Abstract
Implants are typically placed after performing ridge expansion by inserting screws of gradually increasing thickness and good clinical outcomes are often obtained. We placed 11 implants in 6 patients, and one implant failed during osseointegration but it was replaced immediately after removal and successful prosthetic treatments were completed. During these surgeries, buccal cortical plate complete fractures do not occur. Inserting screws for ridge expansion is a successful and predictable technique for implant placement in narrow alveolar bone.
Many cases of implant placement involve insufficient buccolingual width of the edentulous ridge. The methods used to resolve this issue are the following: narrow implant placement, horizontal veneer block bone graft, horizontal guided bone regeneration (GBR), and the ridge splitting procedure1,2,3. Ridge splitting is applied primarily in cases where the bone height is sufficient, but the width is narrow. The purpose of ridge splitting is to widen the alveolar ridge by taking advantage of the elasticity of bones, and it is frequently performed in the anterior maxillomandibular area. This surgery restores the morphology of the lingual side of the alveolar bone and obtains not only aesthetic results, but also a housing effect exerted by the cortical bone of the buccolingual side, which improves the osseointegration of implants by providing an ample supply of blood circulation4. Nevertheless, fracture and separation of the buccolingual bone during surgery are potential risks, so it is crucial to minimize these complications. Methods augmenting the alveolar bone to the buccolingual side are often done because ridge splitting involving the use of an osteotome and mallet can induce greenstick fractures of the buccal cortical bone. In the ridge splitting procedure, discomfort to patients is often substantial because of malleting, and there is a risk of buccolingual bone fracture when excessive force is delivered. Therefore, the present report introduces and evaluates the clinical results of a procedure that expands the ridge in a stepwise technique using screws of gradually increasing width.
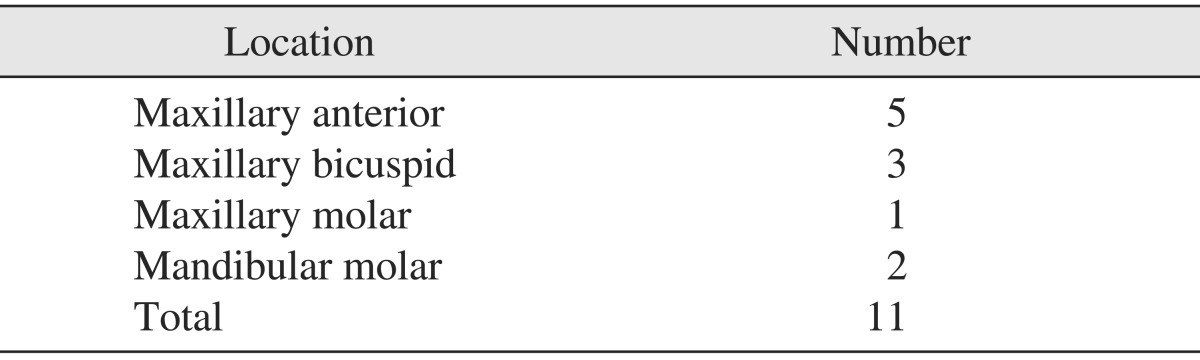
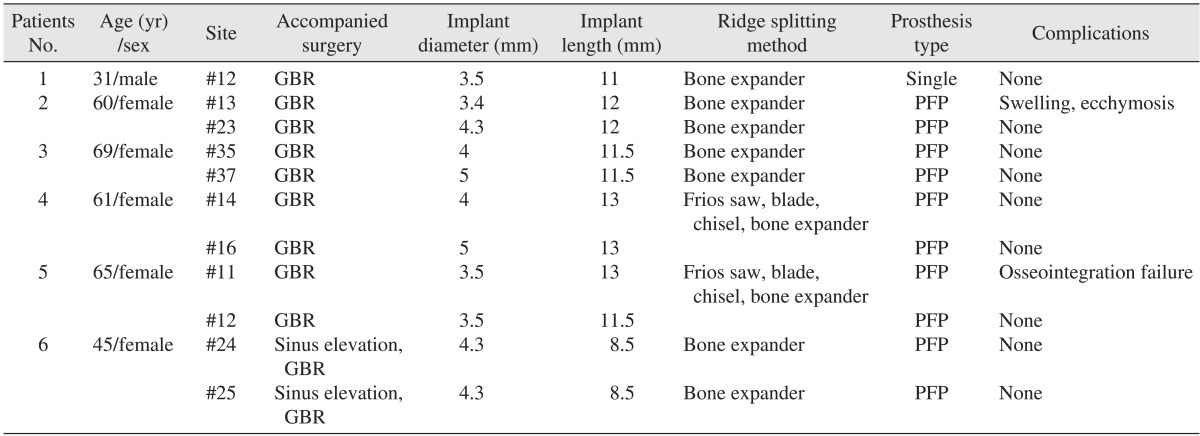
This study was performed after obtaining approval from the institutional review board of the Seoul National University Bundang Hospital (No. B-1007-105-106). In the department of oral and maxillofacial surgery, one oral and maxillofacial surgeon performed ridge expansions from May 2008 to September 2009. The procedure was performed using expanding screws (SplitMaster; Mr. Curette, Seoul, Korea), and implants were placed sequentially or simultaneously in 6 patients (1 male and 5 females). The age of the patients ranged from 31 to 69 years with a mean age of 55.1 years. One patient had osteoporosis, and the rest were generally healthy. The postsurgical follow-up observation period ranged from 24 to 63 months with an average of 44.7 months.
The surgery was performed under local anesthesia. A midcrestal incision was made in the maxillary and mandibular alveolar bone, and the bone was exposed through the creation of a full thickness flap. Initial drillings were performed in the area of implant placement, and the implant was placed at the proper placement depth using a SplitMaster No. 1 expanding screw. Gradually, thicker screws were used relative to the final width and length of the implants. Simultaneous implants were placed with self-tapping and sequential implants were placed with an approximately 3- to 4-month healing period in between. In two cases, a groove was created in the alveolar ridge with Frios saws (Dentsply Implants, Mannheim, Germany) or #15 blades, and alveolar ridge splitting was performed using an osteotome. Then, the implant placement site was expanded to the width of the implant by using expanding screws. In some cases, additional bone graft was performed to prevent resorption of the thin buccal cortical plate. The space between the implants and the bone was filled with graft materials and, if needed, blocking membranes. In one of the ridge expansions, a maxillary lift surgery was performed simultaneously.
A total of 11 implants were placed: 5 in the maxillary anterior and 3 in the maxillary premolar area.(Table 1) Complications during surgery, such as buccal cortical plate complete fracture, did not develop with the exception of severe edema and post-surgical ecchymosis in one case. In that case, osseointegration failure was observed 4 months after the first surgery, so the implant was removed and was replaced immediately. Wound dehiscence developed after implant placement, and the implant was considered a possible etiologic factor. After approximately 8 weeks after replacement, a fixed partial prosthesis was installed. During the follow-up observation period, averaging 44.7 months, all 6 patients maintained normal function without any specific problems.(Table 2)
A 31-year-old male patient with a history of right unilateral cleft lip and palate presented to our clinic with a missing right maxillary lateral incisor and alveolar bone loss. Together with orthodontic therapy, a treatment plan was developed that included a symphysis bone graft, oronasal fistula closure surgery, and implant placement. The first implant surgery was performed after a 6-month healing period following the bone graft. To secure an adequate view, a full thickness flap was created. The bone height was sufficient for implant placement and the buccolingual width was approximately 3 mm. Using SplitMaster expanding screws, a 4-mm ridge expansion was performed; subsequently, an implant that was 3.5 mm in diameter and 11 mm in length was placed. To prevent buccal bone fracture, expanding screws were carefully handled with a hand ratchet. On the buccal side, a 2-mm implant thread was exposed, so GBR with xenogeneic bones (Biocera; Osscotec, Cheonan, Korea) and barrier membranes (Bioarm; ACE Surgical Supply, Brockton, MA, USA) was performed in the exposed area. After a 4-month healing period, the second surgery to maintain the buccal volume was performed through creating a labial pouch and grafting the Biocera. After 3 months of orthodontic treatment for regaining the space of implant prosthesis, a provisional restoration was placed. After the orthodontic treatment was finished (nine months after the implant surgery), the implant was restored with an all-ceramic crown supported by zirconia abutment post.(Figs. 1,2,3,4,5,6)
A 69-year-old female patient without any history of systemic diseases presented to our clinic with a chief complaint of missing several teeth. Under local anesthesia, a full thickness flap lift was performed in the left mandibular implant 235restoration area. Bone height was sufficient for implant placement; the buccolingual width was as narrow as 3 to 4 mm, bone quality was D3, and osteoporosis was suspected. After initial drilling, expansion was performed using SplitMaster expanding screws at the left mandibular 2nd premolar and 2nd molar area; the areas were expanded to 3.8 mm and 4.3 mm, respectively. Two GS II implants (Osstem, Busan, Korea) which were 4mm in diameter, 11.5 mm in length and 5 mm in diameter, 11.5 mm in length were placed. As measured by the Osstell Mentor (Integration Diagnostics, Savedalen, Sweden), the primary stability of the implants in the left mandibular 2nd premolar and 2nd molar was 76 and 77 implant stability quotient (ISQ), respectively. These were relatively good values. Subsequently, a xenogeneic bone graft (Biocera) was performed in the space between the bones and the thin area of the buccal side. The surgery was performed using the one-stage method, and after a healing period of approximately 2 months, the implants were restored with a fixed partial prosthesis.(Figs. 7,8,9,10,11)
Since 1990, it was widely used and referred to in the literature with various terms such as ridge widening, the split crest procedure, and staged ridge splitting5. Generally, this surgery induces a greenstick fracture in the narrow alveolar ridge with an osteotome. The procedure forms an implant bed and facilitates the placement of implants with wide diameter. In addition, bone regeneration is achieved on both sides, so the bone healing capacity is good; therefore, sufficient osseointegration can be achieved with relatively small volumes of bone. Furthermore, a 3-month waiting period is required at minimum for distraction osteogenesis and 6 months is required for GBR in implant placement. On the other hand, after performing ridge splitting, the first placement surgery can be performed on the same day or within the month. It is still controversial as to whether a bone graft is required for the space generated after splitting. In simultaneous implant placements, it is controversial whether bone graft materials improve osseointegration6. It has been reported that in cases with bony gaps smaller than 3 mm, bone graft materials other than collagen sponges are not required7. Also, implants placed in the space between expanded bones are protected from biodynamic external loading. Furthermore, bony compaction effects can occur as a result of the compression of bony trabeculae. Nonetheless, this surgery is a method that uses bone elasticity, so it can only be performed in cases with cancellous bone within the cortical bone on both sides. Therefore the indications of this procedure might be limited when compared with GBR or onlay graft that could be applied in a cancellous bone-deficient area. In cases where the width of the basal bone is too narrow, the primary stability or the slope of edentulous alveolar bone can be worsened and an esthetically poor maxillary prosthesis may be produced. Thus, it is better to select alternate procedures. It has been reported that cases with a residual width of more than 4 mm are ideal for the procedure; in cases with a width of 3 mm or less, other bone graft procedures should be additionally performed, and the implant should be placed after a certain healing period6. Moreover, it has been reported that ridge splitting is a procedure that should be applied primarily to the maxilla, as the outcomes are poor in the mandible due to the abundance of cortical bone7. However, it has also been reported that if the characteristics of the mandible are well understood and slow expansion is performed manually rather than with a mallet, then successful results can be obtained7. Chiapasco et al.8 demonstrated gradual bone expansion of 1 mm per day for 4-5 days using screw-type tools in the mandible. Recently, minimal invasive ridge expansion and screw spreading techniques were reported9. Chan et al.10 reported that the mean increased ridge width was 0.79 mm in a cadaver study on the ridge width gain through the use of screws. In this study, even in the mandibular molar area, the bone width was expanded to a maximum of 4.3 mm using expanding screws and simultaneously placing implants. Even though some of case reports reported the occurrence of cortical bone greenstick fracture after surgery, the separation of bone fragment caused by the occurrence of complete fracture was not reported. One year after functional loading, good results without the gingival recession or alveolar bone resorption were obtained. In a case with poor D4 bone quality, the compaction effect of the bony trabeculae using screw-type tools was observed and resulted in effective primary stability of the implants.
In several reports, a 97.0%-97.6% success rate of ridge splitting was reported; however, cortical bone fracture, resorption of the alveolar ridge, nerve injury, and other complications may occur11,12. Buccal cortical bones are fractured in many cases, particularly when ridge splitting is performed in the mandible with hard bone quality, and this will induce resorption of the alveolar ridge during the bone remodeling process. The screw-type tools used in this study deliver relatively low amounts of force. The bone was also expanded sequentially in the deep area, and it was considered to be more effective in preventing cortical bone fracture. In addition, the conventional malleting process was minimized, thereby minimizing head echo and the resulting headaches, injury to the temporomandibular joint, and others.
Jensen et al.6 reported that mucoperiosteal elevation should be performed minimally in ridge splitting, and that the use of partial thickness flaps show good results. In this study, and in cases involving the maxillary anterior area where esthetics are required, full-thickness flap elevations were performed in the alveolar ridge and slightly below it. Afterwards, a partial flap was elevated. In the posterior areas, a full-thickness flap was elevated in most cases.
The ridge expansion technique mentioned in this case report is slightly different from the existing ridge splitting technique. The ridge splitting technique is a methodology to increase the ridge width by performing the ridge splitting using a chisel after the formation of a groove at the center of ridge crest using a saw or surgical bur and is mainly used in the maxilla. If the ridge splitting technique is performed in the mandible composed of mainly cortical bone, then it runs the risk of cortical bone fractures. Whereas, the ridge expansion technique is a stepwise technique using screws of gradually increasing width, so it has a lower risk of cortical bone fracture than the ridge splitting technique. Therefore, ridge expansion technique is considered to be an acceptable method to use on the mandible.
In this study, one case involving implant placement in the maxillary anterior area developed a complication of failed osseointegration. However, implant replacement was performed immediately after removal, and successful prosthesis treatments were completed. Buccal cortical bone fracture did not occur in any of the cases. Even after the prosthesis were functioning, all adjacent alveolar bones and soft tissues remained stable.
References
1. Buser D, Brägger U, Lang NP, Nyman S. Regeneration and enlargement of jaw bone using guided tissue regeneration. Clin Oral Implants Res. 1990; 1:22–32. PMID: 2099209.

2. Jovanovic SA, Spiekermann H, Richter EJ. Bone regeneration around titanium dental implants in dehisced defect sites: a clinical study. Int J Oral Maxillofac Implants. 1992; 7:233–245. PMID: 1398841.
3. Misch CM. Maxillofacial donor sites for sinus floor and alveolar reconstruction. In : Jensen OT, editor. The sinus bone graft. 2nd ed. Chicago: Quintessence Publishing;2006. p. 129–143.
4. Jensen J, Sindet-Pedersen S. Autogenous mandibular bone grafts and osseointegrated implants for reconstruction of the severely atrophied maxilla: a preliminary report. J Oral Maxillofac Surg. 1991; 49:1277–1287. PMID: 1955919.

5. Kim YK, Kim SG, Lee BG. Bone graft and implant. 1st ed. Seoul: Narae Publishing;2007. p. 435–467.
6. Jensen OT, Cullum DR, Baer D. Marginal bone stability using 3 different flap approaches for alveolar split expansion for dental implants: a 1-year clinical study. J Oral Maxillofac Surg. 2009; 67:1921–1930. PMID: 19686930.
7. Jensen OT, Cullum DR, Baer D. Marginal bone stability using 3 different flap approaches for alveolar split expansion for dental implants: a 1-year clinical study. J Oral Maxillofac Surg. 2009; 67:1921–1930. PMID: 19686930.
8. Chiapasco M, Ferrini F, Casentini P, Accardi S, Zaniboni M. Dental implants placed in expanded narrow edentulous ridges with the Extension Crest device. A 1-3-year multicenter follow-up study. Clin Oral Implants Res. 2006; 17:265–272. PMID: 16672021.
9. Nishioka RS, Kojima AN. Screw spreading: technical considerations and case report. Int J Periodontics Restorative Dent. 2011; 31:141–147. PMID: 21491013.
10. Chan HL, Fu JH, Koticha T, Benavides E, Wang HL. Ridge width gain with screw spreaders: a cadaver study. Implant Dent. 2013; 22:552–558. PMID: 24013399.
11. Sethi A, Kaus T. Maxillary ridge expansion with simultaneous implant placement: 5-year results of an ongoing clinical study. Int J Oral Maxillofac Implants. 2000; 15:491–499. PMID: 10960981.
12. Ferrigno N, Laureti M. Surgical advantages with ITI TE implants placement in conjunction with split crest technique. 18-month results of an ongoing prospective study. Clin Oral Implants Res. 2005; 16:147–155. PMID: 15777323.
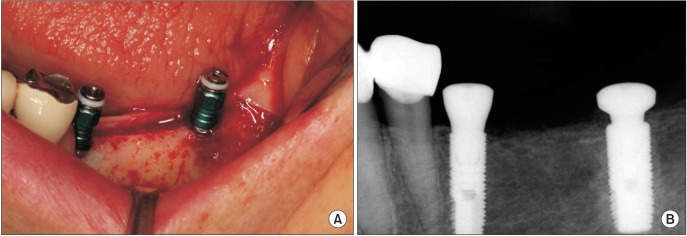
Fig. 1
Clinical view before implant placement. A. Preoperative intraoral photograph. B. Mucoperiosteal flap was elevated. Narrow alveolar ridge is observed.
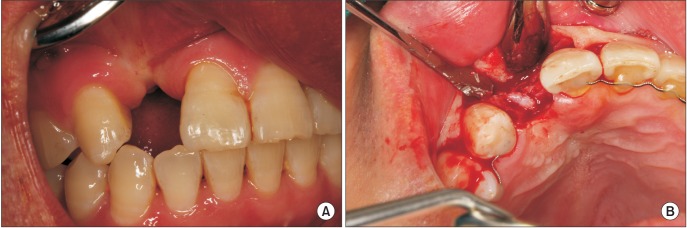
Fig. 2
Expansion of buccal plate achieved by splitting the ridge with bone expander in SplitMaster (Mr. Curette).
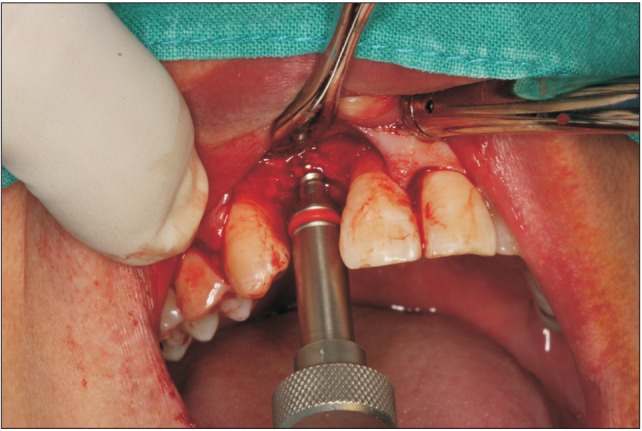
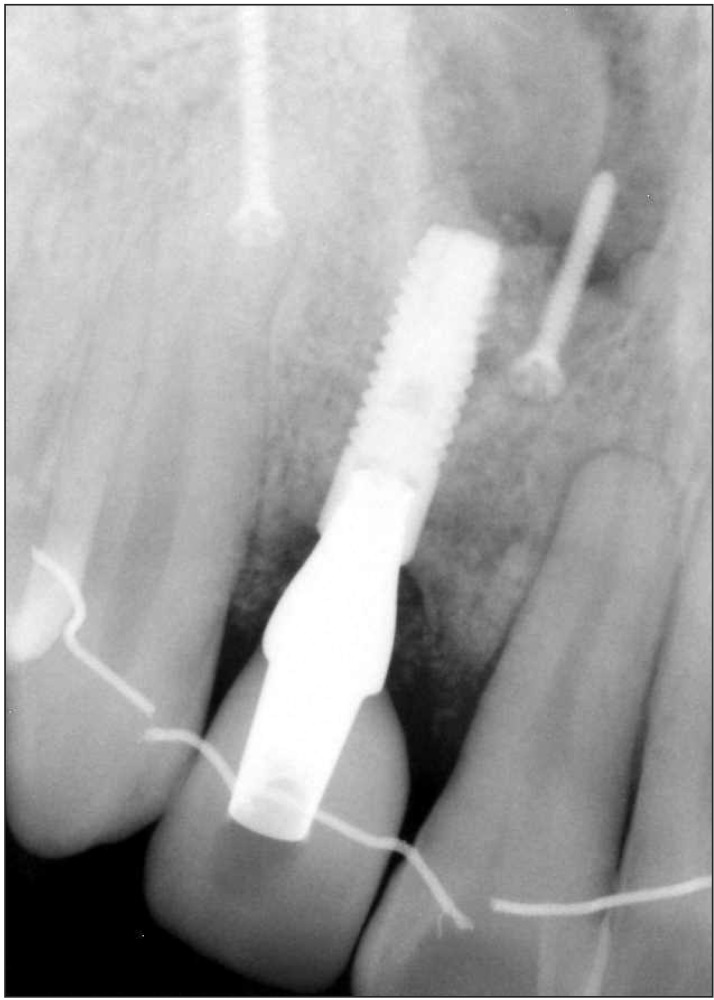
Fig. 3
A. Implant was placed at the expanded ridge. B. Periapical radiograph after implant placement.
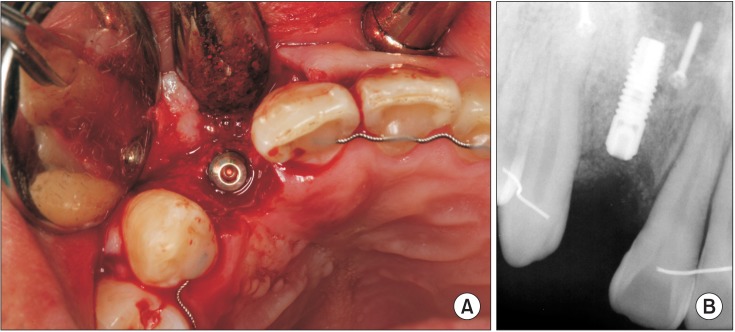
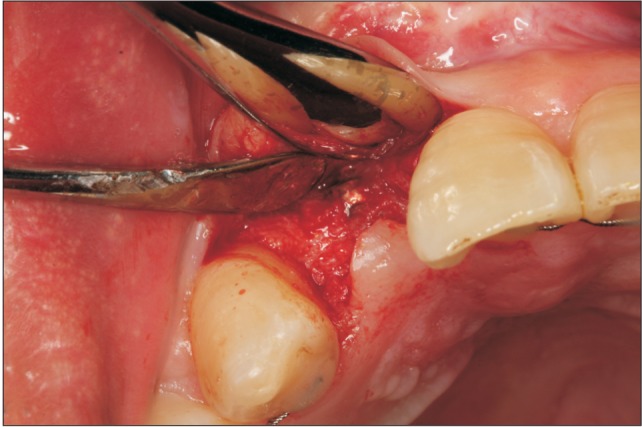
Fig. 8
Expansion of buccal plate achieved by splitting the ridge using the bone expander in SplitMaster (Mr. Curette).
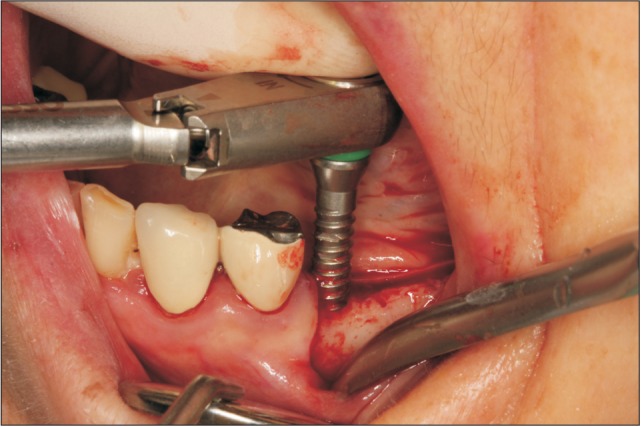
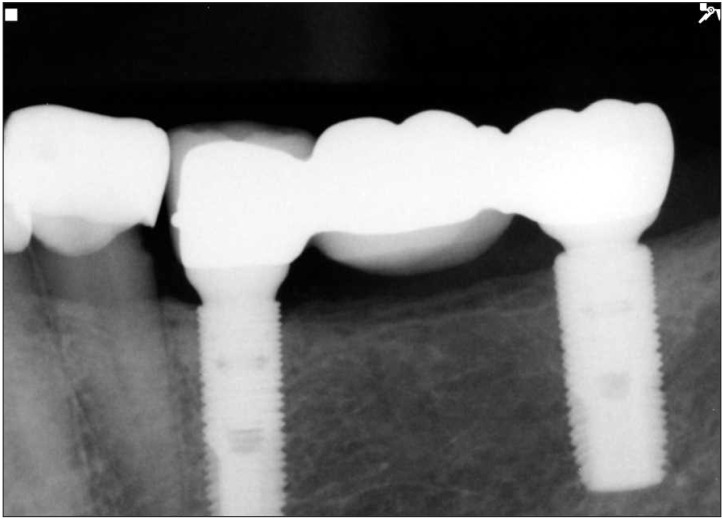
Fig. 9
A. Implants were placed at the expanded ridge. B. Periapical radiograph after implant placement.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download