Abstract
Eagle syndrome is a rare condition caused by elongation of the styloid process or calcification of the stylohyoid ligament. Patients with Eagle syndrome typically present with dysphagia, dysphonia, cough, voice changes, otalgia, sore throat, facial pain, foreign body sensation, headache, vertigo, and neck pain. Here we report a case in which the patient initially presented with sore throat, left-sided facial pain, and cough. This case report provides a brief review of the diagnosis and nonsurgical management of this rare syndrome.
Go to : 
Eagle syndrome is a rare clinical condition caused by elongation of the styloid process or by mineralization (ossification or calcification) of the stylohyoid ligament1. The length of the styloid process is normally 2 to 2.5 cm, and elongation beyond 2.5 cm causes Eagle syndrome, which was first defined in 19372,3.
This syndrome has two types, including classic and styloid-carotid syndromes. The classic syndrome, also known as stylalgia, is usually characterized by pharyngeal pain localized to the tonsillar fossa, referred otalgia, and neck pain. It also may be associated with dysphagia, hypersalivation, sensation of a foreign body in the throat, and transient voice changes that are often seen following tonsillectomy4. Styloid-carotid syndrome is characterized by nonspecific symptoms caused by compression of the carotid arteries and sympathetic fibers by the styloid process4. The most common etiology of this syndrome is ossification or calcification of the stylohyoid ligament.
The prevalence of styloid process elongation or stylohyoid ligament mineralization in imaging studies has been reported to be between 19.4% to 52.1% in the general population5,6,7 and in up to 76% of patients with temporomandibular disorder8. However, the incidence of Eagle syndrome in the general population is underestimated since only 6% of those with an elongated styloid process have symptoms9.
Here, we present a case of Eagle syndrome treated with medical therapy.
Go to : 
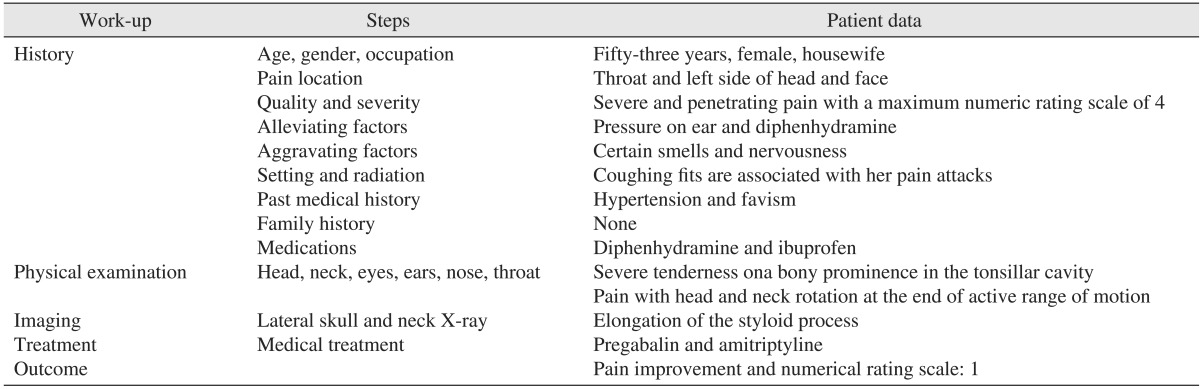
A 53-year-old woman was referred to the pain clinic at Amir Alam Hospital with a complaint of pain in the throat and the left side of the head and face. Her pain began 16 years prior following a root canal of a mandibular tooth on the left side. She at times experienced severe pain attacks lasting approximately 10 minutes with a frequency of 10 times per day, which extended from the external auditory canal to the left side of the throat. Additionally, cough was a trigger for these pain attacks. Certain odors or nervousness were also aggravating factors of her pain, while pressure on the ear and diphenhydramine were mitigating factors. The patient reported her highest and lowest pain intensity as 4 and 2, respectively, according to the numeric rating scale (NRS). The patient had a past medical history significant for hypertension and favism.
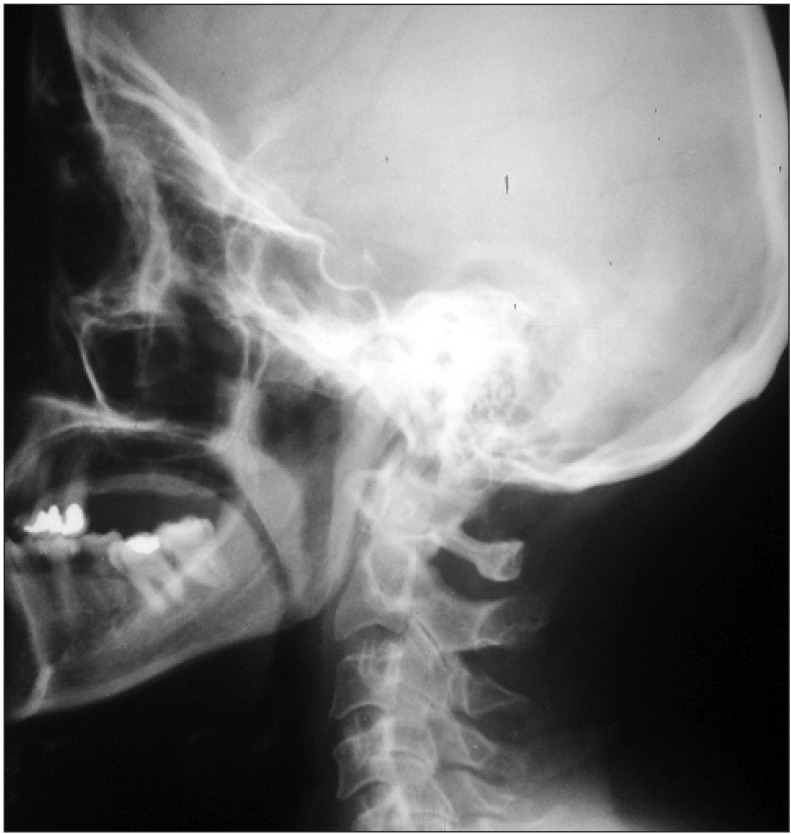
The patient's general health as well as her head and neck were thoroughly examined. Her skull, cranial nerves, eyes, ears, nose, sinuses, thyroid, and dentition were unremarkable. No cervical, axillary, epitrochlear, or inguinal adenopathy was detected. On oral and pharyngeal examination, severe tenderness was present on a bony prominence in the tonsillar cavity. Head and neck rotation was painful at the end of active range of motion. As a result, lateral skull and neck x-rays were taken that showed elongation of the styloid process, thereby confirming the diagnosis of Eagle syndrome.(Fig. 1) Laboratory studies and histopathology were not performed.
Upon diagnosis, treatment with pregabalin (75 mg/day) and amitriptyline (10 mg/day) was initiated. These medications improved the patient's cough and reduced the pain severity by about 50% within 2 months. Three and 6 months after treatment, her pain severity improved by about 80% and her NRS score decreased to one. The patient also experienced occasional pain-free intervals.(Table 1)
Go to : 
In this study, Eagle syndrome was identified in our patient, after which medical therapy was initiated with an appropriate response.
Eagle syndrome may be unilateral or bilateral, although in most cases symptoms are unilateral. According to Moon et al.10, Eagle syndrome and elongation of the stylohyoid ligament is typically a bilateral process, though in our patient this condition was unilateral.
A calcified stylohyoid ligament is found in 4% to 28% of normal population11. There is no direct correlation between the severity of Eagle syndrome and level of calcification12. However, there is a clear relationship between longer lengths of the styloid process and higher pain intensity and severity of Eagle syndrome8.
Pharyngeal pain with radiation to the neck and ears poses a very difficult challenge for interpretation, including a vast number of differential diagnoses13,14,15,16,17.(Table 2) The differential diagnosis for Eagle syndrome includes inflammatory disorders, masses of the pharynx and tongue base, and cranial nerve neuralgia. On the other hand, patients with an elongated styloid process manifest some transient and nonspecific symptoms as well as the severe classic symptoms, which require surgery18. Traumatic fracture of the apophysis, pharyngeal infection and inflammation, rheumatoid disorders of the hyoid bone, inflammation of the muscles attached to the styloid process, osteoarthritis of the cervical vertebrae, pressure on adjacent nerves such as cranial nerve IX and the mandibular branch of the 5th cranial nerve and corda tympani, pathologies of the third molar, and pharyngeal scar following tonsillectomy are other pathologies that could mimic symptoms of Eagle syndrome. Different forms of pharyngeal neuralgia may also result in similar symptoms including laryngeal neuralgia, occipital neuralgia (involving Arnold's nerve), sphenopalatine neuralgia (secondary to sphenoethmoid inflammation), and finally trigeminal neuralgia which may account for sporadic pains with pressure within the auditory canal19. Disorders of the temporomandibular joint constitute another possible diagnosis. In our case, most other differential diagnoses were ruled out according to the history and physical examination findings.
Clinical diagnosis rests upon previous history of trauma or tonsillectomy and palpation of the tonsillar fossa. Radiologic studies such as an orthopantomograph or lateral skull view with the head slightly extended may help to confirm this diagnosis18. A precise history, examination, and imaging studies also contribute greatly to achieving the correct diagnosis.(Table 2) The final diagnosis in our case was confirmed by imaging.
Medical therapy is first-line treatment for Eagle syndrome. Surgery with resection of the elongated styloid process is considered to be definitive treatment, however, surgery may be contraindicated in some cases or patients may decline operative intervention. In these cases, conservative treatment with oral medications may be considered. In cases that do not respond to medical therapies, surgery is indicated. Different medications may be used in medical management of Eagle syndrome based on the respective etiology, including analgesics, anticonvulsants, antidepressants, and local infiltration with steroids or long-acting local anesthetic agents20. In our case, a tricyclic antidepressant (amitriptyline) and an anticonvulsant (pregabalin) were started after diagnosis. Our patient dramatically and persistently responded to conservative treatment after 3 and 6 months of therapy. Nonsurgical treatment of Eagle syndrome with gabapentin, tianeptine, tramadol, acetaminophen, local lidocaine injection and stellate ganglion block has also been reported20. However, to our knowledge, our patient is the first case of Eagle syndrome to be treated with only oral medications, while previous similar cases also utilized a stellate ganglion block2,10,14,15,16,20.
The exact mechanism by which medications achieve symptom relief in patients with Eagle syndrome is not known. The cause of pain in Eagle syndrome is the stimulation of adjacent nerves by the elongated styloid process and secondary induced inflammation. It seems that medications such as anticonvulsants and antidepressants may reduce nerve stimulation and consequently pain intensity by altering the concentration of neurotransmitters, and analgesics such as nonsteroidal antiinflammatory drugs may improve pain by reducing inflammation in adjacent tissues.
In conclusion, lateral skull imaging in cases suspicious for Eagle syndrome is recommended to confirm this diagnosis, and medical therapy should be considered as first-line treatment for this rare condition.
Go to : 
Acknowledgements
The authors would like to thank the Farzan Institute for Research and Technology for technical assistance.
Go to : 
References
1. Balbuena L Jr, Hayes D, Ramirez SG, Johnson R. Eagle's syndrome (elongated styloid process). South Med J. 1997; 90:331–334. PMID: 9076308.

3. Murtagh RD, Caracciolo JT, Fernandez G. CT findings associated with Eagle syndrome. AJNR Am J Neuroradiol. 2001; 22:1401–1402. PMID: 11498437.
4. Soldati AB, Miguelote C, Quero C, Pereira R, Santos R, Soares C. Eagle's syndrome. Arq Neuropsiquiatr. 2013; 71:265–266. PMID: 23588292.

5. More CB, Asrani MK. Evaluation of the styloid process on digital panoramic radiographs. Indian J Radiol Imaging. 2010; 20:261–265. PMID: 21423900.

6. Phulambrikar T, Rajeshwari A, Rao BB, Warhekar A, Reddy P. Incidence of elongated styloid process: a radiographic study. J Indian Acad Oral Med Radiol. 2011; 23:S344–S346.

7. Bagga MB, Kumar CA, Yeluri G. Clinicoradiologic evaluation of styloid process calcification. Imaging Sci Dent. 2012; 42:155–161. PMID: 23071965.

8. de Andrade KM, Rodrigues CA, Watanabe PC, Mazzetto MO. Styloid process elongation and calcification in subjects with tmd: clinical and radiographic aspects. Braz Dent J. 2012; 23:443–450. PMID: 23207864.
9. Ilgüy M, Ilgüy D, Güler N, Bayirli G. Incidence of the type and calcification patterns in patients with elongated styloid process. J Int Med Res. 2005; 33:96–102. PMID: 15651721.

10. Moon CS, Lee BS, Kwon YD, Choi BJ, Lee JW, Lee HW, et al. Eagle's syndrome: a case report. J Korean Assoc Oral Maxillofac Surg. 2014; 40:43–47. PMID: 24627843.

11. Gorlin RJ, Cohen MM, Levin LS. Syndromes of the head and neck. New York: Oxford University Press;1990.
12. Goaz PW, White SC. Oral radiology: principles and interpretation. St. Louis, Missouri: Mosby;1994.
13. Casale M, Rinaldi V, Quattrocchi C, Bressi F, Vincenzi B, Santini D, et al. Atypical chronic head and neck pain: don't forget Eagle's syndrome. Eur Rev Med Pharmacol Sci. 2008; 12:131–133. PMID: 18575165.
14. Gelabert-González M, García-Allut A. Eagle syndrome. An unusual cause of neck pain. Neurocirugia(Astur). 2008; 19:254–256. PMID: 18654725.
15. Chi J, Harkness M. Elongated stylohyoid process: a report of three cases. N Z Dent J. 1999; 95:11–13. PMID: 10208079.
16. Nishihara K, Hanakita J, Kinuta Y, Kondo A, Yamamoto Y, Kishimoto S. Three cases of Eagle's syndrome. No Shinkei Geka. 1986; 14(3 Suppl):441–445. PMID: 3703148.
17. Eversole LR. Clinical outline of oral pathology: diagnosis and treatment. 2nd ed. Philadelphia: Lea and Febiger;1978.
18. Prasad KC, Kamath MP, Reddy KJ, Raju K, Agarwal S. Elongated styloid process (Eagle's syndrome): a clinical study. J Oral Maxillofac Surg. 2002; 60:171–175. PMID: 11815916.

19. Mortellaro C, Biancucci P, Picciolo G, Vercellino V. Eagle's syndrome: importance of a corrected diagnosis and adequate surgical treatment. J Craniofac Surg. 2002; 13:755–758. PMID: 12457088.

20. Han MK, Kim DW, Yang JY. Non surgical treatment of Eagle's syndrome: a case report. Korean J Pain. 2013; 26:169–172. PMID: 23614080.
Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download