Abstract
This following case report describes the open reduction, internal fixation and the reconstruction of an extensive comminuted mandibular fracture with bilateral condylar fractures in a 19-year-old male patient with an intellectual disability and autistic disorder. He suffered fall trauma, resulting in shattered bony fragments of the alveolus and mandibular body between both mandibular rami, the fracture of both condyles and the avulsion or dislocation of every posterior tooth of the mandible. The patient underwent open reduction and internal fixation between both mandibular rami using a reconstruction plate, open reduction and internal fixation of the shattered fragments using miniplates and screws, and the closed reduction of the bilateral condylar fractures.
Comminuted fracture is defined as the presence of multiple fracture lines resulting in many small pieces within the same area of the mandible (e.g., angle, body, ramus, or symphysis)1. In extensive communited fractures, multiple sites (exceeding one region and involving the neighbouring region) of the mandible are splintered, crushed, pulverized, or broken into several pieces1,2. Extensive comminuted mandibular fractures occur when a high-energy impact is applied onto a region of the mandible. The high-energy impact seen in gun shots, traffic accidents, and falls can lead to enough concentrated force on the mandible to cause multiple sites of comminuted fractures3,4.
Traditionally, extensive comminuted mandibular fractures have been considered to be indications for closed reduction in order to avoid periosteal stripping and devascularization of the comminuted bone segments5. In the last 30 years, however, there has been a change in the treatment perspective of such injuries driven by advancements in rigid fixation techniques2. Some reports3,5,6,7 insist that open reduction and internal fixation is a better treatment option and causes lower complication rates than closed reduction in some comminuted mandibular fractures. However, it is still controversial whether closed reduction is the optimal treatment for comminuted fractures as compared to open reduction and internal fixation.
The decision for the proper treatment can be complicated when condylar fractures accompany the comminuted mandibular fracture. Closed reductions with long-term limitation of mouth opening are beneficial for comminuted fracture, but are harmful for condylar fractures.
There are two types of condylar fractures, intracapsular and extracapsular, but for practical purposes, the anatomical level of the fracture is divided into three sites: the condylar head (intracapsular), the condylar neck (extracapsular), and the subcondylar region8,9,10. Condylar fractures are usually caused by traffic accidents, falls, and violence8. Teeth injuries such as fractures and luxations are frequently accompanied with condylar head or neck fractures. Concomitant fractures of the mandibular body often accompany subcondylar fractures and are more frequently bilateral than unilateral11.
In the treatment of condylar fractures, there are conservative methods such as closed reduction with concomitant physical therapy, and surgical methods using open reduction and internal fixation. Like other mandibular fractures, the treatment of condylar fractures is controversial12. For conservative methods using closed reduction, early mouth mobilization is essential to prevent adhesion or ankylosis of the temporomandibular joint (TMJ).
This article reports a case of extensive comminuted mandibular fracture with bilateral condylar fractures treated by open reduction, internal fixation, and reconstruction, and discusses the indications and benefits of treatment options.
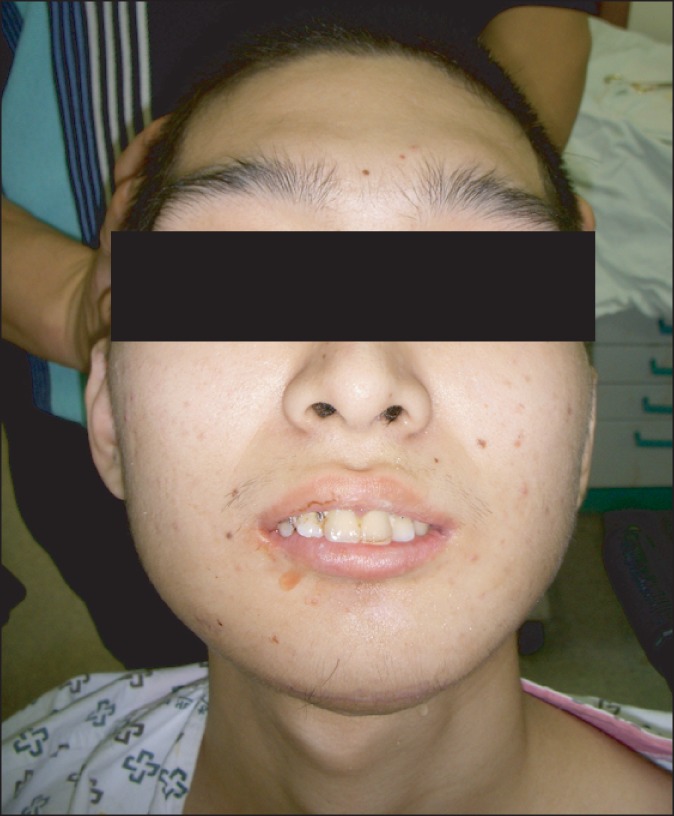
A 19-year-old male who was in the care of an institution for the disabled due to an intellectual disability and autistic disorder visited the emergency room at Inje University Ilsan Paik Hospital (Goyang, Korea) after a fall. His injury included extensive comminuted mandibular fracture between both angles, bilateral condylar fractures, the avulsion or dislocation of all posterior teeth in the mandible, and shattered bony fragments of the alveolus and mandible body. Accordingly, there was a defect of mandible continuity and occlusion was absent.(Fig. 1) His facial injuries were accompanied by fractures on the right tibia and ankle. To make matters worse, his psychological state made it impossible for him to maintain stabilization of his jaws for closed reduction and his tibial fracture kept him on strict bed rest.
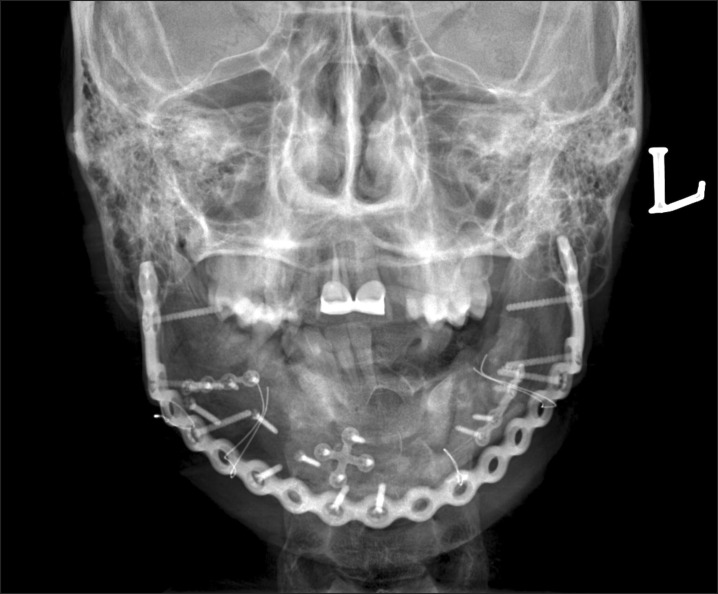
Under general anesthesia, open reduction and internal fixation of the mandibular comminuted fracture were performed using a locking reconstruction plate, mini-plates and screws. A locking reconstruction plate (Stryker-Leibinger, Kalamazoo, MI, USA) was adjusted and fixed to both rami with screws. Marginal bone segments were reduced and fixed to the reconstruction plate with screws. Small or non-marginal bone segments were reduced and fixed to each other and marginal bone with mini-plates and screws. Soft tissue were attached to the periosteum and sutured with vicryl. The closed reduction of both condylar fractures was followed by maxillomandibular fixation with steel wires between the arch-bar on the maxillary teeth and the reconstruction plate on the mandible.(Fig. 2)
Two weeks later, the maxillomandibular fixation steel wires were released and the patient started mouth-opening exercises for condyle rehabilitation to prevent TMJ complications. Twenty millimeters of mouth opening was measured. The patient was allowed a liquid diet per oral and wheelchair ambulation four weeks after the operation. After six weeks, 23 mm of mouth opening was measured (Fig. 3) and favorable bone healing and soft tissue maturation were observed.(Fig. 4) After 10 weeks, the patient was able to have a diet of soft-to-mildly hard solids, and more than 30 mm of mouth opening was measured. Although it was impossible to achieve panoramic radiographs and computed tomography due to the patient's psychological problems, infections or bone necrosis were not observed, and signs of non-union were not found on plain radiographs and clinical examination up to this time.(Fig. 5)
Reconstruction of the mandible continuity and rehabilitation of oral functions like dieting and mouth opening recovered without significant complications.
More follow-up hospital visits were not possible due to personal reasons, although his condition was reported over the phone by his guardian. Any specific complications involving the mandible did not occur for more than one year.
Comminuted mandibular fractures have been treated by several methods: closed reduction, external pin fixation, internal wire fixation, and open reduction and internal fixation. It has been debated whether closed reduction or open reduction and internal fixation is the proper treatment for comminuted mandibular fractures. For extensive comminuted mandibular fractures, closed reduction has long been considered to be the optimal treatment to preserve blood supply to the bone fragments and to prevent secondary infections. However, since Kazanjian6 described the open reduction and internal fixation of mandibular comminuted fractures 60 years ago, it has been reported that open reduction and internal fixation is a better treatment with lower complication rates than closed reduction in comminuted mandibular fractures. Furthermore, there have been remarkable advancements in fixation materials and techniques. As a result, open reduction and internal fixation tends to be the contemporary treatment of choice.
A recent report by Smith and Teenier5 suggested that open reduction and internal fixation in cases of comminuted mandibular fractures are indicated (a) in severe injuries with significant displacement to allow for the restoration of the pre-traumatic anatomic relationships, (b) in the edentulous and partially edentulous patient who does not have stable occlusion and may benefit from the open reduction and internal fixation of comminuted fractures, and (c) in cases with multiple fractures of the midface, in which the mandible serves as a guide to reposition the midfacial bones. The authors also proposed that closed reduction or conservative treatment is a better choice for minimally displaced comminuted fractures.
The healing of displaced or dislocated condylar fractures requires the remodeling of the condyles. Remodeling can be understood as a process directed to meet the demands of function and growth, and occurs in such a way to allow for the functional adaptation to condylar rotation without translation. For dislocated or severely displaced condylar heads, the remodeling process configures the head parallel to the frontal plane13.
For condylar fractures, conservative treatment is the treatment of choice for the majority of fractures8. In general, early mouth opening exercises (i.e., the early mobilization of the jaw and functional rehabilitation) is essential for the treatment of condylar fractures14. Adhesion, fibrosis, and ankylosis of the condyle can occur after long periods of maxillomandibular fixation15.
Zachariades et al.8 proposed several guidelines for treating condylar fractures, including: 1) "Displaced condylar fractures with altered occlusion may be satisfactorily treated in 50% of cases with intermaxillary fixation. In cases with displaced fractures, maxilla-mandibular fixation should always be used, even if the occlusion is unchanged on admission. An open reduction, however, may be required." 2) "Absolute indications for non-surgical treatment are intracapsular condylar fractures, high condylar fractures close to or involving the articular surface, and fractures in growing children." 3) "Conservative treatment may be required when the patient's past medical history does not allow the administration of general anesthesia." 4) "Open reduction is recommended for condylar fractures (especially on one side of bilateral fractures) associated with fracture(s) elsewhere in the mandible and/or involving comminuted maxillary fractures. If open reduction and rigid internal fixation is to be used for other mandibular or maxillary fractures, it may also be used for subcondylar fractures to avoid intermaxillary fixation." 5) "Open reduction is recommended when it is impossible to achieve pre-traumatic or adequate occlusion by closed reduction, in cases where conservative therapy has failed, and in anterior open bite results".
Titanium plates and screws are mostly used for internal fixation, and the plate systems widely used are 1.3, 1.5, and 2.0 mm miniplate systems for ordinary fractures and 2.4 and 2.7 mm reconstruction plates systems for comminuted fractures16. A mandibular reconstruction bone plate can be used to bridge the comminution gap and stabilize the most proximal and distal segments. If major fractured fragments are immobilized, other minor fragments between the major segments can heal well even if unfixed7. There are two designs of plate-screw locking systems, with the convention being non-locking and the other being locking. Non-locking systems achieve stability by the compression between the screw head compassed-plate and the screw-bone interface, which requires anatomically reduced fragments and precisely fitted plates. The drawbacks of this system are the possibility of primary reduction-loss in cases with incompletely adapted plates and disturbances of the blood supply to the compressed cortex. In the latter system, the screw head is locked at both threads of the plate and bone, creating no compression between the plate and bone. This system can produce more rigid construction with less distortion of the reduced fragments and less hindrances to blood circulation. Its merits include: (1) less precision required in plate adaptation, (2) less alterations in reduced bone segments and the occlusal relationship on screw tightening, (3) greater stability across the fracture site, (4) less screw loosening16,17. For the reasons above, the locking reconstruction plate system can be a valid internal fixation tool for the treatment of comminuted mandibular fractures.
In this case, because the fracture was so severe and widespread, discontinuity of the mandible occurred so it could be treated by either closed reduction or open reduction and internal fixation. However, there were several problems that made closed reduction less feasible for this patient. First, all of the patient's posterior teeth were avulsed or excessively dislocated, the alveolus was fractured, and stable occlusion was completely absent. Second, both condylar fractures caused retraction of the mandible and early mouth opening exercises were required to avoid adhesion of the condyles, but could not be practically achieved under closed reduction. Finally, patient cooperation was difficult to achieve because of his psychological state. From these reasons, the oral and maxilla-facial surgery team concluded that this comminuted mandibular fracture was an indication for open reduction and internal fixation. In the report by Smith and Teenier5, a partially edentulous state without stable occlusion was a suggested indication for open reduction and internal fixation, and early mouth opening exercises after open reduction and internal fixation are essential for TMJ rehabilitation. In this case, open reduction and internal fixation with reconstruction and a short period of maxillomandibular fixation were the treatment of choice. Considering the limitations of this one case and the short follow-up period, we suggest that open reduction and internal fixation with a reconstruction plate can be a satisfactory treatment option in extensive comminuted mandibular fracture with bilateral condylar fractures.
References
1. Finn RA. Treatment of comminuted mandibular fractures by closed reduction. J Oral Maxillofac Surg. 1996; 54:320–327. PMID: 8600240.

2. Chrcanovic BR. Open versus closed reduction: comminuted mandibular fractures. Oral Maxillofac Surg. 2013; 17:95–104. PMID: 22842858.

3. Li Z, Li ZB. Clinical characteristics and treatment of multiple site comminuted mandible fractures. J Craniomaxillofac Surg. 2011; 39:296–299. PMID: 20605726.

4. Alpert B, Tiwana PS, Kushner GM. Management of comminuted fractures of the mandible. Oral Maxillofac Surg Clin North Am. 2009; 21:185–192. PMID: 19348983.

5. Smith BR, Teenier TJ. Treatment of comminuted mandibular fractures by open reduction and rigid internal fixation. J Oral Maxillofac Surg. 1996; 54:328–331. PMID: 8600241.

6. Kazanjian VH. An outline of the treatment of extensive comminuted fractures of the mandible: based chiefly on experience gained during the last war. Am J Orthod Oral Surg. 1942; 28:B265–B274.
7. Ellis E 3rd. Treatment of mandibular angle fractures using the AO reconstruction plate. J Oral Maxillofac Surg. 1993; 51:250–254. PMID: 8445465.

8. Zachariades N, Mezitis M, Mourouzis C, Papadakis D, Spanou A. Fractures of the mandibular condyle: a review of 466 cases. Literature review, reflections on treatment and proposals. J Craniomaxillofac Surg. 2006; 34:421–432. PMID: 17055280.

9. MacLennan WD. Fractures of the mandibular condylar process. Br J Oral Surg. 1969; 7:31–39. PMID: 5258903.

10. Marker P, Nielsen A, Bastian HL. Fractures of the mandibular condyle. Part 1: patterns of distribution of types and causes of fractures in 348 patients. Br J Oral Maxillofac Surg. 2000; 38:417–421. PMID: 11010766.

11. Lindahl L. Condylar fractures of the mandible. I. Classification and relation to age, occlusion, and concomitant injuries of teeth and teeth-supporting structures, and fractures of the mandibular body. Int J Oral Surg. 1977; 6:12–21. PMID: 402318.
12. Choi KY, Yang JD, Chung HY, Cho BC. Current concepts in the mandibular condyle fracture management part II: open reduction versus closed reduction. Arch Plast Surg. 2012; 39:301–308. PMID: 22872831.

13. Dahlström L, Kahnberg KE, Lindahl L. 15 years follow-up on condylar fractures. Int J Oral Maxillofac Surg. 1989; 18:18–23. PMID: 2497204.

14. Ellis E, Throckmorton GS. Treatment of mandibular condylar process fractures: biological considerations. J Oral Maxillofac Surg. 2005; 63:115–134. PMID: 15635566.

15. Beekler DM, Walker RV. Condyle fractures. J Oral Surg. 1969; 27:563–564. PMID: 4978291.
16. Pereira CC, LetíciaDos Santos P, Jardim EC, Júnior IR, Shinohara EH, Araujo MM. The use of 2.4-mm locking plate system in treating comminuted mandibular fracture by firearm. Craniomaxillofac Trauma Reconstr. 2012; 5:91–96. PMID: 23730424.

17. Collins CP, Pirinjian-Leonard G, Tolas A, Alcalde R. A prospective randomized clinical trial comparing 2.0-mm locking plates to 2.0-mm standard plates in treatment of mandible fractures. J Oral Maxillofac Surg. 2004; 62:1392–1395. PMID: 15510361.

Fig. 1
Preoperative images of computed tomography axial view and three-dimensional reconstruction view. There are scattered fragments of mandible andposterior teeth.
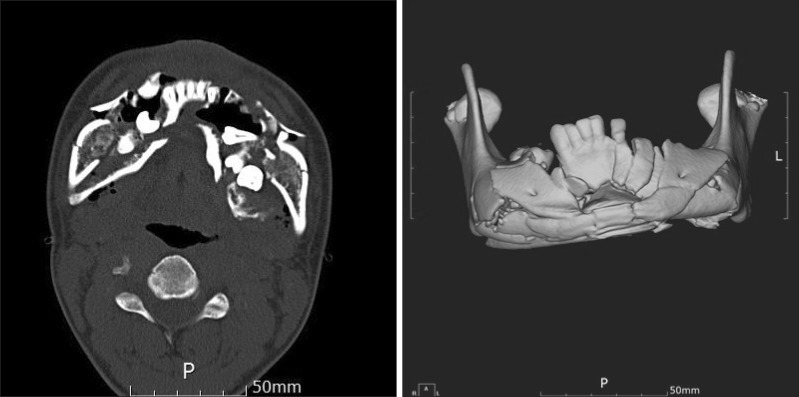
Fig. 2
Intraoperative photo showing a reconstruction plate, miniplates and screws used for internal fixationand steel wires used for maxillomandibular fixation.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download