Abstract
Objectives
The purpose of this article is to evaluate factors influencing prognosis of arthrocentesis in patients with temporomandibular joint (TMJ) disorder.
Materials and Methods
The subjects included 145 patients treated with arthrocentesis at the Dental Center of Ajou University Hospital from 2011 to 2013 for the purpose of recovering mouth opening limitation (MOL) and pain relief. Prognosis of arthrocentesis was evaluated 1 month after the operation. Improvement on MOL was defined as an increase from below 30 mm (MOL ≤30 mm) to above 40 mm (MOL ≥40 mm), and pain relief was defined as when a group with TMJ pain with a visual analog scale (VAS) score of 4 or more (VAS ≥4) decreased to a score of 3 or more. The success of arthrocentesis was determined when either mouth opening improved or pain relief was fulfilled. To determine the factors influencing the success of arthrocentesis, the patients were classified by age, gender, diagnosis group (the anterior disc displacement without reduction group, the anterior disc displacement with reduction group, or other TMJ disorders group), time of onset and oral habits (clenching, bruxism) to investigate the correlations between these factors and prognosis.
Results
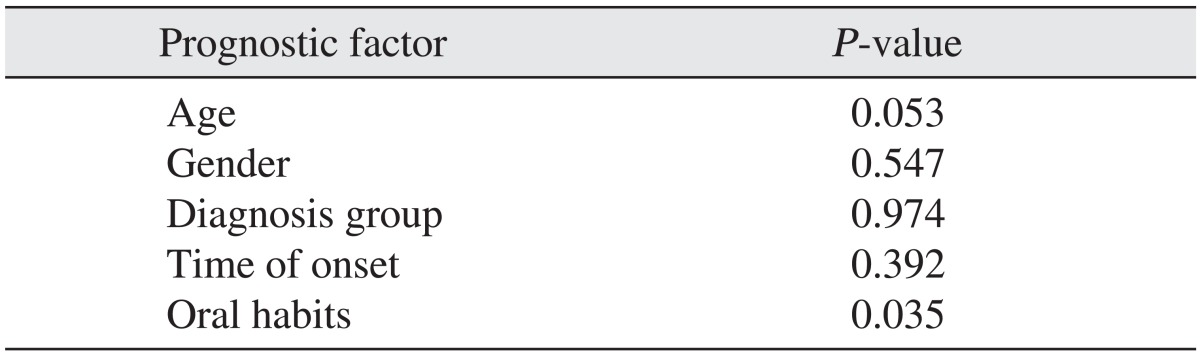
One hundred twenty out of 145 patients who underwent arthrocentesis (83.4%) were found to be successful. Among the influencing factors mentioned above, age, diagnosis and time of onset had no statistically significant correlation with the success of arthrocentesis. However, a group of patients in their fifties showed a lower success rate (ANOVA P=0.053) and the success rate of the group with oral habits was 71% (Pearson's chi-square test P=0.035).
Go to : 
Arthrocentesis is known to be an effective surgical approach to treating temporomandibular joint (TMJ) disorders. It is widely used to not only treat an acute closed lock but also for various TMJ disorders. In the early days, a simple lavage after local anesthesia of the superior joint space was performed to reset gliding of the articular disc and mouth opening for patients with a closed lock1. Numerous studies have been conducted by researchers, and this technique has been applied broadly, such as during injection of corticosteroids or sodium hyaluronate in the superior joint space. Arthrocentesis has been developed as a supplementary treatment method for internal derangement as well as a treatment method with satisfactory prognosis upon long-term observation. In addition, it has been recognized as being a very simple operation with nearly no complications.
Several studies have found that arthrocentesis is capable of recovering normal mouth opening and reducing pain and functional disorder. Brennan and Ilankovan2 stated that arthrocentesis is a relatively simple surgical procedure for patients with pain that cannot be improved by conservative treatments, and Lee and Yoon3 reported that the patients with TMJ internal derangement were successfully treated with a combination of arthrocentesis and stabilization splint therapy. Some researchers claim that arthrocentesis is effective for degenerative joint diseases including degenerative arthritis, while Al-Belasy and Dolwick4 state that arthrocentesis is only clearly effective for acute closed lock for a long period of time.
There have been a wide range of studies on the effectiveness of arthrocentesis, but the factors influencing the prognosis of the operation are not well known. When it comes to prognosis of arthrocentesis, a lot of influencing factors possibly exist. Thus, it is important to check for these factors as well as the indications and limitations of arthrocentesis.
In this regard, the present study examined the factors influencing prognosis of hospitalized patients who underwent arthrocentesis for TMJ disorder.
Go to : 
The subjects consisted of 145 patients with TMJ disorders accompanied by mouth opening limitation or pain, hospitalized at the Department of Oral and Maxillofacial Surgery, Dental Center in the Ajou University Hospital from January 2011 to January 2013, for arthrocentesis. This study was approved by the Institutional Review Board of Ajou University Hospital (MED-MDB-14-088). There were 145 patients in total who were included in the postoperative follow-up research. At each patient's first medical examination, a conservative treatment of medications and physical therapy was applied for around 2 weeks. However, when there was no improvement even after stabilization splint therapy, arthrocentesis was carried out.
During the operation, saline solution was used for cleaning, and around 1.5 mL of hyaluronic acid (Guardix-sol; Hanmi Pharm., Seoul, Korea) was injected.
In general, mouth opening limitation refers to the state in which the mouth cannot be opened within the normal range. Normal mouth opening may vary for every patient, but it is usually about 40 to 60 mm. The distance between the upper anterior teeth and the lower anterior teeth is measured5,6. The vertical mouth opening is larger in males. Many researchers have reported mouth opening limitations in a wide range of diseases7.
In the study, the maximum mouth opening was the distance between the incisal edges of the upper and lower central incisors (mm) and pain was recorded according to the visual analog scale (VAS) out of 10 (0, without pain; 10, intolerably severe pain). When the vertical space between the incisal edges of the upper and lower incisors when the mouth was opened at maximum was 30 mm or shorter, it was classified as mouth opening limitation, and when the mouth opening increased from below 30 mm to above 40 mm, it was regarded as an improvement in the mouth opening limitation. Using VAS, improvement in pain was determined as when more than 3 points are reduced from a score of 4 or greater. The effectiveness of arthrocentesis was evaluated 1 month after the operation, and when either mouth opening limitation was treated or pain was reduced, it was regarded as an effective treatment.
Postoperative predictive factors including the patient's gender, age, TMJ disorder type, time of onset and oral habits (clenching, bruxism) were used to classify the patients for analyses. The patients treated with arthrocentesis were divided into three groups-the anterior disc displacement (ADD) without reduction group, the ADD with reduction group, and the TMJ disorder (which included patients with pain from degenerative arthritis, capsulitis, synovitis and/or other) group. TMJ disorders that were present for more than 3 months were classified as chronic and the others as acute, and the groups were divided according to whether there were oral habits or not. Oral habits included clenching and bruxism. In the case of patients with oral habits, occlusal stabilizing splint therapy was used.
SPSS software version 17.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analyses of postoperative predictive factors. Independent variables included gender, age, TMJ disorder type, time of onset and oral habits and the dependent variable was the prognosis of arthrocentesis. For an analysis by age, the groups were divided by age group (for instance, the patients in their teens, twenties, thirties and so on) and Pearson chi-square analysis was used for analyses by gender, TMJ disorder type, time of onset and oral habits. Logistic regression analysis and ANOVA analysis were used for the analyses by age. The significance level of all statistical procedures was 0.05% for all variables under assessment.
Go to : 
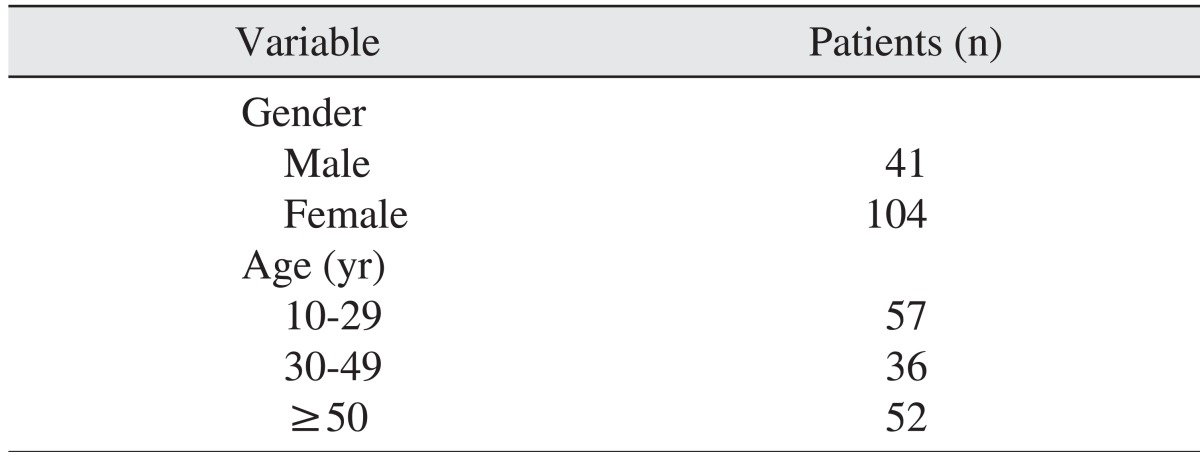
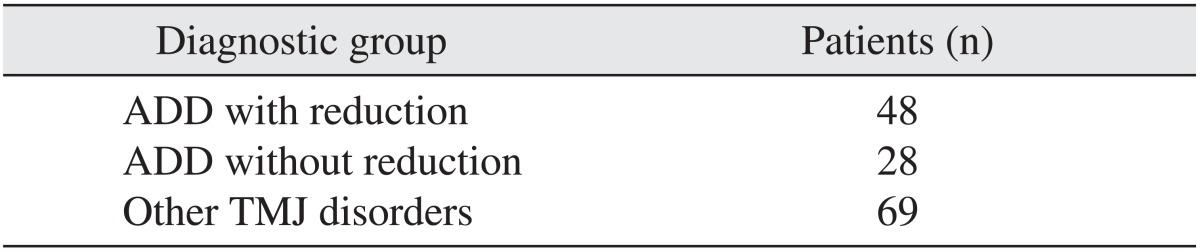
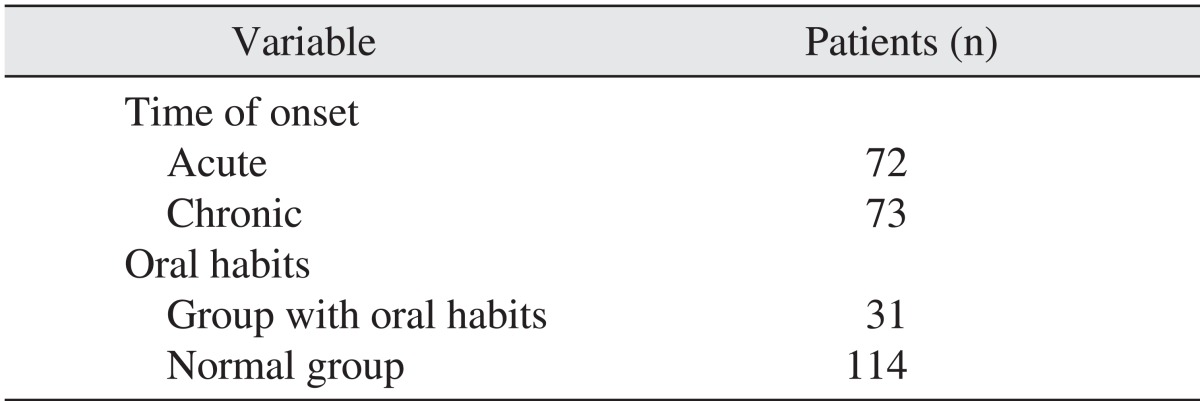
The subjects consisted of 41 male patients and 104 female patients (Table 1) with ages ranging from 13 to 66 years and the average age was 39.4 years. There were 57 patients from the 10 to 29 years group and 36 patients from the 30 to 49 years group and 52 patients who were older than 50 years.(Table 1) There were 48 patients in the ADD with reduction group, 28 patients in the ADD without reduction group and 69 patients in other TMJ disorders group.(Table 2) There were 72 patients with acute TMJ disorder and 73 patients with chronic TMJ disorder. There were 31 patients who had oral habits.(Table 3)
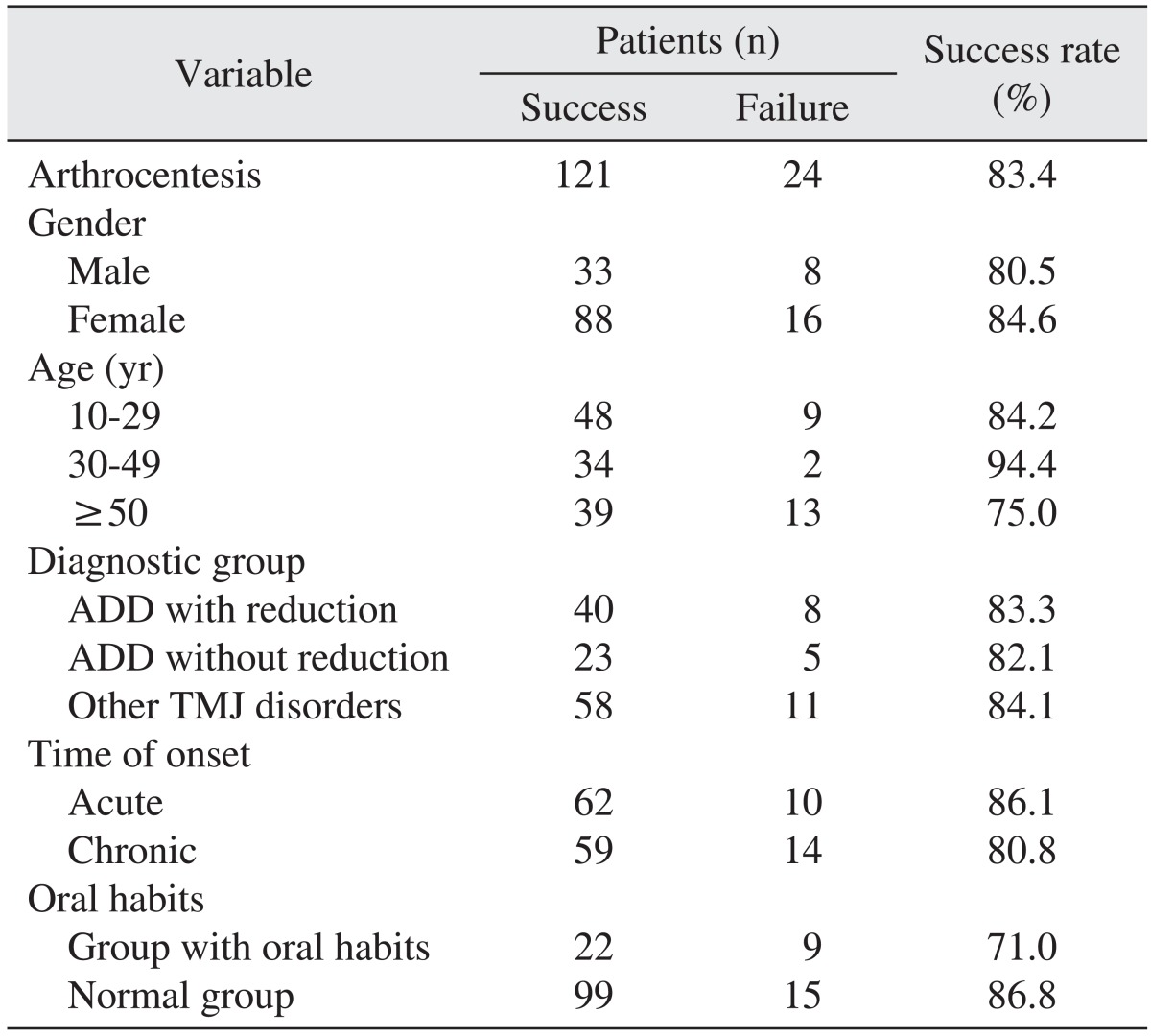
Among 145 patients with arthrocentesis, 121 patients claimed to have improvements, where the success rate was 83.4%. The success rate was 80.5% for male patients and 84.6% for female students, and 84.2% for the 10 to 29 years group, 94.4% for the 30 to 49 years group, and 75% for the ≥50 years group. According to the diagnostic group, the success rate was 83.3% for the ADD with reduction group, 82.1% for the ADD without reduction group and 84.1% for other TMJ disorders group. When it comes to the time of onset, the success rate was 86.1% for the acute onset group and 80.8% for the chronic onset group. The success rate of the group with oral habits was 71% and that of the group without oral habits was 86.8%.(Table 4) As a result of the prognostic factors significance test, age (P=0.053; P>0.05), gender (P=0.547; P>0.05), diagnostic group (P=0.974; P>0.05), time of onset (P=0.392; P>0.05), and the group with oral habits (P=0.035; P<0.05) were shown. A significant result was obtained from the group with oral habits.(Table 5) In terms of age, the patients were divided into six groups. The success rate of the 10 to 29 years group was around 80% on average, and increased to about 90% at the 30 to 49 years group. Then, it decreased to around 70% in the ≥50 years group. Thus, it could not be explained using a linear regression equation, making it statistically invalid upon logistic regression analyses. When the patients were divided into three groups-10 to 29 years, 30 to 49 years, and ≥50 years-the P-value was 0.053 by the ANOVA analysis, a figure approximate to the significance level of 0.05.
Go to : 
When a TMJ disorder occurs, the patients mainly suffer greatly from pain and mouth opening limitation. There have been many reports on the causes of this pain and mouth opening limitation, and several studies having examined synovial fluids.
Normal synovial fluid has an extremely small amount of protein owing to the selective permeability of the synovial sheath when compared to that of blood plasma. Here, albumin accounts for 60% to 75% of the proteins and a very small amount of globulin and transferrin exists. Also, hyaluronic acid is created by the cells near the synovial sheath, which plays an important role in the lubrication mechanism of TMJ. However, when inflammation occurs at the synovial sheath, the amount of protein increases as the permeability of the synovial sheath increases, as does and the amount of transferrin and immunoglobulin G. Moreover, the amount of hyaluronic acid decreases, due to the functional disturbance of cells8.
In particular, it is clinically significant that substance P and macromolecule fibrin, which are known as the materials that deliver pain, are found within the synovial fluid of the patients claiming chronic pain.
Considering that the friction between the articular disc and the superior joint space has a great impact on mandibular movement, it is believed that an inflammatory reaction caused by long-term external injury and changes to the secretion of synovial fluids caused by damages to the subsynovial tissue play a crucial role in the vicious cycle of pain and mouth opening limitation.
Alpaslan and Alpaslan9 suggested that it is more effective to inject hyaluronic acid during arthrocentesis for pain, mouth opening limitation and clicking sound. Hyaluronic acid is a macromolecular polysaccharide composed of a repeating disaccharide unit created by B-type synovial cells as well as the main component of synovial fluids. It plays an important role in joint lubrication and homeostasis at the articular joint space10,11. Hyaluronic acid included in the 1 to 2 µm layer of the joint cartilage surface is associated with the restoration of cartilage surfaces, and it acts as a buffer to protect the cartilage cells from trauma. It has been reported that hyaluronic acid removes free radicals, inhibits the creation of granulation tissue, supplies nutrients to the avascular parts of joints, reduces vascular permeability, deters migration of polymorphonuclear leukocytes and macrophages and encourages anti-inflammation-like phagocytosis12. In addition, Kim13 reported that hyaluronic acid has an analgesic effect. The study also took into consideration the benefits of hyaluronic acid when performing arthrocentesis.
Various studies have found that arthrocentesis can result in normal maximum mouth opening and a reduction in pain and inconvenience. The overall success rate shown in this study was 83.4%. This is higher than that reported by Murakami et al.14 (70%) and Hosaka et al.15 (79%), but lower than that reported by Nitzan et al.16 (91%, 95%).
In this study, it was discovered that arthrocentesis was effective for 120 out of 145 patients. Thus, it can be determined that arthrocentesis is capable of reducing pain and of improving mouth opening limitation. Age and the group with oral habits were notable prognosis determinants. Examining the success rate by age group, the average of the 10 to 29 years group was around 80%, increased to around 90% in the 30 to 49 years group, and decreased to around 70% in the ≥50 years group. The P-value upon statistical analyses with the three groups was 0.053 (ANOVA analysis, P>0.05), which was close to a statistically significant outcome. It is believed that age may impact the prognosis of arthrocentesis. In other words, the success rate of a group in their fifties may decrease. Also, the group with oral habits showed a low success rate of 71% (Pearson chi-square test P=0.035; P<0.05).
Murakami et al.14 concluded that age may be an influential factor in predicting the result of arthrocentesis, since the average age of failed cases was 39 years, which was somewhat higher than the average age of successful cases, which was 27 years. Nitzan et al.16 stated that more time is required for recovery of patients 40 years or older, and Guarda-Nardini et al.17 reported that arthrocentesis using hyaluronic acid is less effective for young patients under 45 years.
Nishimura et al.18 and Sakamoto et al.19 claimed that arthrocentesis is effective for patients suffering from ADD without reduction and is less effective when bony changes are detected at the mandibular condyle. Alpaslan et al.20 assumed that arthrocentesis is likely to be more effective for patients without bruxism.
Park et al.21 reported that arthrocentesis is more effective in improving mouth opening and reducing pain when used in conjunction with splint therapy.
In the study, it is assumed that the success rate of a group with oral habits before/after arthrocentesis is low since bad oral habits, including clenching and bruxism, reduce the therapeutic effect. Bruxsism is thought to be one of the major contributing factors to the aetiology of TMJ. Patients with myofacial pain dysfunction syndrome, and who are prone to clenching or bruxism, may develop disc derangements22. In this study, splint therapy was also performed for those in the group with oral habits to reduce forces directed at the TMJ as well as the intraarticular pressure. It is estimated that continuous stress in the disc and retrodiscal tissue during clenching and bruxism have an effect on the prognosis of arthrocentesis. There is limited information to judge whether splint therapy has a direct impact on arthrocentesis in this study.
Although our results did not meet our original standard of statistical significance, the success rates of the ADD without reduction group, the ADD with reduction group and other TMJ disorders group were high, and the success rate was high regardless of the onset of the TMJ disorder. These results confirmed that arthrocentesis is an effective treatment in reducing pain and improving mouth opening limitation.
Since prognosis of the operation was evaluated 1 month after arthrocentesis, the long-term success rate of the operation could not be checked.
Go to : 
Arthrocentesis is an effective treatment option that is tolerable by patients. Since it is less invasive than other surgical procedures, it can easily be done again, if required, and is recommended to surgeons treating patients with TMJ disorder. It was found in the study that arthrocentesis showed high success rates and was effective in recovering mouth opening and reducing pain. The factors influencing the prognosis of the operation may be diverse and complex. However, the success rate of arthrocentesis in patients in their fifties or older is likely to be low. Also, it was discovered that arthrocentesis may be less effective when the patients have bad oral habits.
Go to : 
References
1. Nitzan DW, Dolwick MF, Martinez GA. Temporomandibular joint arthrocentesis: a simplified treatment for severe, limited mouth opening. J Oral Maxillofac Surg. 1991; 49:1163–1167. PMID: 1941330.

2. Brennan PA, Ilankovan V. Arthrocentesis for temporomandibular joint pain dysfunction syndrome. J Oral Maxillofac Surg. 2006; 64:949–951. PMID: 16713811.

3. Lee SH, Yoon HJ. MRI findings of patients with temporomandibular joint internal derangement: before and after performance of arthrocentesis and stabilization splint. J Oral Maxillofac Surg. 2009; 67:314–317. PMID: 19138604.

4. Al-Belasy FA, Dolwick MF. Arthrocentesis for the treatment of temporomandibular joint closed lock: a review article. Int J Oral Maxillofac Surg. 2007; 36:773–782. PMID: 17582743.

6. Nelson SJ, Nowlin TP, Boeselt B. Consideration of linear and angular values of maximum mandibular opening. Compendium. 1992; 13:362. 364. 366 passim. PMID: 1521281.
7. Dworkin SF, Huggins KH, LeResche L, Von Korff M, Howard J, Truelove E, et al. Epidemiology of signs and symptoms in temporomandibular disorders: clinical signs in cases and controls. J Am Dent Assoc. 1990; 120:273–281. PMID: 2312947.

8. Yi AN, Han SY, Yun KI. Clinical aspect of arthrocentesis. J Korean Assoc Oral Maxillofac Surg. 2000; 26:97–104.
9. Alpaslan GH, Alpaslan C. Efficacy of temporomandibular joint arthrocentesis with and without injection of sodium hyaluronate in treatment of internal derangements. J Oral Maxillofac Surg. 2001; 59:613–618. PMID: 11381380.

10. Fraser JR, Clarris BJ, Baxter E. Patterns of induced variation in the morphology, hyaluronic acid secretion, and lysosomal enzyme activity of cultured human synovial cells. Ann Rheum Dis. 1979; 38:287–294. PMID: 384932.

11. Balazs EA. The physical properties of synovial fluid and the special role of hyaluronic acid. In : Helfet AJ, editor. Disorders of the Knee. Philadelphia: Lippincott;1974. p. 61–64.
12. Rydell N, Balazs EA. Effect of intra-articular injection of hyaluronic acid on the clinical symptoms of osteoarthritis and on granulation tissue formation. Clin Orthop Relat Res. 1971; 80:25–32. PMID: 5002457.

13. Kim JJ. The effect of intra-articular injection of hyaluronic acis after arthrocentesis in treatment of internal derangements of the TMJ. J Korean Assoc Oral Maxillofac Surg. 2006; 32:453–457.
14. Murakami K, Hosaka H, Moriya Y, Segami N, Iizuka T. Short-term treatment outcome study for the management of temporomandibular joint closed lock. A comparison of arthrocentesis to nonsurgical therapy and arthroscopic lysis and lavage. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995; 80:253–257. PMID: 7489265.
15. Hosaka H, Murakami K, Goto K, Iizuka T. Outcome of arthrocentesis for temporomandibular joint with closed lock at 3 years follow-up. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996; 82:501–504. PMID: 8936512.

16. Nitzan DW, Samson B, Better H. Long-term outcome of arthrocentesis for sudden-onset, persistent, severe closed lock of the temporomandibular joint. J Oral Maxillofac Surg. 1997; 55:151–157. PMID: 9024352.

17. Guarda-Nardini L, Olivo M, Ferronato G, Salmaso L, Bonnini S, Manfredini D. Treatment effectiveness of arthrocentesis plus hyaluronic acid injections in different age groups of patients with temporomandibular joint osteoarthritis. J Oral Maxillofac Surg. 2012; 70:2048–2056. PMID: 22907107.

18. Nishimura M, Segami N, Kaneyama K, Suzuki T. Prognostic factors in arthrocentesis of the temporomandibular joint: evaluation of 100 patients with internal derangement. J Oral Maxillofac Surg. 2001; 59:874–877. PMID: 11474440.

19. Sakamoto I, Yoda T, Tsukahara H, Morita S, Miyamura J, Yoda Y, et al. Clinical studies of arthrocentesis of the temporomandibular joint: analysis of clinical findings in patients with a good outcome. Jpn J Oral Maxillofac Surg. 1996; 42:808–814.
20. Alpaslan C, Dolwick MF, Heft MW. Five-year retrospective evaluation of temporomandibular joint arthrocentesis. Int J Oral Maxillofac Surg. 2003; 32:263–267. PMID: 12767872.

21. Park YH, Lee SH, Yoon HJ. An effect of combination with arthrocentesis and stabilization splint treatment on temporomandibular joint disorder patient. J Korean Assoc Maxillofac Plast Reconstr Surg. 2010; 32:32–36.
22. Ghanem WA. Arthrocentesis and stabilizing splint are the treatment of choice for acute intermittent closed lock in patients with bruxism. J Craniomaxillofac Surg. 2011; 39:256–260. PMID: 20598897.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download