMF) using an arch bar or a skeletal anchorage system was carried out in both groups. After surgery, patients were admitted to the ward facilities for two or three days on average. Follow-up visits were carried out at 1 week, 2 weeks, 1 month, and 3 months after surgery with periodic panoramic X-ray views.(Figs. 3, 4) The occurrence of complications was evaluated by clinical assessment.
The primary variables for this comparative analysis are the union of the fracture and return to normal function. Secondary variables included the incidence of complications such as infection, soft tissue dehiscence, screw fracture rates, operative time, and specific technical challenges.
The data were analyzed using statistical software (SPSS Statistics version 17.0; SPSS Inc., Chicago, IL, USA). A P-value of <0.05 was considered significant.
Thirteen patients were in the experimental (R) group, where 39 resorbable plates (Inion CPS system [Inion Ltd, Tampere, Finland] and Biosorb FX system [Linvatec Biomaterial Ltd, Tampere, Finland]) were utilized.
The control (T) group consisted of 16 patients who received 48 titanium plates (Osteo-fit [GSSEM, Seoul, Korea] and Synthes [Synthes, Paoli, PA, USA]). The overall mean age was 25.78 years. The mean age in the R and T groups was 24.23±6.87 years and 28.29±12.91 years, respectively. Patient demographic data are shown in Table 1.
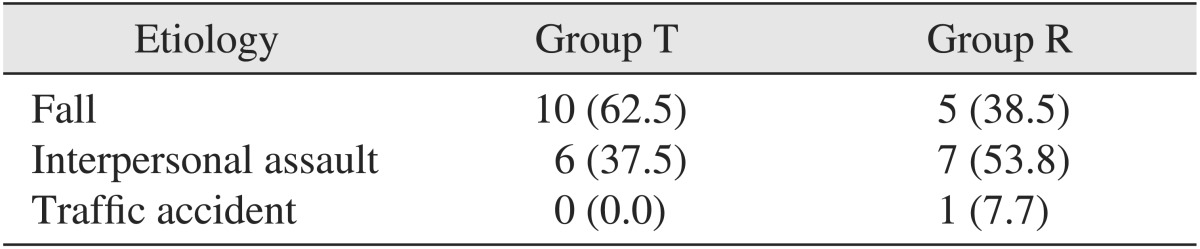
In the T group, falls were the leading mechanism of injury (62.5%), followed by interpersonal assaults (37.5%) and traffic accidents (0%). In the R group, interpersonal assault (53.8%) was the leading mechanism of injury, followed by falls (38.5%) and traffic accidents (7.7%).(Table 2)
Nonunion or malunion were not observed in any fracture site on radiography and clinical assessment in either the R or T group during the follow-up period. Clinical and radiographic evaluation indicated clinical union of all fractures at the 1 month and 3 months follow-up visits. All patients in both groups recovered immediate function such as eating a normal textured diet after the follow-up periods.
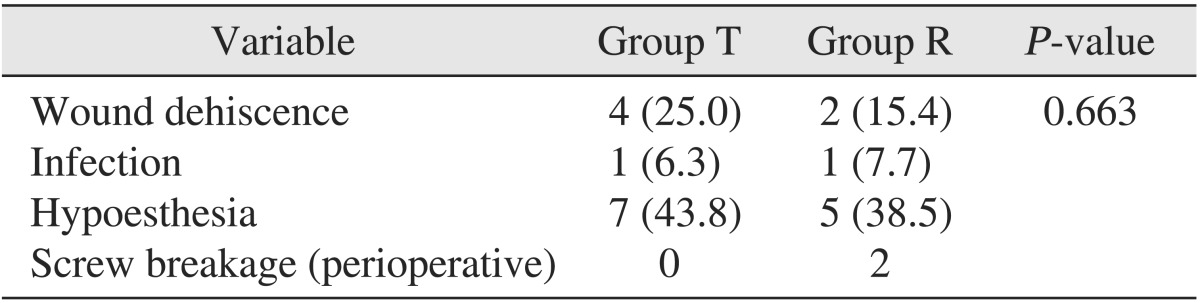
There are 4 cases of wound dehiscence and 1 case of infection in the T group. In R group, there were 2 cases of wound dehiscence and 1 case of infection.(Table 3) The incidence of postoperative complications was 31.2% in the T group and 23.0% in the R group, but this difference was not significant.
All infections occurred within 1 month after surgery, and all affected patients were treated immediately upon presentation. All infected sites responded well to local antibiotic therapy and fully resolved by 1 week after presentation with symptoms and signs of infection. Incision and drainage was not needed, and the fixation plates were not removed. There was no significant association between the stability of fractured segments and the type of plate used (P<0.05).
We observed the breakage of 2 screws during the perioperative period in the R group, while no screws broke in the T group.(Table 3) This represents a 15.4% incidence of specific technical problems. All fractured screws were removed and the previously drilled osteotomy site was re-drilled through the remnant of the previous screw shank. The site was retapped in standard fashion with placement of a new screw.
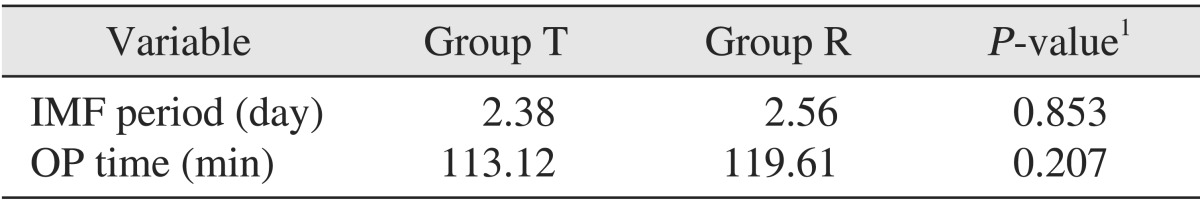
The operation time was 113.12 minutes in the T group and 119.61 minutes in the R group.(Table 4) The IMF period was 2.38 days in the T group and 2.56 days in the R group.(Table 4) More time was spent in the R groups, but there was no significant difference in the operation time and IMF period between the groups.
The treatment goal of mandible fractures allows the patient to have mandibular function and to achieve a normal diet earlier. Rigid fixation of fracture segments in an anatomic bony union is necessary for optimal healing. Rigid internal fixation with metallic materials is a standard technique in use for the last 30 years, and is performed to align bone segments during healing periods3.
The disadvantages of titanium plates include the possibility of hardware removal4, and resorbable plates and screws were developed to avoid this5. Several studies have investigated resorbable plating systems for mandibular fractures. In oral and maxillofacial surgery, biodegradable materials were used in animal studies11 and later in humans for fixation of fractures and in orthognathic surgery12. Resorbable plating systems have allowed the development of a biocompatible, resorbable material suitable for the treatment of facial fractures7,8,9.
In 1997, Bessho et al.13 introduced a poly l-lactic acid (PLLA) miniplate fixation system for fixation of facial fractures and osteotomies. In a sheep model, Kallela et al.14 showed that resorbable plates and screws are biocompatible and have high potential for fixation in oral and maxillofacial surgeries.
Wittwer et al.15 reported that resorbable materials and titanium fixation were not significantly different with respect to fracture healing and postoperative complications. However, other studies16,17 showed that resorbable plating systems do not provide the optimal rigidity to counteract the masticatory forces of the mandibular angle region, resulting in higher rates of delayed union compared to traditional titanium based systems.
Ellis18 reported that patients with double mandibular fractures have different fixation requirements than those with isolated fractures of the mandible. Double fractures require that at least one of the fractures undergoes rigid fixation to decrease the incidence of complications.
In this retrospective study, all cases had a reduction of the symphyseal area with rigid fixation. On the angle area, fixation was performed through the lateral border of the external oblique ridge by Champy's technique10. Our study focused on the rigidity and efficacy of the resorbable plating system with the combined mandibular angle and symphysis area.
We did not observe any mobility problems or severe malocclusion requiring re-operation to remove hardware in either group. Primary bone healing was achieved in 100% of cases. The IMF period for stabilizing bone fragments was slightly longer in the R group (P<0.853). Resorbable plating systems, despite having less strength than metallic plates, provide sufficient strength to support the occlusal force during the postoperative healing period.
Observed postoperative complications included inferior alveolar nerve hypoesthesia, wound dehiscence, infection, and perioperative screw breakage. The postoperative complications were minor and resolved completely after local antibiotic therapy. The average rate of infection in cases of mandibular fractures treated with titanium plates ranges from 5% and 10%19. We observed 4 cases of wound dehiscence and 1 case of infection in the T group. In the R group, there were 2 cases of wound dehiscence and 1 case of infection. Complications occurred in 27.6% of all patients. The incidence of complications was 31.6% in patients with titanium metal plates and 23.1% in those with resorbable plates, but difference was not significant. In this study, all infections occurred within 1 month after surgery, and all affected patients underwent antibiotic therapy.
Incision and drainage were not needed in any patients. The fixation plates were not removed, and the infection resolved within 5 to 7 days after local antibiotic therapy. Wound dehiscence and infections occurred mostly in the vestibule of the symphysis area. Local muscle movement around the symphysis area tends to be a contributing factor.
We observed some technical difficulties regarding the resorbable plates. The resorbable plates were transparent, so it was difficult to distinguish between the plate and screw holes, especially at the mandibular angle area. Care had to be taken while drilling or tapping in order to avoid grinding the screw holes. There were significantly more screw breakages of the head of the screw in the R group. This may have been due to under-tapping of the screw holes or use of excessive torque while tightening. This can be avoided by thorough tapping to the full length of the hole according to the length of the screw. More careful screw tightening can be achieved by using the thumb and index finger instead of using the palm. Use of the thumb and fingers generates more controlled force and can help to reduce the frequency of screw breakage20. When screw breakage occurs, the same holes can be re-drilled and reused with new screws, and plates do not need to be relocated.
There was an increase in operation time for R group patients for two potential reasons. The plates had to be heated and then bent according to the mandible's anatomy, and screw tapping before insertion is technically difficult, especially at the mandibular angle area, which requires extra time. On average, more time was spent in the R group, but there was no significant difference in operation time between the groups. More experience for the surgeons and more careful patient selection may reduce the incidence of screw breakage and decrease operation time.
The resorbable plates which were used in this study were Inion CPS system and Biosorb FX series. The Inion CPS system consisted of an amorphous injection-molded copolymer of L-lactide/D-lactide/trimethylene carbonate. The Biosorb Fx series are made of self-reinforced poly-L/DL lactic acid copolymer in a ratio of 70% L-lactide and 30% D-lactide (SR-PLDLA; Biosorb FX system). This study did not include sufficient cases to compare each commercial resorbable plating system. Further study is needed to compare the efficacy and effectiveness of the each resorbable plating system for the treatment of mandibular fractures. Both resorbable plating systems provided satisfactory stability to enable bone healing during the initial phase. Studies have been published that have evaluated the efficacy of these resorbable plating systems using on the isolated mandible fractures. This study focused on the rigidity and efficacy of the resorbable plating system for treatment of mandible fractures with combined symphysis and angle. The clinical outcome of the resorbable plating systems applied for treatment of combined mandibular symphysis and angle was comparable with outcomes from titanium plating systems. The treatment goals of immobilization, fixation, and stabilization were fulfilled. Resorbable plates can be used as an alternative to titanium plates in combined mandibular angle and symphysis fractures.
References
1. Ellis E 3rd, Moos KF, el-Attar A. Ten years of mandibular fractures: an analysis of 2,137 cases. Oral Surg Oral Med Oral Pathol. 1985; 59:120–129. PMID: 3856795.

2. Haug RH, Prather J, Indresano AT. An epidemiologic survey of facial fractures and concomitant injuries. J Oral Maxillofac Surg. 1990; 48:926–932. PMID: 2395044.

3. Tuovinen V, Nørholt SE, Sindet-Pedersen S, Jensen J. A retrospective analysis of 279 patients with isolated mandibular fractures treated with titanium miniplates. J Oral Maxillofac Surg. 1994; 52:931–935. PMID: 8064456.

4. Kim YK, Yeo HH, Lim SC. Tissue response to titanium plates: a transmitted electron microscopic study. J Oral Maxillofac Surg. 1997; 55:322–326. PMID: 9120693.

5. Suuronen R, Kallela I, Lindqvist C. Bioabsorbable plates and screws: current state of the art in facial fracture repair. J Craniomaxillofac Trauma. 2000; 6:19–27. PMID: 11373737.
6. Leonhardt H, Demmrich A, Mueller A, Mai R, Loukota R, Eckelt U. INION compared with titanium osteosynthesis: a prospective investigation of the treatment of mandibular fractures. Br J Oral Maxillofac Surg. 2008; 46:631–634. PMID: 18597909.

7. Choi EJ, Nam W, Jung YS, Kim KH, Kim HJ. Clinical and radiological comparison between titanium and biodegradable miniplate monocortical osteosynthesis in mandibular angle fractures. J Korean Assoc Oral Maxillofac Surg. 2006; 32:222–225.
8. Jeong JC, Choi SH, Song MS, Jun CH, Kim HM. Clinical study of resorbable plate and screw for treatment of maxillofacial fractures. J Korean Assoc Oral Maxillofac Surg. 2003; 29:438–443.
9. Kim YK, Kim SG. Treatment of mandible fractures using bioabsorbable plates. Plast Reconstr Surg. 2002; 110:25–31. PMID: 12087226.

10. Champy M, Loddé JP, Schmitt R, Jaeger JH, Muster D. Mandibular osteosynthesis by miniature screwed plates via a buccal approach. J Maxillofac Surg. 1978; 6:14–21. PMID: 274501.

11. Bos RR, Rozema FR, Boering G, Nijenhuis AJ, Pennings AJ, Verwey AB. Bio-absorbable plates and screws for internal fixation of mandibular fractures. A study of six dogs. Int J Oral Maxillofac Surg. 1989; 18:365–369. PMID: 2516105.
12. Kim YK, Shim CH, Bae JH, Yun PY. Application of bioabsorbable plates in orthognathic surgery. J Korean Assoc Oral Maxillofac Surg. 2006; 32:60–64.
13. Bessho K, Iizuka T, Murakami K. A bioabsorbable poly-L-lactide miniplate and screw system for osteosynthesis in oral and maxillofacial surgery. J Oral Maxillofac Surg. 1997; 55:941–945. PMID: 9294503.

14. Kallela I, Tulamo RM, Hietanen J, Pohjonen T, Suuronen R, Lindqvist C. Fixation of mandibular body osteotomies using biodegradable amorphous self-reinforced (70L:30DL) polylactide or metal lag screws: an experimental study in sheep. J Craniomaxillofac Surg. 1999; 27:124–133. PMID: 10342151.

15. Wittwer G, Adeyemo WL, Yerit K, Voracek M, Turhani D, Watzinger F, et al. Complications after zygoma fracture fixation: is there a difference between biodegradable materials and how do they compare with titanium osteosynthesis? Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006; 101:419–425. PMID: 16545702.

16. Bayram B, Araz K, Uckan S, Balcik C. Comparison of fixation stability of resorbable versus titanium plate and screws in mandibular angle fractures. J Oral Maxillofac Surg. 2009; 67:1644–1648. PMID: 19615576.

17. Esen A, Ataoğlu H, Gemi L. Comparison of stability of titanium and absorbable plate and screw fixation for mandibular angle fractures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008; 106:806–811. PMID: 18718777.

18. Ellis E 3rd. Open reduction and internal fixation of combined angle and body/symphysis fractures of the mandible: how much fixation is enough? J Oral Maxillofac Surg. 2013; 71:726–733. PMID: 23245520.

19. Fonseca RJ, Walker RV, Betts NJ, et al. Oral and Maxillofacial Trauma. Vol 2. 2nd ed. Philadelphia: WB saunders;1997.
20. Ahmed W, Ali Bukhari SG, Janjua OS, Luqman U, Shah I. Bioresorbable versus titanium plates for mandibular fractures. J Coll Physicians Surg Pak. 2013; 23:480–483. PMID: 23823951.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download