Abstract
Objectives
To identify post-treatment prognostic factors for medication-related osteonecrosis of the jaw (MRONJ).
Materials and Methods
We evaluated 54 MRONJ patients who visited the Department of Dentistry, Ajou University Hospital, from May 2007 to March 2014. Twenty-one patients were surgically managed with debridement or sequestrectomy and 33 patients were conservatively managed using antibiotics. Correlations of age, sex, stage, bisphosphonate duration and type, and drug holiday with the prognosis of MRONJ were investigated. Correlations were verified by logistic regression analysis and t-tests with a significance level of 0.05.
Results
Clinical outcomes were evaluated on the basis of both clinical and radiographic findings. Twelve out of 21 surgically managed patients showed a favorable prognosis and nine patients relapsed. Thirty-one of the 33 conservatively managed patients showed no specific change in prognosis, and two patients worsened. Statistical analyses of the conservative management group did not reveal any correlation of the above factors with the prognosis of conservative management. Drug holiday was the only prognostic factor in the surgical management group (P=0.031 in logistic regression analysis, P=0.004 in t-test).
Bisphosphonates have been used for hypercalcemia of malignancy, osteolytic lesions of multiple myeloma, and Paget's disease1. In addition, the antiresorptive activity has produced excellent results for both prevention and treatment of osteoporosis. Medication (previously, bisphosphonate)-related osteonecrosis of the jaw (MRONJ) is a well-known complication of bisphosphonates in the oral and maxillofacial regions, as well as an atypical femur fracture in orthopedic surgery. The third edition of a position paper was published by the American Association of Oral and Maxillofacial Surgeons (AAOMS) in 2014, in which the definition of MRONJ is current or previous treatment with antiresorptive or antiangiogenic agents, exposed bone in the maxillofacial region for more than 8 weeks, and no history of radiation therapy to the jaw bone2.
MRONJ is relatively rare. However, its impacts are significant and include symptoms such as delayed wound healing, loss of oral mucosa, continued pain from exposure, necrosis, and purulent secretion of the jaw bones. MRONJ has been continuously reported globally as well as in Korea since its first report in 20033. An Australian study reported that the occurrence of MRONJ in patients receiving bisphosphonate therapy was 0.01% to 0.04%4. The occurrence of MRONJ following intravenous administration of bisphosphonate has been reported as 0.8% to 12% by the American Society of Bone and Mineral Research5. The first national survey of MRONJ in Korea conducted by the Korean Association of Oral and Maxillofacial Surgeons reported an occurrence of 0.04% (1/2,300)6.
The pathophysiology and treatment principles of MRONJ remain debatable. The risk of MRONJ may increase as its duration extends beyond 3 years7. A drug holiday of about 1 year after 5 years of drug therapy has been recommended8. However, there are no established prognostic factors for MRONJ after surgical management. This study retrospectively investigated prognostic factors including drug holidays after surgical management of patients diagnosed with MRONJ.
The present study was granted an exemption by the institutional review board of Ajou University Hospital because it is a retrospective study. The study involved 54 patients diagnosed with MRONJ who visited the Department of Dentistry, Ajou University Hospital from May 2007 to March 2014. According to the treatment guidelines of the Korean Position Paper for BRONJ7, a drug holiday of at least three months is recommended for patients on oral bisphosphonate. These recommendations were not evidence-based. Our investigation includes all data before the three-month drug holiday. Symptoms related to MRONJ were evaluated every 3 months of follow-up to decide the adequate time for surgical management.
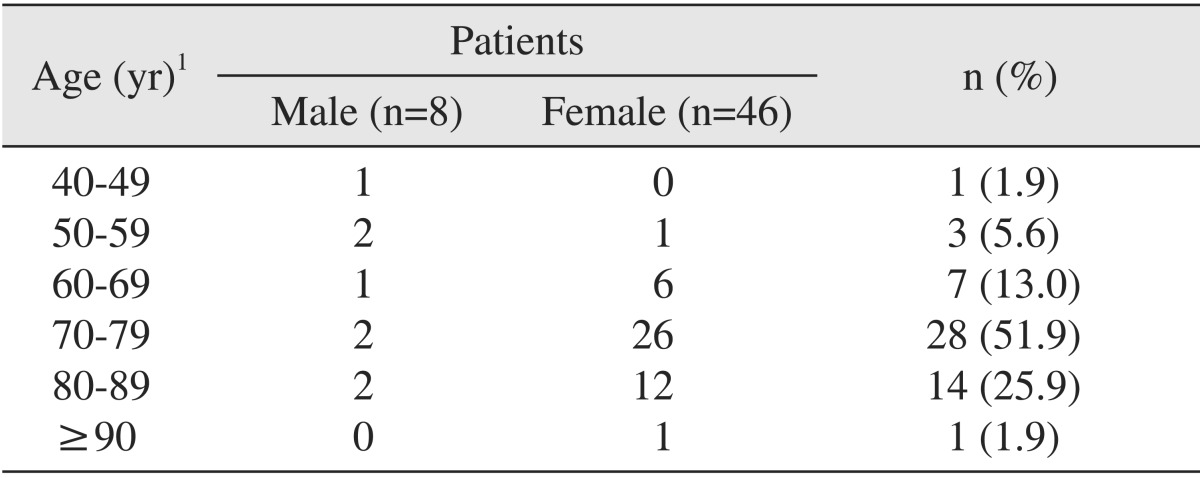
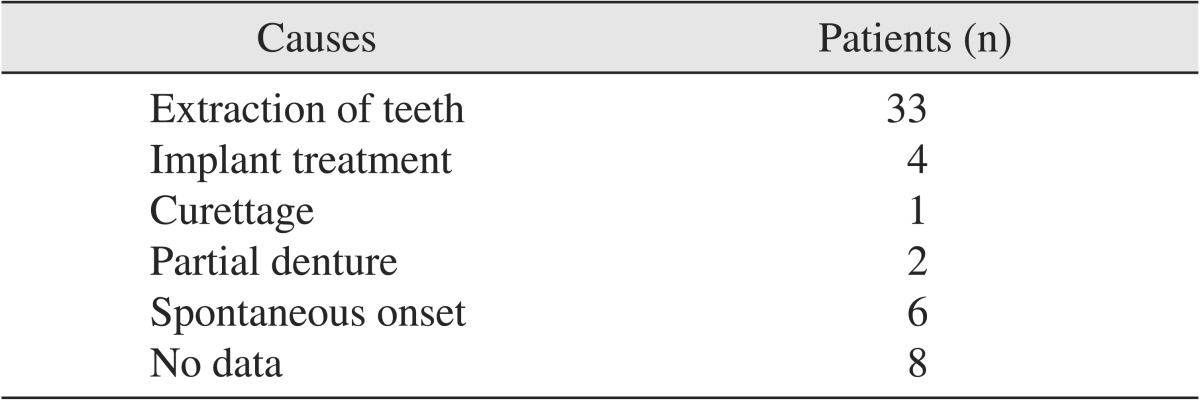
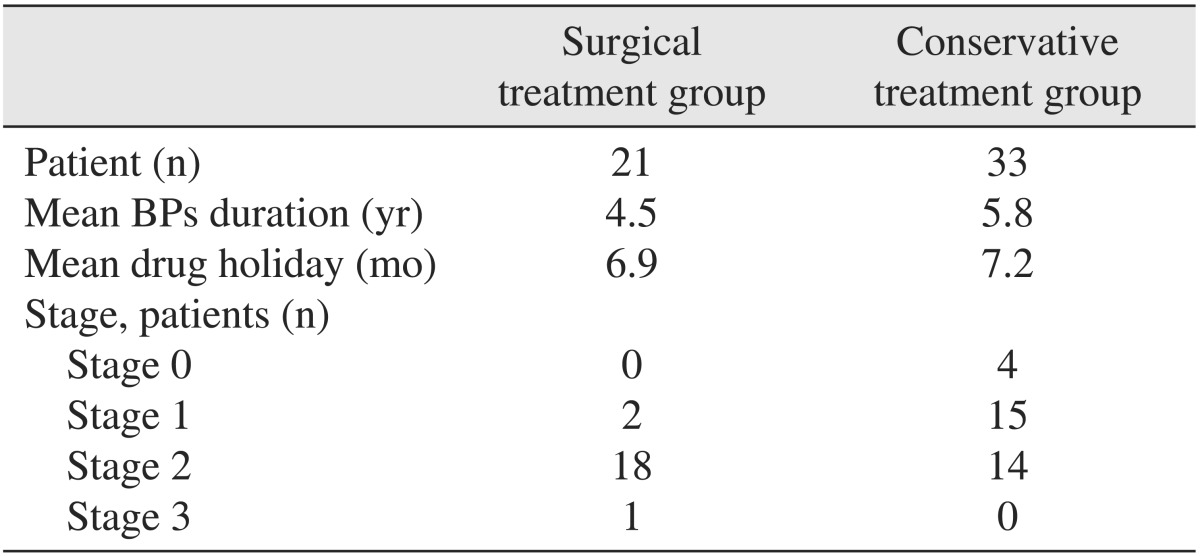
Of the 54 patients, eight were male and 46 were female. They ranged from 42 to 90 years of age (average 73.7 years), with septuagenarians predominating.(Table 1) Patients were classified according to the diagnostic criteria of the AAOMS guidelines2. Medication with antibiotics was used in all 33 patients who were conservatively managed; the average times spent on bisphosphonate therapy and drug holiday were 5.8 years and 7.2 months, respectively. Twenty-one patients were managed surgically with debridement or sequestrectomy; the average times spent on bisphosphonate therapy and drug holiday were 4.5 years and 6.9 months, respectively.
The mean follow up period was 7.8 months in the surgical and conservative treatment group. The surgical treatment group was observed over 8.6 months (range, 3 to 24 months).
In the surgical treatment group, evaluation of prognosis was done every 3 months. For clinical success criteria, a favorable prognosis was no exposure of bone with no evidence of infection and no pain. For radiographic success criteria, a favorable prognosis was the bone operation site showing a continuous trabecular pattern on the follow-up radiologic exam.
Various independent variable factors influencing prognosis were statistically analyzed, including gender, age, disease stage, duration of bisphosphonate use, type of bisphosphonates, and drug holiday. SPSS version 17.0 software (SPSS Inc., Chicago, IL, USA) was used for the statistical analyses. The dependent variables were prognosis of the conservative and surgical groups. Chi-square tests, t-tests, and logistic regression analyses were used according to the characteristics of each independent or dependent variable. The significance level was 0.05.
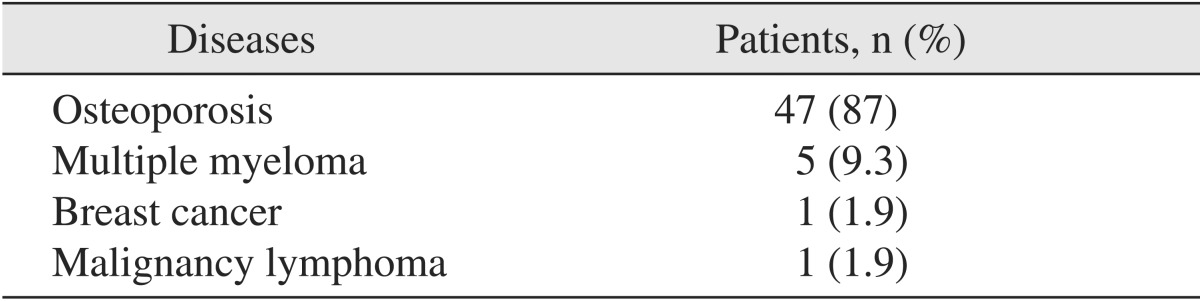
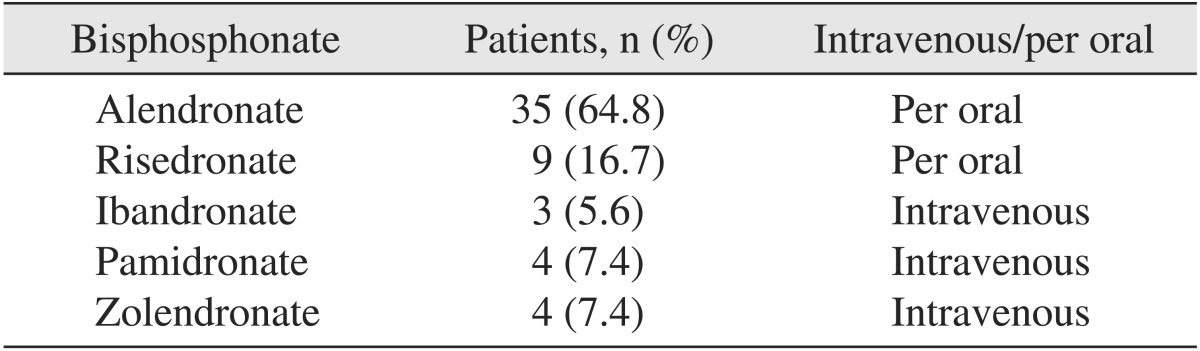
The causes for prescribing bisphosphonates and classification of the bisphosphonates prescribed are summarized in Tables 2 and 3, respectively. The causative factors for MRONJ onset are summarized in Table 4. Surgery was performed in 18 of 32 patients for stage 2, one patient for stage 3, and two of 17 patients for stage 1.(Table 5)
Twenty-one of the surgically managed patients previously complained of pain and mucosal swelling with bone exposure and infection in the preoperative stage. Surgery involved sequestrectomy (n=16) and debridement (n=5); all the wounds were closed with tension-free suture. Twelve of 21 patients (57%) in the surgical management group had good prognosis compared to nine patients (43%) with poor prognosis. Thirty-one of the 33 patients in the conservative management group did not display any improvement of symptoms; the remaining two patients complained of more severe pain and infection.
The 12 patients (3 males, 9 females) who had good prognosis after surgical treatment averaged 72.3 years of age. Their average period of bisphosphonate administration was 4.9 years (range, 12 months to 15 years) and the average drug holiday was 9.8 months (range, 1 month to 2 years). Nine patients received alendronates (Fosamax Tab.; MSD Korea, Seoul, Korea) therapy and three patients received pamidronates (Panorin Soft Cap.; Hanlim, Seoul, Korea) therapy. For the nine patients with poor prognosis after surgical treatment, the average age was 77.8 years. All were females and stage 2 according to the AAOMS guidelines. Bisphosphonate was administered for an average of 3.9 years (range, 2 months to 10 years) and the average drug holiday was 3.1 months (ranging from immediately to 8 months). Of the nine patients, eight received Fosamax therapy and the remaining patient received Maxmarvil Tab. (YuYu Pharma, Seoul, Korea). The stage of two patients changed to stage 0, that of 5 patients changed to stage 1, and the rest changed to stage 2 during the follow-up period.
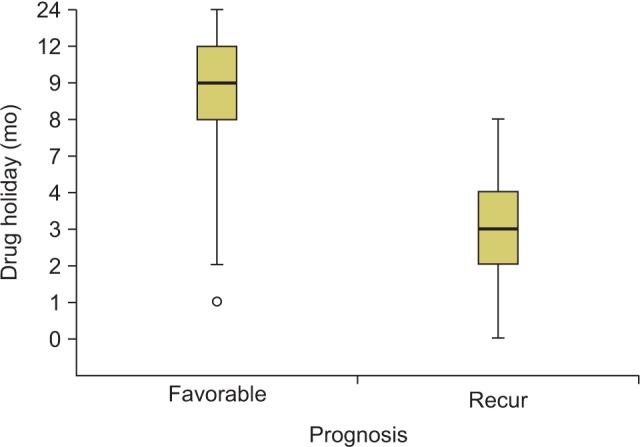
Additional logistic regression analysis was used on the meaningful variables from the chi-square tests and t-tests. A correlation was found between drug holiday and prognosis (P=0.031 in logistic regression analysis, P=0.004 in t-test) in the surgical treatment group. No other results were statistically significant, including the conservative management group (P>0.05). By quartile, the drug holiday lengths of the patients with a good prognosis were 7.25 months for the lowest 25%, 9 months for the middle 50%, and 12 months for the top 25%. The drug holiday lengths of the patients with poor prognosis were 1.5 months for the lowest 25%, 3 months for the middle 50%, and 4 months for the top 25%.(Fig. 1)
The purpose of MRONJ treatment is to improve patients' quality of life by reduction of pain, control of secondary infections, and control of bone exposure6. Effective treatment of MRONJ has not been established; the best approach is prevention followed by conservative management, such as pain reduction or antibiotic use4,6,9. Recently, the importance of surgical management has been emphasized10.
In a 2009 study in which patients were treated only conservatively, complete healing was observed in only 15% of patients (4 of 26), with seven cases (27%) progressing11. The present results were similar; there was no improvement of symptoms and two patients worsened in the 33 conservatively managed patients.
Although surgical treatment is recommended only for stage 3 patients2, it has been reported that the symptoms can become severe despite the administration of antibiotics in stage 2 patients11,12,13. In one of these studies13, nine of 13 patients (69.2%) treated surgically (among a total of 28 stage 2 patients) showed good results. Our study revealed a similar result, showing symptom improvements in 11 of 20 (55%) surgically managed patients.
The duration of administration is known to be a prognostic factor, and the occurrence of BRONJ may increase in patients who receive bisphosphonate for over 3 years7. In general, 1 year of drug holiday is recommended after 5 years of bisphosphonate therapy8. A recent MRONJ paper recommended that clinicians may consider discontinuation of oral bisphosphonates for a period of 2 months for those patients who have taken an oral bisphosphonate for more than 4 years or have taken corticosteroids or antiangiogenic medications2. Usually, a 3-month drug holiday is recommended before surgical decision making for patients on bisphosphonate therapy at Ajou University Hospital7.
While there are many studies that have examined the causative factors of MRONJ, little is known about the prognostic factors of surgical management of MRONJ. The stage, underlying diseases, administration route, and lesion size are known to affect the prognosis after surgical treatment14,15,16,17.
In the present study, drug holiday was a significant correlation factor for the prognosis in the surgical management group. The drug holiday was statistically significantly shorter in patients with poor prognosis (P=0.031; <0.05 in logistic regression analysis). The drug holiday must be continued at least 4 months, as patients with a poor prognosis had durations positioned at 1.5 to 4 months in quartile comparison analysis. The relatively good prognosis of patients with an adequate drug holiday may coincide with prior findings18 that the risk of fracture is not increased despite the decrease in bone density after cessation of bisphosphonate. Compared to other studies, patients taking antiresorptive per oral drugs were more numerous than patients who received bisphosphonate intravenously in our study. Differences in population characteristics may partially explain the results.
In conservative management of MRONJ, there was no improvement of symptoms, while surgical management resulted in a good prognosis. Drug holiday was a prognostic factor in the surgical management group (P<0.05). Drug holiday duration should be at least 4 months to prevent a poor prognosis after surgical management.
References
1. Devogelaer JP. Treatment of bone diseases with bisphosphonates, excluding osteoporosis. Curr Opin Rheumatol. 2000; 12:331–335. PMID: 10910187.

2. Medication-related osteonecrosis of the Jaw--2014 update [Internet]. Rosemont (IL): American Association of Oral and Maxillofacial Surgeons;cited 2014 Apr 1. Available from: http://www.aaoms.org/docs/position_papers/mronj_position_paper.pdf?pdf=MRONJ-Position-Paper.
3. Marx RE. Pamidronate (Aredia) and zoledronate (Zometa) induced avascular necrosis of the jaws: a growing epidemic. J Oral Maxillofac Surg. 2003; 61:1115–1117. PMID: 12966493.

4. Mavrokokki T, Cheng A, Stein B, Goss A. Nature and frequency of bisphosphonate-associated osteonecrosis of the jaws in Australia. J Oral Maxillofac Surg. 2007; 65:415–423. PMID: 17307586.

5. Khosla S, Burr D, Cauley J, Dempster DW, Ebeling PR, Felsenberg D, et al. American Society for Bone and Mineral Research. Bisphosphonate-associated osteonecrosis of the jaw: report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2007; 22:1479–1491. PMID: 17663640.

6. Lee JK, Kim KW, Choi JY, Moon SY, Kim SG, Kim CH, et al. Bisphosphonates-related osteonecrosis of the jaw in Korea: a preliminary report. J Korean Assoc Oral Maxillofac Surg. 2013; 39:9–13. PMID: 24471011.

7. The Korean Endocrine Society. The Korean Society of Bone Metabolism. The Korean Society of Osteoporosis. The Korean Association of Oral and Maxillofacial Surgeons. Bisphosphonate related osteonecrosis of the jaw (BRONJ): position statement of Korea. J Korean Endocr Soc. 2009; 24:227–230.
8. Bilezikian JP. Osteonecrosis of the jaw--do bisphosphonates pose a risk? N Engl J Med. 2006; 355:2278–2281. PMID: 17135582.
9. Park YJ, Pyo SW, Kim JA, Min JK. A case of avascular necrosis of mandible associated with the use of bisphosphonate in a patient with rheumatoid arthritis and osteoporosis. J Korean Rheum Assoc. 2006; 13:150–154.
10. Carlson ER. Management of antiresorptive osteonecrosis of the jaws with primary surgical resection. J Oral Maxillofac Surg. 2014; 72:655–657. PMID: 24480762.

11. Thumbigere-Math V, Sabino MC, Gopalakrishnan R, Huckabay S, Dudek AZ, Basu S, et al. Bisphosphonate-related osteonecrosis of the jaw: clinical features, risk factors, management, and treatment outcomes of 26 patients. J Oral Maxillofac Surg. 2009; 67:1904–1913. PMID: 19686928.

12. Ruggiero SL, Fantasia J, Carlson E. Bisphosphonate-related osteonecrosis of the jaw: background and guidelines for diagnosis, staging and management. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006; 102:433–441. PMID: 16997108.

13. Lee HK, Seo MH, Pang KM, Song SI, Lee JK. Comparative study on surgical and conservative management of bisphosphonate-related osteonecrosis of the jaw (BRONJ) in disease stage 2. J Korean Assoc Maxillofac Plast Reconstr Surg. 2013; 35:302–309.

14. Stockmann P, Burger M, von Wilmowsky C, Ebker T, Lutz R, Bauersachs A, et al. The outcome after surgical therapy of bisphosphonate-associated osteonecrosis of the jaw--results of a clinical case series with an average follow-up of 20 months. Clin Oral Investig. 2014; 18:1299–1304.
15. Holzinger D, Seemann R, Klug C, Ewers R, Millesi G, Baumann A, et al. Long-term success of surgery in bisphosphonate-related osteonecrosis of the jaws (BRONJs). Oral Oncol. 2013; 49:66–70. PMID: 22892237.

16. Graziani F, Vescovi P, Campisi G, Favia G, Gabriele M, Gaeta GM, et al. Resective surgical approach shows a high performance in the management of advanced cases of bisphosphonate-related osteonecrosis of the jaws: a retrospective survey of 347 cases. J Oral Maxillofac Surg. 2012; 70:2501–2507. PMID: 22883322.

17. Mücke T, Koschinski J, Deppe H, Wagenpfeil S, Pautke C, Mitchell DA, et al. Outcome of treatment and parameters influencing recurrence in patients with bisphosphonate-related osteonecrosis of the jaws. J Cancer Res Clin Oncol. 2011; 137:907–913. PMID: 20927569.

18. Black DM, Schwartz AV, Ensrud KE, Cauley JA, Levis S, Quandt SA, et al. FLEX Research Group. Effects of continuing or stopping alendronate after 5 years of treatment: the fracture intervention trial long-term extension (FLEX): a randomized trial. JAMA. 2006; 296:2927–2938. PMID: 17190893.

Fig. 1
Comparison quartile of drug holiday by prognosis. The drug holiday of patients with a good prognosis was 7.25 months for the bottom 25%, 9 months for the middle 50%, and 12 months for the top 25%. The drug holiday of patients with a poor prognosis was 1.5 months for the bottom 25%, 3 months for the middle 50%, and 4 months for the top 25%.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download