Abstract
Clear cell odontogenic carcinoma (CCOC) is a rare jaw tumor that was classified as a malignant tumor of odontogenic origin in 2005 by the World Health Organization because of its aggressive and destructive growth capacity and metastasis to the lungs and lymph nodes. We report a case of a 66-year-old female who had swelling, incision and drainage history and a well-defined unicystic radiolucent lesion that was comparable to a cystic lesion. At first, the patient received decompression, and the lesion size decreased. Three months after decompression, cyst enucleation was performed. The pathologic result indicated that the lesion was CCOC. In this report we emphasize that patients with painful cystic lesions in addition to jaw enlargement and loosening teeth should be considered for the possibility of malignancy.
Clear cell odontogenic carcinoma (CCOC) is a rare jaw tumor that was first described by Hansen et al.1 in 1985, in which patients presented with local bony invasions without metastasis. At first, CCOC was called a clear cell odontogenic tumor or clear cell ameloblastoma, and was considered more aggressive than ameloblastoma. The potential for CCOC to metastasize was initially unclear; however, CCOC was defined as a benign tumor in the 1992 World Health Organization (WHO) classification2.
The WHO reclassified CCOC as a malignant tumor of odontogenic origin in 20053 because of its aggressive and destructive growth capacity and metastasis to the lungs and lymph nodes4,5,6,7,8. About onethird of CCOC cases were initially misdiagnosed, and the primary diagnosis was ameloblastoma which lead to inadequate treatment for some patients. In this case report, we describe a case of a CCOC, which presented in a similar manner to a cystic lesion; the patient was misdiagnosed and received insufficient treatment. We introduce this case to discuss differential patient presentations to reduce the rate of malignancy misdiagnosis.
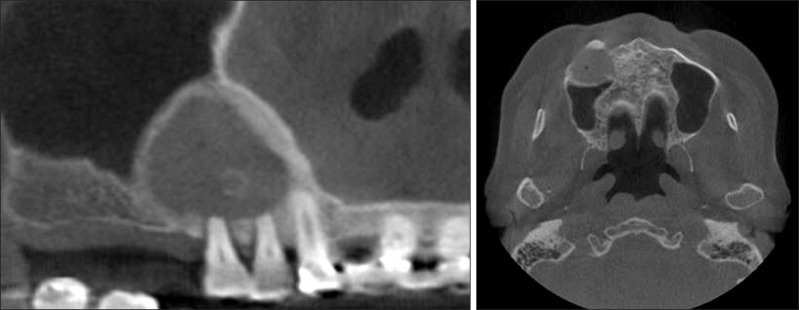
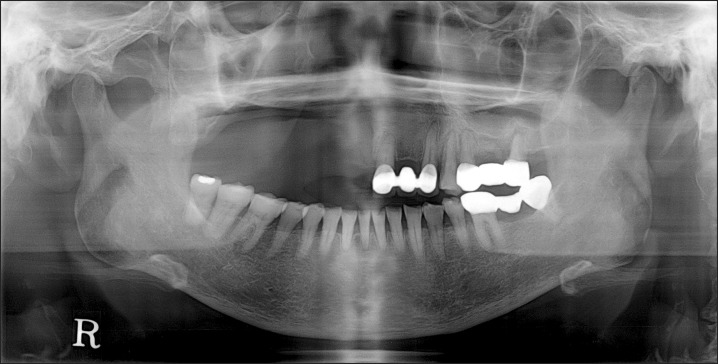
A 66-year-old female visited the Department of Oral and Maxillofacial Surgery at Yonsei Dental Hospital due to swelling and pain on the right premolar maxillary area. Incision and drainage had been performed at a local clinic 5 days previously. Clinical examination showed fluctuating swelling on the right maxillary vestibule with tenderness to palpation, severe tooth mobility and loss of vitality on the first and second premolars and no appreciable cervical lymphadenopathy. A panoramic radiograph revealed an approximately 27×29 mm well-defined radiolucency in the apex of the maxillary right premolars with root resorption.(Fig. 1) A computed tomography (CT) scan showed a low attenuated cystic lesion with a volume of 7,419 mm3 (Simplant software; Materialise, Leuven, Belgium).(Fig. 2)
At first, the lesion was diagnosed as infected odontogenic cyst (radicular cyst), the patient received decompression in order to separate the cyst from maxillary sinus wall. A yellowish exudate was discharged from the cyst while a local anesthetic was injected. The cystic wall was too thin and fragile to be sent for pathologic examination. Two months after decompression, a panoramic radiograph showed that the lesion size was reduced to approximately 25×26 mm.(Fig. 3) The lesion was reduced to a volume of 4,797 mm3 (Simplant software) on the 3-month follow-up conebeam CT.(Fig. 4) The measurement and comparison may not be precise because of the differences in CT imaging; however, there was definite shrinkage of the lesion.(Fig. 5)
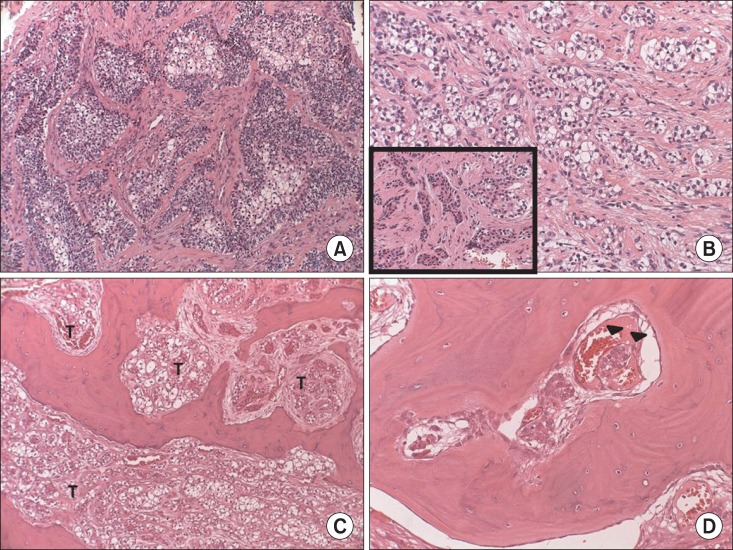
Because there was not a change in the lesion size, a cyst enucleation was performed and specimens were sent to oral pathology. Unexpectedly, the pathologic results indicated that the mass was CCOC.(Fig. 6. A, 6. B) Magnetic resonance imaging of the neck and positron emission tomography CT, were taken to examine the lymph nodes and distant metastasis.(Fig. 7) There were no pathologic lymph nodes and evidence of metastasis. A partial maxillectomy was performed without neck dissection. An obturator was placed at the time of surgery and a 2.4×2.0 cmsized CCOC with a positive basal resection margin, massive bone marrow infiltration and lymphovascular permeation was reported.(Fig. 6. C, 6. D)
Postoperative radiotherapy was conducted 1 month after surgery. No recurrence or metastasis was detected 10 months after the surgery.(Fig. 8)
Nearly 100 cases of CCOC have been reported in the Englishlanguage literature to date, and these tumors have a higher reported incidence in females with an male/female ratio of 1 : 1.8. Most cases of CCOC have been diagnosed in patients over the age of 40, with an average age of 54 years. The mandible is more frequently involved than the maxilla, and the posterior of the jaw is a more frequent site than the anterior site9,10,11.
Radiographic findings show mainly radiolucent lesions with or without regular margins, although some cases exhibited a mixed radiolucent-radiopaque lesion. Previous reports have suggested that painless swelling was the most common clinical symptom. In addition, tooth mobility and pain were occasionally associated as symptoms9,10,11.
Approximately one half of patients that were diagnoses with CCOC experienced a recurrence. The likelihood of the recurrence depended on the method of initial therapy and the extent of the tumor invasion. Three-quarters of the patients who were treated with conservative care (curettage or enucleation) had recurrence and onethird of the patients who were treated with resection experienced a recurrence. Conservative care (curettage or enucleation) and presence of soft tissue involvement were associated with a higher recurrence rate10,12. The ideal treatment approach for CCOC has not been determined. A wide resection with at least 1 cm of a tumor-free margin is recommended and when there is evidence broad soft tissue invasion, palpable neck lymph node, perineural invasion or tumor removal without free margins, adjuvant neck dissection and/or radiotherapy should be considered10,12,13. However, except for squamous cell carcinoma and high-grade central mucoepidermoid carcinoma, neck dissection is rarely required for maxillary carcinomas without nodal metastases12,13,14.
In our case, the patient had swelling, incision and drainage history and a well-defined unicystic radiolucent lesion, that was comparable with a cystic lesion. At first we misdiagnosed the lesion as an infected cyst, performed decompression and were unable to send specimen for pathologic examination. Our treatment was limited because we did not make a correct diagnosis when the patient first presented at our clinic. When decompression was performed, the clinical findings were similar to a cystic lesion and during follow the up period we found that lesion size decreased. Currently, mass properties have not been described in previous reports, and our case study presented with both radiographic and clinical similarities to cystic lesion symptoms; for these reasons our diagnosis was delayed. Additional reports have indicated that many cases of CCOC are misdiagnosed because of its rarity and similarity to cystic lesions11,13. In this report, we discuss a patient that presented with a painful cystic lesion, jaw enlargement jaw and loosening teeth. Similar cases should be considered for the possibility of malignant CCOC to identify and treat patients with CCOC.
Notes
References
1. Hansen LS, Eversole LR, Green TL, Powell NB. Clear cell odontogenic tumor--a new histologic variant with aggressive potential. Head Neck Surg. 1985; 8:115–123. PMID: 4077550.
2. Kramer IR, Pindborg JJ, Shear M. Histological typing of odontogenic tumours. Berlin: Springer;1992.
3. Barnes L. Pathology and genetics of head and neck tumours. Lyon: IARC Press;2005.
4. Kumar M, Fasanmade A, Barrett AW, Mack G, Newman L, Hyde NC. Metastasising clear cell odontogenic carcinoma: a case report and review of the literature. Oral Oncol. 2003; 39:190–194. PMID: 12509974.

5. Brinck U, Gunawan B, Schulten HJ, Pinzon W, Fischer U, Füzesi L. Clear-cell odontogenic carcinoma with pulmonary metastases resembling pulmonary meningothelial-like nodules. Virchows Arch. 2001; 438:412–417. PMID: 11355179.

6. Piattelli A, Sesenna E, Trisi P. Clear cell odontogenic carcinoma. Report of a case with lymph node and pulmonary metastases. Eur J Cancer B Oral Oncol. 1994; 30B:278–280. PMID: 7950843.

7. Fan J, Kubota E, Imamura H, Shimokama T, Tokunaga O, Katsuki T, et al. Clear cell odontogenic carcinoma. A case report with massive invasion of neighboring organs and lymph node metastasis. Oral Surg Oral Med Oral Pathol. 1992; 74:768–775. PMID: 1488233.
8. Bang G, Koppang HS, Hansen LS, Gilhuus-Moe O, Aksdal E, Persson PG, et al. Clear cell odontogenic carcinoma: report of three cases with pulmonary and lymph node metastases. J Oral Pathol Med. 1989; 18:113–118. PMID: 2746520.

9. Swain N, Dhariwal R, Ray JG. Clear cell odontogenic carcinoma of maxilla: A case report and mini review. J Oral Maxillofac Pathol. 2013; 17:89–94. PMID: 23798837.

10. Zhang J, Liu L, Pan J, Tian X, Tan J, Zhou J, et al. Clear cell odontogenic carcinoma: report of 6 cases and review of the literature. Med Oncol. 2011; 28(Suppl 1):S626–S633. PMID: 20827579.

11. Werle H, Blake FA, Reichelt U, Schmelzle R, Heiland M. Clear-cell odontogenic carcinoma: a new case and long-term follow-up of an old case, and review of the literature. J Oral Maxillofac Surg. 2009; 67:1342–1348. PMID: 19446231.

12. Ebert CS Jr, Dubin MG, Hart CF, Chalian AA, Shockley WW. Clear cell odontogenic carcinoma: a comprehensive analysis of treatment strategies. Head Neck. 2005; 27:536–542. PMID: 15772956.

13. Avninder S, Rakheja D, Bhatnagar A. Clear cell odontogenic carcinoma: a diagnostic and therapeutic dilemma. World J Surg Oncol. 2006; 4:91. PMID: 17156493.

14. Chaine A, Pitak-Arnnop P, Dhanuthai K, Bertrand JC, Bertolus C. An asymptomatic radiolucent lesion of the maxilla. Clear cell odontogenic carcinoma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009; 107:452–457. PMID: 19071036.
Fig. 1
Panoramic radiograph showing a defined radiolucent lesion in the right maxillary region (arrow).
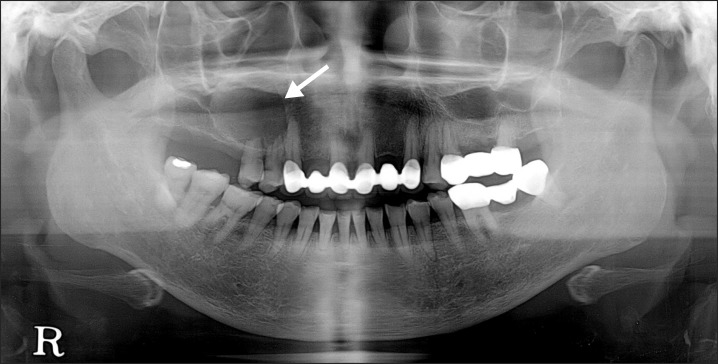
Fig. 2
Computed tomography image at first visit showed well defined and low attenuated cystic lesion on the right maxillary region.
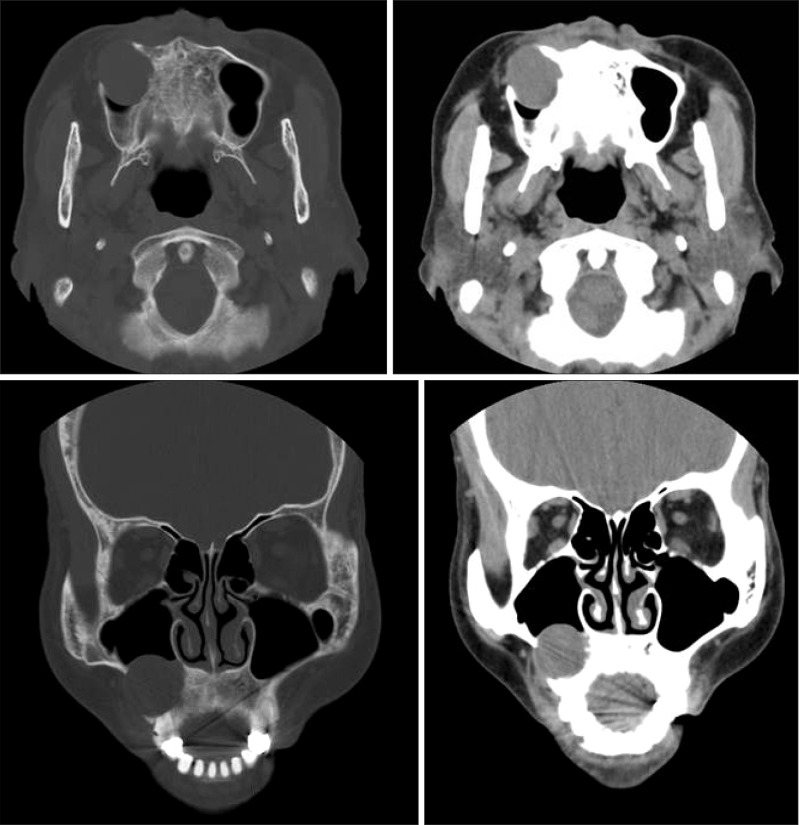
Fig. 3
Two month after decompression, a panoramic radiograph showed that a lesion size decreased, compared with previous radiograph (arrow).
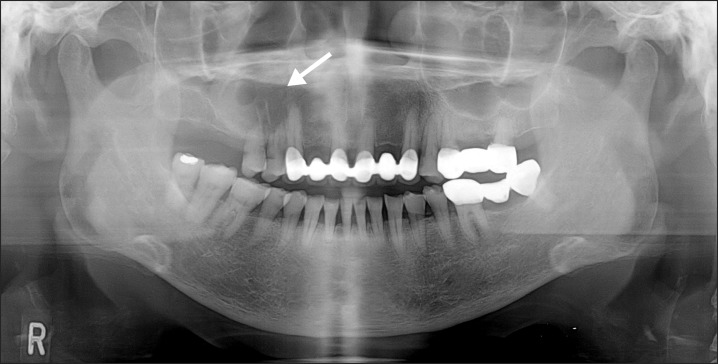
Fig. 5
Three-dimensional reconstruction image, image at first visit is on the left (lesion is indicated with black arrows) and image at 3-months after decompression is on the right (lesion is indicated with white arrows).
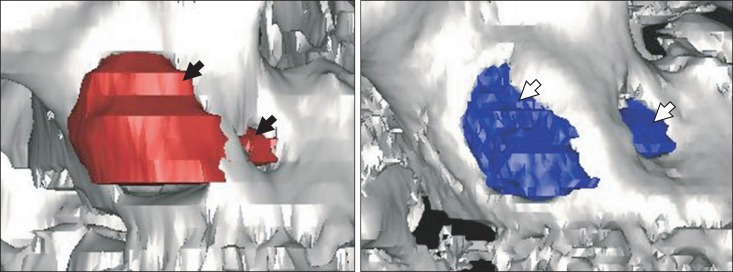
Fig. 6
Histopathologic findings. A. Histopathologic examination of the previous enucleation specimen revealed tumorous proliferation of epithelial nests infiltrating the stroma, indicating malignancy (H&E staining, ×100). B. Cuboidal shaped odontogenic cells were also noted among the tumorous clear cells (H&E staining, B: ×200, inset box: ×200). C. In the resected specimen, the tumor cells (T) infiltrated to the bone marrow of the maxilla (H&E staining, ×100). D. Lymphovascular permeation of tumor cells (arrowheads) (H&E staining, ×200).




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download