Abstract
Objectives
This study aimed to assess and compare the levels of interleukin-1beta (IL-1β) and interleukin-6 (IL-6) in the crevicular fluid around healthy implants, implants with peri-implantitis, and healthy teeth.
Materials and Methods
This study evaluated 16 dental implants in 8 patients (4 males and 4 females). These patients had at least one healthy implant and one implant with peri-implantitis next to healthy teeth. The crevicular fluid was collected using absorbent cones and transferred to the laboratory. Specimens were evaluated by ELISA for interleukin levels. Data were analyzed using repeated measures ANOVA and Bonferroni tests (P<0.05).
Results
Levels of IL-1β in the crevicular fluid around implants with peri-implantitis were significantly higher than around healthy implants (P=0.002); the latter was significantly higher than around healthy teeth (P=0.015). A significant difference was found in the level of IL-6 in the crevicular fluid around implants with peri-implantitis and healthy implants (P=0.049) and also between implants with peri-implantitis and healthy teeth (P<0.001).
At present, use of dental implants for treatment of edentulism has become a widely popular treatment modality in dentistry1. Accumulation of microbial plaque on the implant surface and inadequacy of neutrophils lead to inflammation of the peri-implant tissues. Clinically, this condition is known as mucositis or peri-implantitis. Roos-Jansåker et al.2 and Ata-Ali et al.3 found the frequency of peri-implant mucositis to be 48% during 9-14 years postimplantation.
Peri-implant mucositis is a reversible inflammation of the peri-implant tissues. Early and late mucositis occur as a result of changes in the microbial flora around implants leading to an increase in Gram-negative microorganisms. The growth of Gram-negative bacteria causes an immune response at the site; inflammatory products enter the peri-implant gingival crevicular fluid4 and the spread of inflammation from the marginal gingiva to the peri-implant supporting tissues leads to bone loss and loss of gingival attachment. This process is known as peri-implantitis5.
The current criteria for assessment of periodontal tissues surrounding teeth and implants are based on clinical and radiographic changes. Researchers are searching for highly sensitive diagnostic biomarkers to detect peri-implant disease before tissue destruction. Saliva, serum, and crevicular fluid have been evaluated as suitable environments for biochemical and immunological analysis of periodontal tissues6. Infla mmatory products in periodontal disease are present in crevicular fluid. Analysis of these inflammatory mediators in the peri-implant crevicular fluid has been used to assess the health of peri-implant tissues7; and specific cytokines have been recognized as potential markers for the diagnosis of peri-implant disease8,9. Analysis of the crevicular fluid around teeth and implants is a non-invasive method to study the host response of the periodontium and inflamed tissues and can be an early indicator for detection of active periodontal disease.
Interleukin-1beta (IL-1β) and interleukin-6 (IL-6) are two pre-inflammatory cytokines that play a major role in periodontal destruction10,11. Biologic effects of IL-1β depend on its tissue concentration. In periodontal tissue, IL-1β causes bone destruction and induces the production of tissue destructive proteinases10.
The majority of studies have analyzed crevicular fluid in periodontal patients in terms of the presence of cytokines, and limited studies have focused on the analysis of crevicular fluid around implants with peri-implantitis. The number of studies comparing the level of cytokines in the crevicular fluid around healthy teeth, healthy implants, and implants with peri-implantitis in the same patient is scarce. Thus, we sought to compare the levels of IL-1β and IL-6 in gingival crevicular fluid around healthy teeth, healthy implants, and implants with peri-implantitis in the same patient.
Sixteen dental implants (Nobel Biocare, Göteborg, Sweden) in 8 patients (4 males and 4 females) were selected. These patients had at least one healthy implant and one implant with peri-implantitis next to healthy teeth. The crevicular fluid was collected using absorbent cones (Gapadent Co., Ltd., Tian Jin, China) and transferred to the laboratory. This cross-sectional study was approved by the Ethics Committee of Tehran University of Medical Sciences (Tehran, Iran). The inclusion criteria were as follows: 1) presence of at least one healthy tooth and two implants at different sites of the oral cavity one year or more after loading, and 2) at least one implant had to be healthy and another with peri-implantitis and at least 5 teeth in each quadrant.
A tooth was considered periodontally healthy if it had no bleeding on probing, no probing depth >3 mm, and gingiva was pink in color and had stippling.
An implant was considered healthy if it had no bleeding on probing, no probing depth >3 mm, gingiva was pink and had stippling, and there was no sign of exposure of implant threads in the parallel radiograph. The most coronal part of the rough surface was used as a reference of bone loss. Peri-implantitis was defined as bleeding on probing, presence of a pocket (probing depth >5 mm), and exposure of at least 2 implant threads in a parallel radiograph (implant success index >IV)12.
All clinical examinations were performed by an expert periodontist with 95% reproducibility using a Williams periodontal probe (Hu-Friedy, Chicago, IL, USA).
The exclusion criteria were smoking, pregnancy, history of systemic disease (cardiovascular disease, hypertension, renal disease, diabetes mellitus, liver disease, and others) affecting the periodontal and peri-implant tissues, history of antibiotic therapy in the past month, history of anti-inflammatory drug use in the past month, and patient noncompliance.
The crevicular fluid was collected from the deepest point of the sulcus around teeth and implants4.
in the sulcus according to studies by Griffiths et al.13 and Page14. The paper cones were placed in the sulcus for 30 seconds and inserted downward until reaching a resistance. Cones contaminated with blood or saliva were replaced. After sample collection, paper points were placed in Eppendorf tubes (Arian Gene Gostar, Tehran, Iran) containing 50γ phosphate buffered saline. Immediately after sampling, the specimens were frozen at -20℃ and transferred to the immunology laboratory under cold conditions.
All specimens were centrifuged for uniform dissemination of components absorbed by the absorbent cone. An ELISA test (Biocompare, South San Francisco, CA, USA) was performed and laboratory assessment was done.
The antigen dissolved in buffer was transferred to the wells using a sampler. The surface of plastic tubes was coated with anti-IL-1β and anti-IL-6 antibodies (in two separate kits; Arian Gene Gostar). Small amounts of antigens were absorbed into this plastic tube. The remaining free antigens were washed off. Large amounts of a neutral protein (bovine serum albumin) were added to the plate to block nonspecific adhesion of other proteins in the next steps of the experiment. Nonadherent proteins to the respective antibodies were washed off. A coloring agent was then added. The added coloring agent was a color-less material that is converted to a colored product by the action of the respective enzyme. As a result, the respective complex became detectable. The amount of IL-1β and IL-6 was measured by quantifying the amount of colored product in the plate by light density scanning of the plate and displayed using a software program (R&D Systems, Minneapolis, MN, USA).
Repeated measures ANOVA was used for the comparison of IL-1β and IL-6 levels at three sites in the patients. The Bonferroni test was applied for pairwise comparison of areas. Data were analyzed using SPSS version 20.0 (IBM Co., Armonk, NY, USA). A P-value less than 0.05 was considered statistically significant.
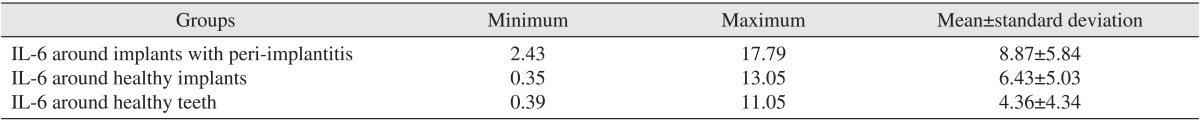
Significant differences were found between the healthy implant and implant with peri-implantitis (P=0.049) and also between the healthy tooth and implant with peri-implantitis (P<0.001). The mean levels of IL-6 in the crevicular fluid at three sites are shown in Table 1. However, the difference between the healthy tooth and healthy implant was not statistically significant (P=0.074).
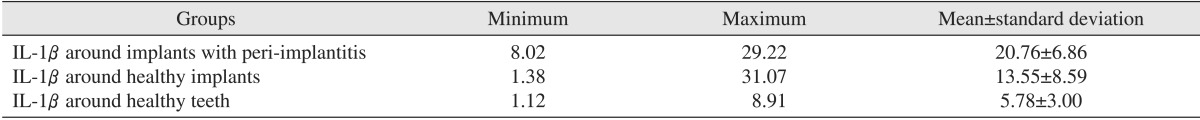
The mean levels of IL-1β in the crevicular fluid among the three groups are shown in Table 2.
According to the repeated measures ANOVA, significant differences existed between the three areas. The level of IL-1β was significantly different around the healthy implant and implant with peri-implantitis (P=0.002), around the healthy tooth and implant with peri-implantitis (P<0.001), and also around the healthy implant and healthy tooth (P=0.015).
The current criteria for the assessment of periodontal and peri-implant tissues are based on changes in radiographic findings and clinical conditions. Only after extensive demineralization can bone loss be detectable radiographically. Furthermore, radiographs do not completely display destructed areas and pathological changes. Therefore, it is not logical to rely solely on radiographic findings of periodontal and peri-implant tissues to make a diagnosis or commence treatment6.
Considering the high resemblance of the anatomy of periodontal and peri-implant tissues and also the fact that crevicular fluid is derived from periodontal tissues (around both teeth and implants), the biochemical and immunologic value of its constituents may be a suitable indicator of tissue changes. Among the new techniques, analysis of gingival crevicular fluid to assess the host response is of great value7.
This adjunct immunologic method provides comprehensive information regarding the current status and prognosis and treatment course of loaded implants as well as the analysis of patient responses to periodontal disease. By using such information, clinicians can more efficiently determine the treatment plan or take preventive measures7,8,9
This study compared the levels of IL-1β and IL-6 in the crevicular fluid around implants with peri-implantitis and around healthy teeth, and revealed that the level of IL-1β in the crevicular fluid around implants with peri-implantitis was significantly higher than around healthy implants. Also, the level of IL-1β in the latter was greater than around healthy teeth. Moreover, the difference between the level of IL-1β in the crevicular fluid around implants with peri-implantitis and healthy teeth was statistically significant. Significant differences were also found in the level of IL-6 in the crevicular fluid around implants with peri-implantitis and healthy implants, and also between implants with peri-implantitis and healthy teeth. However, the level of IL-6 was not significantly different in the crevicular fluid around healthy implants and healthy teeth.
Our findings confirmed those of many previous studies regarding the proinflammatory role of IL-1β11,15. In the current study, we assessed a healthy tooth, a healthy implant, and an implant with peri-implantitis all in the same patient as one important inclusion criterion. Also, in our study, sampling was performed at a specific time; which was the same for all patients (considering the fact that the circadian rhythm can affect gingival crevicular fluid volume). Therefore, our results may be more reliable than those of previous studies.
Nowzari et al.16 in 2008 compared the level of interleukins around healthy teeth and healthy implants and showed that the level of cytokines in the implant group was significantly higher than around teeth. Thus, despite the fact that the gingival tissue around teeth and implants was healthy in both groups, a significant difference existed in the level of cytokines around teeth and implants16.
However, some studies did not find a significant difference in the level of IL-1β in the crevicular fluid around healthy teeth and implants17,18. Several studies have reported signi-ficantly higher levels of IL-1β in the crevicular fluid around implants than around healthy teeth11,17,19,20,21. As mentioned earlier, in our study the difference in IL-1β levels between healthy implants and implants with peri-implantitis was significant.
Güncü et al.22 in 2012 evaluated the effect of inflammation on the level of cytokines in the crevicular fluid around implants. They divided specimens into two groups: with and without inflammation. After analysis, they reported significantly higher levels of IL-1β, IL-10, and osteoprotegerin in the crevicular fluid around implants with inflammation compared to noninflamed implants.
Yaghobee et al.23 in 2013 evaluated the level of IL-1β in the crevicular fluid around dental implants and investigated its association with periodontal parameters compared with healthy teeth. A total of 41 dental implants and 41 healthy teeth were studied as case and control groups, respectively. They showed a significant difference in the level of IL-1β between the two groups (P=0.001).
Liskmann et al.24 in 2006 assessed the level of IL-6 in the crevicular fluid and concluded that the level of IL-6 was significantly higher around implants with peri-implantitis compared to healthy implants. Thus, they introduced IL-6 as an effective marker for detection of peri-implant diseases and emphasized its efficacy in assessing the ability of the immune system to achieve an inflammatory balance.
Konttinen et al.25 in 2006 studied the level of IL-6 in the crevicular fluid and stated that a significant difference existed in the level of IL-6 in the crevicular fluid around implants with peri-implantitis and healthy implants. Therefore, peri-implant conditions may be treated with cytokine modulators.
In contrast to the above-mentioned studies, Mengel et al.26 in 1996 compared two groups of periodontitis and normal implant patients and reported no significant difference in the levels of IL-6 and IL-1β between the two groups.
Such conflicting results may be attributed to differences in the methodology of the studies. For example, the cited studies had significant differences with one another in terms of sample size, time lapsed following the loading of implants, type of restorations, definition of peri-implantitis, time of sampling (in terms of the stage of the inflammatory process), and sampling techniques.
Taking into account the findings of this cross-sectional study, long-term studies using a comparative approach for the assessment of biologic markers in the crevicular fluid around implants (especially immunologic markers) at regular time intervals are required to achieve more definite results regarding the application of these immunologic markers for detection of active sites of periodontal disease around implants.
Within the limitations of this small cross-sectional study, significant differences in the levels of IL-1β and IL-6 in the crevicular fluid of implants with peri-implantitis, healthy implants, and healthy teeth were noted. These markers may be used as adjuncts for assessing the state of peri-implant tissues. More studies with larger sample sizes in different populations are necessary.
Acknowledgements
The authors would like to thank Dr. Kharrazi Fard for his assistance in the statistical analysis.
References
1. Abrishami MR, Sabour S, Nasiri M, Amid R, Kadkhodazadeh M. Comparison of the reproducibility of results of a new peri-implantitis assessment system (implant success index) with the Misch classification. J Korean Assoc Oral Maxillofac Surg. 2014; 40:61–67. PMID: 24868502.

2. Roos-Jansåker AM, Lindahl C, Renvert H, Renvert S. Nine- to fourteen-year follow-up of implant treatment. Part II: presence of peri-implant lesions. J Clin Periodontol. 2006; 33:290–295. PMID: 16553638.

3. Ata-Ali J, Flichy-Fernandez AJ, Ata-Ali F, Penarrocha-Diago M, Penarrocha-Diago M. Clinical, microbiologic, and host response characteristics in patients with peri-implant mucositis. Int J Oral Maxillofac Implants. 2013; 28:883–890. PMID: 23748323.

4. Petković AB, Matić SM, Stamatović NV, Vojvodić DV, Todorović TM, Lazić ZR, et al. Proinflammatory cytokines (IL-1beta and TNF-alpha) and chemokines (IL-8 and MIP-1alpha) as markers of peri-implant tissue condition. Int J Oral Maxillofac Surg. 2010; 39:478–485. PMID: 20207110.
5. Sanz M, Chapple IL. Working Group 4 of the VIII European Workshop on Periodontology. Clinical research on peri-implant diseases: consensus report of Working Group 4. J Clin Periodontol. 2012; 39(Suppl 12):202–206. PMID: 22533957.

6. Greenstein G, Caton J. Periodontal disease activity: a critical assessment. J Periodontol. 1990; 61:543–552. PMID: 2213463.

7. Dennison DK, Van Dyke TE. The acute inflammatory response and the role of phagocytic cells in periodontal health and disease. Periodontol 2000. 1997; 14:54–78. PMID: 9567966.

8. Okada H, Murakami S. Cytokine expression in periodontal health and disease. Crit Rev Oral Biol Med. 1998; 9:248–266. PMID: 9715365.

9. Panagakos FS, Aboyoussef H, Dondero R, Jandinski JJ. Detection and measurement of inflammatory cytokines in implant crevicular fluid: a pilot study. Int J Oral Maxillofac Implants. 1996; 11:794–799. PMID: 8990643.
10. Stashenko P, Fujiyoshi P, Obernesser MS, Prostak L, Haffajee AD, Socransky SS. Levels of interleukin 1 beta in tissue from sites of active periodontal disease. J Clin Periodontol. 1991; 18:548–554. PMID: 1894750.
11. Ataoglu H, Alptekin NO, Haliloglu S, Gursel M, Ataoglu T, Serpek B, et al. Interleukin-1beta, tumor necrosis factor-alpha levels and neutrophil elastase activity in peri-implant crevicular fluid. Clin Oral Implants Res. 2002; 13:470–476. PMID: 12453123.
12. Kadkhodazadeh M, Esfahrood ZR, Amid R, Zarnegarnia P. Comparison of the acceptability of a new scoring system with Misch's classification for dental implant success determination. J Long Term Eff Med Implants. 2012; 22:85–93. PMID: 23016792.

13. Griffiths GS, Curtis MA, Wilton JM. Selection of a filter paper with optimum properties for the collection of gingival crevicular fluid. J Periodontal Res. 1988; 23:33–38. PMID: 2963902.

14. Page RC. Host response tests for diagnosing periodontal diseases. J Periodontol. 1992; 63(4 Suppl):356–366. PMID: 1573549.

15. Casado PL, Canullo L, de Almeida Filardy A, Granjeiro JM, Barboza EP, Leite Duarte ME. Interleukins 1β and 10 expressions in the periimplant crevicular fluid from patients with untreated periimplant disease. Implant Dent. 2013; 22:143–150. PMID: 23459153.

16. Nowzari H, Botero JE, DeGiacomo M, Villacres MC, Rich SK. Microbiology and cytokine levels around healthy dental implants and teeth. Clin Implant Dent Relat Res. 2008; 10:166–173. PMID: 18218050.

17. Murata M, Tatsumi J, Kato Y, Suda S, Nunokawa Y, Kobayashi Y, et al. Osteocalcin, deoxypyridinoline and interleukin-1beta in peri-implant crevicular fluid of patients with peri-implantitis. Clin Oral Implants Res. 2002; 13:637–643. PMID: 12519339.
18. Melo RF, Lopes BM, Shibli JA, Marcantonio E Jr, Marcantonio RA, Galli GM. Interleukin-1β and interleukin-6 expression and gene polymorphisms in subjects with peri-implant disease. Clin Implant Dent Relat Res. 2012; 14:905–914. PMID: 21414132.

19. Stashenko P, Dewhirst FE, Peros WJ, Kent RL, Ago JM. Synergistic interactions between interleukin 1, tumor necrosis factor, and lymphotoxin in bone resorption. J Immunol. 1987; 138:1464–1468. PMID: 3492553.
20. Preiss DS, Meyle J. Interleukin-1 beta concentration of gingival crevicular fluid. J Periodontol. 1994; 65:423–428. PMID: 8046557.
21. Zhong Y, Slade GD, Beck JD, Offenbacher S. Gingival crevicular fluid interleukin-1beta, prostaglandin E2 and periodontal status in a community population. J Clin Periodontol. 2007; 34:285–293. PMID: 17378884.
22. Güncü GN, Akman AC, Günday S, Yamalık N, Berker E. Effect of inflammation on cytokine levels and bone remodelling markers in peri-implant sulcus fluid: a preliminary report. Cytokine. 2012; 59:313–316. PMID: 22592038.

23. Yaghobee S, Khorsand A, Paknejad M. Comparison of interleukin-1β levels in gingival crevicular fluid and peri-implant crevicular fluid and its relationship with clinical indexes. J Dent (Tehran). 2013; 10:1–9. PMID: 23724197.
24. Liskmann S, Vihalemm T, Salum O, Zilmer K, Fischer K, Zilmer M. Correlations between clinical parameters and interleukin-6 and interleukin-10 levels in saliva from totally edentulous patients with peri-implant disease. Int J Oral Maxillofac Implants. 2006; 21:543–550. PMID: 16955604.
25. Konttinen YT, Lappalainen R, Laine P, Kitti U, Santavirta S, Teronen O. Immunohistochemical evaluation of inflammatory mediators in failing implants. Int J Periodontics Restorative Dent. 2006; 26:135–141. PMID: 16642902.
26. Mengel R, Stelzel M, Hasse C, Flores-de-Jacoby L. Osseointegrated implants in patients treated for generalized severe adult periodontitis. An interim report. J Periodontol. 1996; 67:782–787. PMID: 8866317.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download