Abstract
Objectives
The aim of this study was to evaluate the pattern of lingual split line when performing a bilateral sagittal split osteotomy (BSSO) for asymmetric prognathism. This was accomplished with the use of cone-beam computed tomography (CBCT) and three-dimensional (3D) software program.
Materials and Methods
The study group was comprised of 40 patients (20 males and 20 females) with asymmetric prognathism, who underwent BSSO (80 splits; n=80) from January 2012 through June 2013. We observed the pattern of lingual split line using CBCT data and image analysis program. The deviated side was compared to the contralateral side in each patient. To analyze the contributing factors to the split pattern, we observed the position of the lateral cortical bone cut end and measured the thickness of the ramus that surrounds the mandibular lingula.
Results
The lingual split patterns were classified into. The true "Hunsuck" line was 60.00% (n=48), and the bad split was 7.50% (n=6). Ramal thickness surrounding the lingual was 5.55±1.07 mm (deviated) and 5.66±1.34 mm (contralateral) (P=0.409). The position of the lateral cortical bone cut end was classified into three types: A, lingual; B, inferior; C, buccal. Type A comprised 66.25% (n=53), Type B comprised 22.50% (n=18), and Type C comprised 11.25% (n=9).
Conclusion
In asymmetric prognathism patients, there were no differences in the ramal thickness between the deviated side and the contralateral side. Furthermore, no differences were found in the lingual split pattern. The lingual split pattern correlated with the position of the lateral cortical bone cut end. In addition, the 3D-CT reformation was a useful tool for evaluating the surgical results of BSSO of the mandible.
Go to : 
Bilateral sagittal split osteotomy (BSSO) is one of the most common orthognathic surgical procedures for the correction of mandibular deformities. The Obwegeser-Dal Pont osteotomy and Hunsuck modifications are widely used1-3. When performing BSSO, it is crucial to control the lingual split because it may result in an unfavorable fracture or inferior alveolar nerve (IAN) damage.
Conventional radiographs, such as panoramic views and cephalograms, have limitations in regard to evaluation of the lingual split pattern. Using cone-beam computed tomography (CBCT) and three-dimensional (3D) reconstruction, we can obtain a view of the lingual aspect of the mandible. Plooij et al.4 and Muto et al.5 evaluated the mandibular ramus split pattern in a symmetric mandible using 3D-CT.
In an asymmetric mandible, the morphology and anatomy of each side differ. The length of the ramus and body, the inclination of the ramus, and the ramal volume are significantly different between the deviated side and the contralateral side6,7.
We hypothesized that a different split pattern would occur in asymmetric mandibular prognathism. Therefore, the aim of this study was to evaluate the lingual split line when performing BSSO in asymmetric mandibular prognathism; we used CBCT and a 3D software program. We also determined the contributing factors that affect the lingual split pattern.
Go to : 
The study group comprised 40 patients with asymmetric mandibular prognathism (20 males and 20 females) who had undergone BSSO from January 2012 through June 2013 in Pusan National University Dental Hospital. Patients' age ranged from 18 to 31 years (mean age: 23.2 years). The inclusion criterion comprised chin deviation >3 mm compared to the facial midline (mean deviation: 5.7 mm; right/left: 17/23). The exclusion criterion was a syndromic mandibular deformity. The surgical procedure employed was the Obwegeser-Dal Pont-Hunsuck method. Two junior oral-maxillofacial surgeons performed horizontal, sagittal, and vertical osteotomies. One senior surgeon split the ramus. The presence of a third molar was also evaluated. This study protocol was approved by Institutional Review Board of Pusan National University Dental Hospital, Yangsan, Korea (PNUDH-2013-036).
Preoperative and postoperative CBCT images were acquired using DCT pro (Vatech Co., Hwaseong, Korea). The images were post-processed to a Digital Imaging and Communications in Medicine (DICOM) 3.0 file (Simplant; Materialise Inc., Leuven, Belgium). A 3D image analysis program was used to reconstruct the 3D images. The mandible was digitally isolated from the maxilla and skull and split up the midline. The deviated and contralateral sides of the mandible were rotated along the vertical axis to visualize the lingual surface of the ramus.
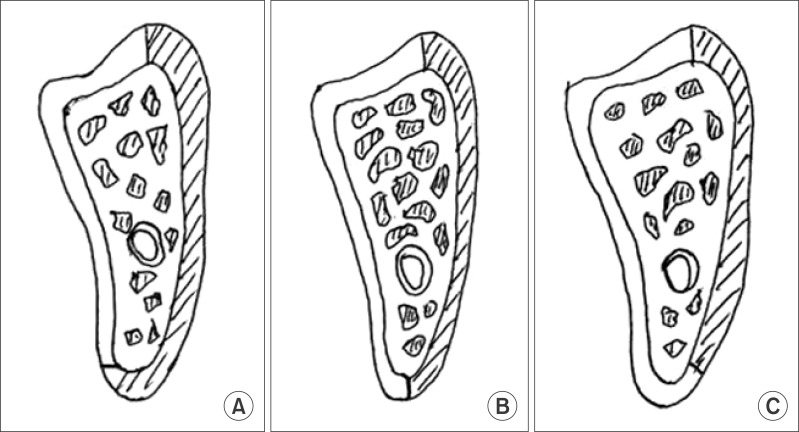
Prior to taking measurements, reference planes were established. The Frankfort horizontal plane was set as the horizontal reference plane, and the mid-sagittal plane was set as the sagittal plane.(Fig. 1. A, 1. B) Measurements were performed at the level of the mandibular lingula which is the reference point for horizontal osteotomy.(Fig. 1. C)
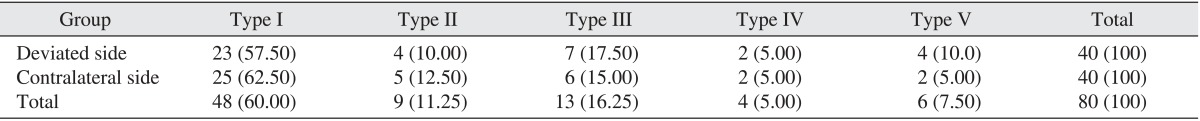
To evaluate contributing factors, we observed the position of the lateral cortical bone cut end using 3D reconstructed images. We categorized the lateral cortical bone cut end into three types. Type A was positioned lingually, Type B was inferior, and Type C was located on the buccal side of the mandibular inferior border.
All statistical analyses were conducted with PASW Statistics 18.0 (IBM Co., Armonk, NY, USA). To evaluate intraobserver reliability, the kappa-coefficient was used for the lingual split pattern and the vertical osteotomy end. Following the measurement of the ramal thickness, a paired t-test was performed to identify any significant differences between the deviated side and the contralateral side. All parameters were measured twice by one examiner 48 hours apart using the paired t-test for intraobserver reliability.
Go to : 
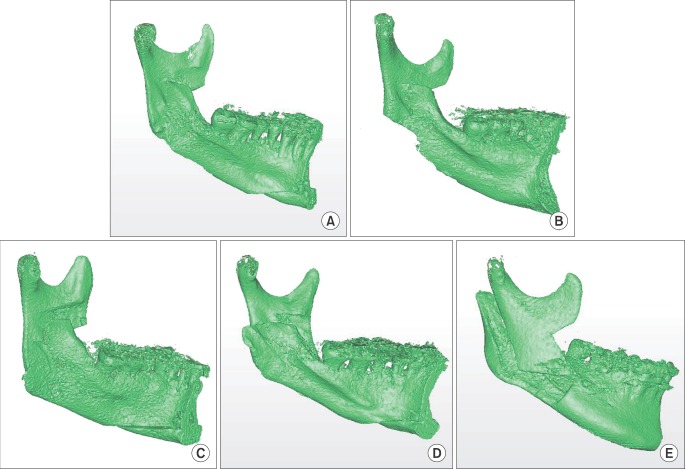
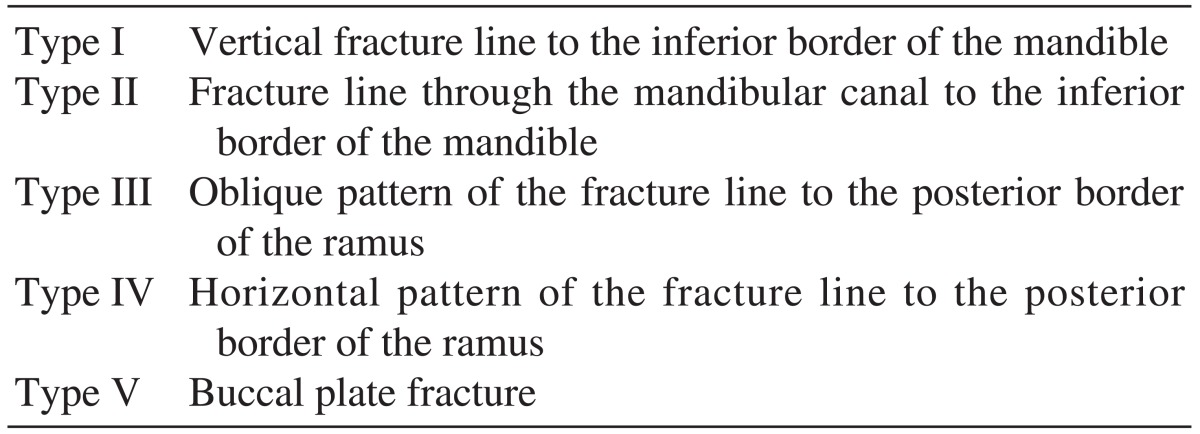
The lingual split line pattern was categorized into five groups according to the path of the fracture line on the lingual surface of the ramus.(Table 1, Fig. 2) The kappa-coefficient of the intraobserver reliability was 0.91 (P=0.000). Intended split pattern (Type I) comprised 60.00% (n=48). Type II, III, and IV accounted for 11.25% (n=9), 16.25% (n=13), and 5.00% (n=4), respectively, and a bad split (Type V) occurred in 7.50% (n=6). There was no split pattern difference between the deviation and contralateral sides.(Table 2)
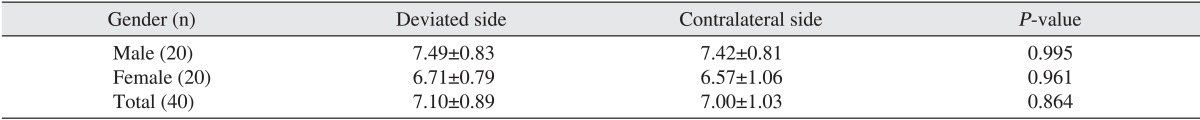
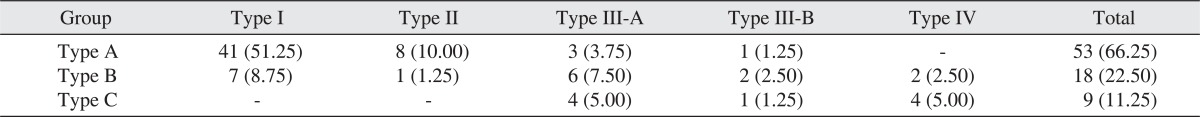
The ramal thickness at the level of the mandibular lingula was measured. On the deviated side, the mean thickness was 7.10±0.89 mm. On the opposite side, it was 7.00±1.03 mm. No significant difference was found between thicknesses on the deviated and the contralateral sides (P<0.864); however, males had a statistically significant difference in ramal thickness.(Table 3) The position of the lateral bone cut end was related to the lingual split pattern. In Type A, Type I was predominant (41/48), and Type V was absent. However, in Type C, the buccal side end was observed in types III, IV, and V.(Table 4, Fig. 3)
Go to : 
BSSO is a widely used orthognathic surgical procedure for the correction of mandibular deformities. Since its initial description by Obwegeser, modified procedures proposed by Dal Pont and Hunsuck are currently in common usage1-3. The Hunsuck's modification advocates extending the horizontal osteotomy to just behind the lingula3. The important aspect of this technique is that it safely separates the proximal and distal segments in an intended direction; it is difficult to identify the separation pattern precisely using a conventional cephalogram or a panoramic view.
CBCT and 3D reconstruction software provide effective means for evaluation of the facial skeleton and are currently used in large-scale studies of the maxillofacial region8,9. Due to its 3D mandibular bone reconstruction capability, CBCT enables accurate assessment of the lingual surface of the ramus, which is hard to evaluate with traditional radiography. We were able to identify the lingual split line created during BSSO.
The 3D evaluation of the lingual split line pattern in a BSSO procedure was first reported by Plooij et al.4 They categorized the lingual split line pattern of 40 consecutive patients with symmetric mandibular hypoplasia who underwent advanced BSSO into four groups. Only 51% of the splits coursed as described by Hunsuck3; 13% extended to the posterior border, 33% coursed along the outer side of the mandibular canal, and 2.5% had an unfavorable split pattern. He noted the length and position of the medial bone cut during horizontal osteotomy and reported that the likelihood of splitting according to Hunsuck's description increases when the bone cut end lies behind the mandibular foramen; however, it decreases if the bone cut end extends through the mandibular canal.
A study of mandibular prognathism performed by Muto et al.5 reported a relatively high prevalence among Asian populations. Thirty patients were categorized into five types of lingual split patterns, and 33% were in the range of Hunsuck's description; however, 15% suffered a buccal fracture. The most important factor influencing such a split tendency is the location of the lateral bone cut end during vertical osteotomy; the lateral bone cut was on the buccal side of all incidences of buccal fracture.
In Korean orthodontic patients, class III malocclusion is predominant. In particular, the incidence of facial asymmetry with skeletal class III is 42.3%10,11. Three dimensional analysis of patients with asymmetric prognathism has been reported by many studies. The deviated side appears to have a shorter ramal and body length than the contralateral side; in addition, it has a smaller degree of ramal inclination, measured in the sagittal plane, and a smaller ramal volume6,7,12,13. These measurements are based on orthodontic reference points or landmarks; however, information regarding the thickness of the ramus or its relationship with the IAN, which should be considered for BSSO, cannot be obtained. The aim of this study was to evaluate whether the lingual split line pattern during BSSO in patients with asymmetric mandibular prognathism is affected by anatomic differences.
We observed that there was no differences in the split pattern between the deviated and the contralateral sides; 60% of split lines were Type I, in agreement with Hunsuck's description, and 7.5% had an unfavorable fracture. To verify contributing factors, ramal thickness and the location of the lateral bone cut end were investigated. Ramal thickness was not significantly different between the deviated side (mean: 7.10 mm) and the contralateral side (mean: 7.00 mm). In addition, the split pattern and the ramal thickness were not correlated. Yamamoto et al.14 measured the distance from the mandibular canal to the buccal cortex and the distance from the mandibular lingula to the inferior border of the ramus. In cases where the distance was <0.8 mm, the incidence of neurosensory disturbance increased significantly. For a medial osteotomy, we measured the ramal thickness only at the level of lingula; however, the need to evaluate the entire ramus following the split requires further investigation. The lateral cortical bone cut end had a correlation with the split pattern. In case of Type I, Type A was the most common (41/48). In addition, six cases of Type V (either Type B or Type C) were observed; these results concurred with those of Muto et al.'s study5.
Lee et al.15 studied mandibular body anatomy in patients with asymmetric prognathism. In that study, the distance from the mandibular canal to the buccal cortex was not significantly different between deviated and contralateral sides. Wolford and Davis16 reported the use of a reciprocating saw to cut the inferior border of the mandible, without using a mallet, to achieve mandible splitting. With preoperative CBCT and a 3D program to locate the lateral bone cut end lingually, it is important to analyze the cross-sectional view of the mandible, the pathway of the IAN, and the distance between the mandibular canal and buccal cortex.
Other studies17-19 have reported an incidence of bad splits during BSSO ranging from 0.9% to 20%; the incidence in this study was 7.5% (6 splits). The risk factors for bad splits were old age, the presence of a third molar, a thin mandibular ramus, a high mandibular lingula, and an incomplete split of the inferior border of mandible20-23. In this study, in six cases of unfavorable fracture, the factors were presence of a third molar (2 cases), a high mandibular lingula (2 cases), and a buccaly-positioned lateral bone cut end (2 cases).
Go to : 
This study was conducted to evaluate whether there is any difference in the split pattern that occurs with BSSO in an asymmetric mandible. Pre- and post-operative CBCT data and a 3D reconstruction program were used to analyze the lingual split pattern, lateral bone cut end, and to measure the thickness of the ramus.
1. We categorized the lingual split pattern of the asymmetric prognathic mandible into five types, and there were no differences in split pattern.
2. The ramal thickness, which was measured at the level of the lingula was not significantly different between the deviated and contralateral sides. In addition, no correlation between ramal thickness and split pattern was found.
3. The lateral bone cut end was categorized into three types; a correlation with ramal thickness and split pattern was found.
Go to : 
References
1. Trauner R, Obwegeser H. The surgical correction of mandibular prognathism and retrognathia with consideration of genioplasty. I. Surgical procedures to correct mandibular prognathism and reshaping of the chin. Oral Surg Oral Med Oral Pathol. 1957; 10:677–689. PMID: 13441284.
2. Dal Pont G. Retromolar osteotomy for the correction of prognathism. J Oral Surg Anesth Hosp Dent Serv. 1961; 19:42–47. PMID: 13719390.
3. Hunsuck EE. A modified intraoral sagittal splitting technic for correction of mandibular prognathism. J Oral Surg. 1968; 26:250–253. PMID: 5237786.
4. Plooij JM, Naphausen MT, Maal TJ, Xi T, Rangel FA, Swennnen G, et al. 3D evaluation of the lingual fracture line after a bilateral sagittal split osteotomy of the mandible. Int J Oral Maxillofac Surg. 2009; 38:1244–1249. PMID: 19713076.

5. Muto T, Takahashi M, Akizuki K. Evaluation of the mandibular ramus fracture line after sagittal split ramus osteotomy using 3-dimensional computed tomography. J Oral Maxillofac Surg. 2012; 70:e648–e652. PMID: 23078827.

6. Baek SH, Cho IS, Chang YI, Kim MJ. Skeletodental factors affecting chin point deviation in female patients with class III malocclusion and facial asymmetry: a three-dimensional analysis using computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007; 104:628–639. PMID: 17656131.

7. You KH, Lee KJ, Lee SH, Baik HS. Three-dimensional computed tomography analysis of mandibular morphology in patients with facial asymmetry and mandibular prognathism. Am J Orthod Dentofacial Orthop. 2010; 138:540.e1–540.e8. PMID: 21055584.

8. Klinge B, Petersson A, Maly P. Location of the mandibular canal: comparison of macroscopic findings, conventional radiography, and computed tomography. Int J Oral Maxillofac Implants. 1989; 4:327–332. PMID: 2639861.
9. Kondo T, Ong SH, Foong KW. Computer-based extraction of the inferior alveolar nerve canal in 3-D space. Comput Methods Programs Biomed. 2004; 76:181–191. PMID: 15501505.

10. Yang WS. The study on the orthodontic patients who visited department of orthodontics, Seoul National University Hospital during 10 years (1985-1994). Korean J Orthod. 1995; 25:497–509.
11. Yoon KS, Jung YS, Kang GC, Park HS. Facial asymmetry with mandibular prognathism: a new trial of classification and interpretation. J Korean Assoc Oral Maxillofac Surg. 2004; 30:108–120.
12. Kwon TG, Park HS, Ryoo HM, Lee SH. A comparison of craniofacial morphology in patients with and without facial asymmetry--a three-dimensional analysis with computed tomography. Int J Oral Maxillofac Surg. 2006; 35:43–48. PMID: 15925488.

13. Kwon TG, Lee KH, Park HS, Ryoo HM, Kim HJ, Lee SH. Relationship between the masticatory muscles and mandibular skeleton in mandibular prognathism with and without asymmetry. J Oral Maxillofac Surg. 2007; 65:1538–1543. PMID: 17656280.

14. Yamamoto R, Nakamura A, Ohno K, Michi KI. Relationship of the mandibular canal to the lateral cortex of the mandibular ramus as a factor in the development of neurosensory disturbance after bilateral sagittal split osteotomy. J Oral Maxillofac Surg. 2002; 60:490–495. PMID: 11988921.

15. Lee JY, Kim YI, Hwang DS, Kim YD, Shin SH, Kim UK, et al. Cross-sectional study of the mandibular body in patients with facial asymmetry. J Korean Assoc Oral Maxillofac Surg. 2011; 37:109–113.

16. Wolford LM, Davis WM Jr. The mandibular inferior border split: a modification in the sagittal split osteotomy. J Oral Maxillofac Surg. 1990; 48:92–94. PMID: 2294218.

17. MacIntosh RB. Experience with the sagittal osteotomy of the mandibular ramus: a 13-year review. J Maxillofac Surg. 1981; 9:151–165. PMID: 6974211.

18. Turvey TA. Intraoperative complications of sagittal osteotomy of the mandibular ramus: incidence and management. J Oral Maxillofac Surg. 1985; 43:504–509. PMID: 3859593.

19. Panula K, Finne K, Oikarinen K. Incidence of complications and problems related to orthognathic surgery: a review of 655 patients. J Oral Maxillofac Surg. 2001; 59:1128–1136. PMID: 11573165.

20. Guernsey LH, DeChamplain RW. Sequelae and complications of the intraoral sagittal osteotomy in the mandibular rami. Oral Surg Oral Med Oral Pathol. 1971; 32:176–192. PMID: 5284103.

21. Veras RB, Kriwalsky MS, Hoffmann S, Maurer P, Schubert J. Functional and radiographic long-term results after bad split in orthognathic surgery. Int J Oral Maxillofac Surg. 2008; 37:606–611. PMID: 18515045.

22. Akhtar S, Tuinzing DB. Unfavorable splits in sagittal split osteotomy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999; 87:267–268. PMID: 10102582.

23. Chrcanovic BR, Freire-Maia B. Risk factors and prevention of bad splits during sagittal split osteotomy. Oral Maxillofac Surg. 2012; 16:19–27. PMID: 21837430.

Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download