II. Case Report
A 71-year-old female patient visited Seoul National University Hospital's Emergency Room complaining of headache and 5-hour-long fever of 39.4℃. She said she could not chew any food because of pain in the right temporomandibular joint area ever since the extraction of the upper right 2nd molar at a local clinic a month ago. At the time of admission, both white blood cells and C-reactive protein counts were high with values of 14,100/cm3 and 22.33 mg/dL, respectively. The serum lipid component value as well as blood urea nitrogen and creatine values were within the normal range. The blood and urine cultures did not show any aerobic or anaerobic bacteria. Moreover, the lumbar puncture result did not indicate any sign of meningitis; neither did the chest postero-anterior radiograph (PA) reveal any significant finding.
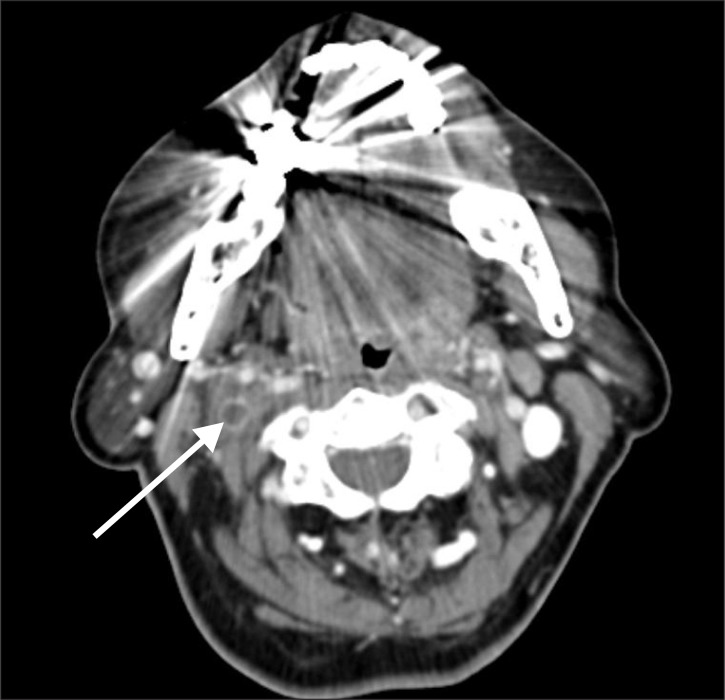
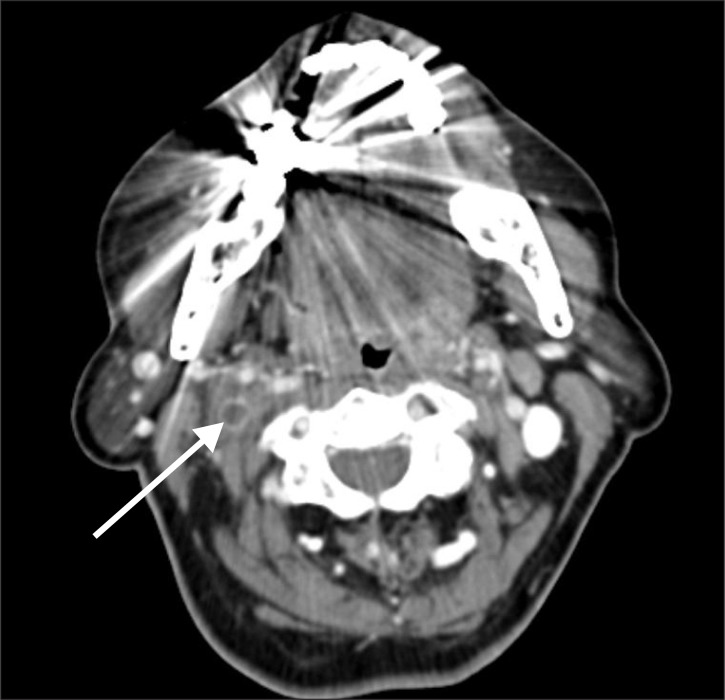
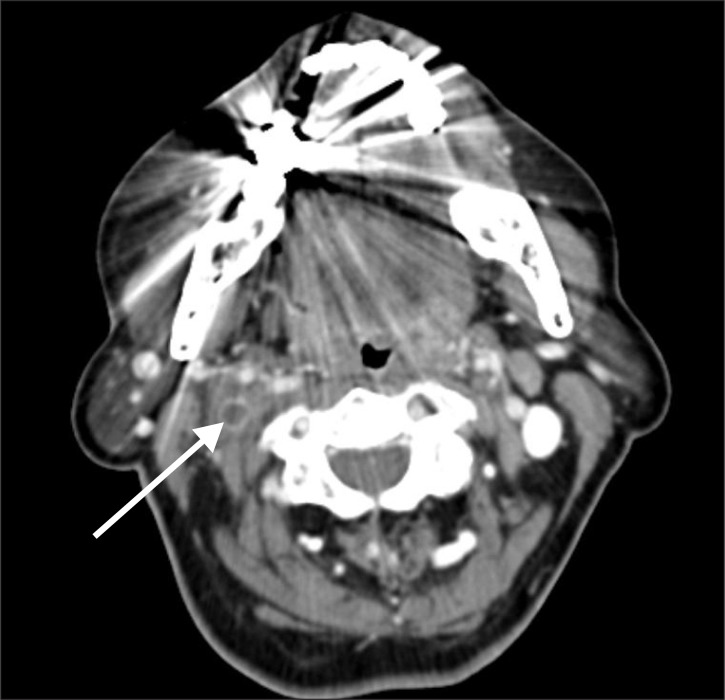
Even though the chest computed tomography (CT) and abdominal CT did not show any significant finding, enhanced neck CT showed thrombosis from the right internal jugular vein to the right sigmoid sinus vein.(
Figs. 1,
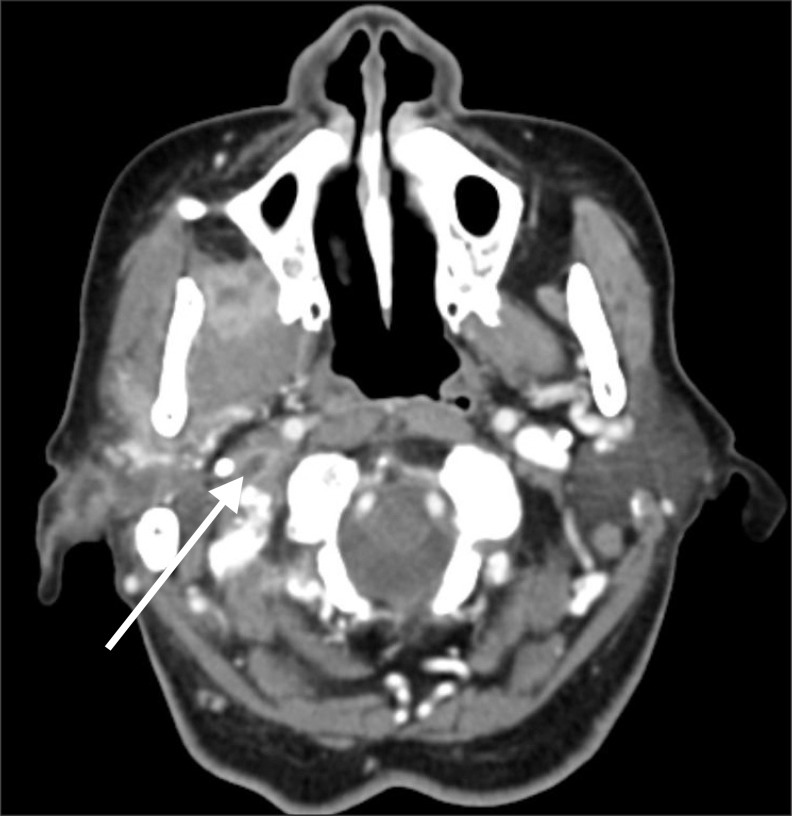
2) Additionally, in posterior nasal spine (PNS) CT images, abscess formation was suspected in the internal aspect of the right ramus as well as in the anterior aspect of the right condyle. In enhanced images of PNS magnetic resonance imaging (MRI), pervasive infection with abscess formation could be seen in the right masticatory and parotid areas.(
Fig. 3) Clinically, the vestibule in the right maxillary molar area was swollen, but abscess discharge or formation of fistula was not observed. To treat severe infection in the right masticatory and parotid areas, amoxicillin clavulanate 1.2 g was administered intravenously every 8 hours in addition to metronidazole 500 mg every 12 hours.
 | Fig. 1Contrast-enhanced neck computed tomography showing thrombosis in the right internal jugular vein (arrow). 
|
 | Fig. 2Contrast-enhanced neck computed tomography showing thrombosis in the right sigmoid sinus (arrow). 
|
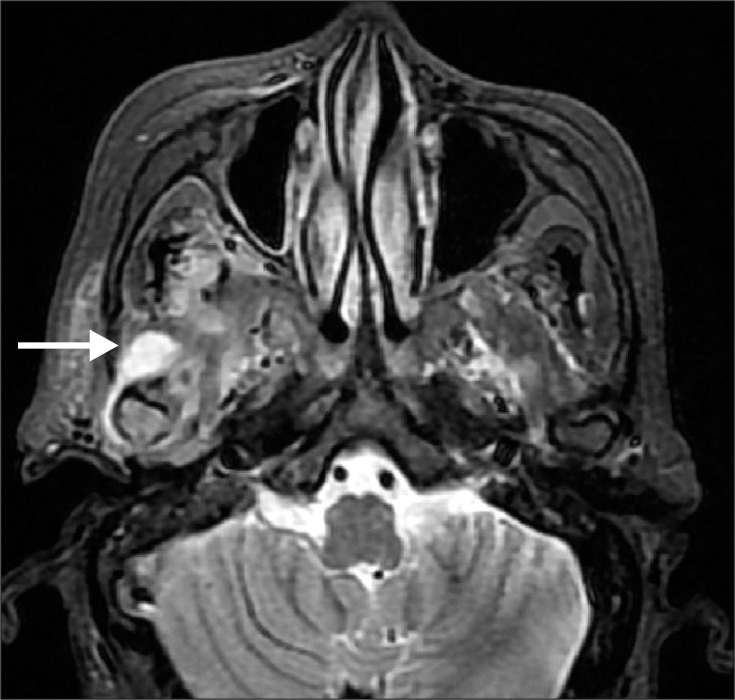 | Fig. 3Contrast-enhanced magnetic resonance imaging showing pervasive infection with abscess formation could be seen in the right masseteric and parotid (arrow). 
|
The following day, she was transferred to Department of Oral and Maxillofacial Surgery in Seoul National University Dental Hospital to undergo incision and drainage procedure under general anesthesia. During the procedure, a copious amount of pus was discharged from the infratemporal, pterygomandibular, and masseteric areas; the result of the pus culture was negative, however. At three days' post-operation, metrodinazole was stopped, and continued infusion of amoxicillin clavulanate was done intravenously. From the day of the surgery, the incision and drainage sites with penrose drains were irrigated copiously twice a day with disposable syringe containing sterile saline. From the 5th day, penrose drains were shortened, and those without any discharge were discarded. The patient was discharged on the 7th day; she visited the hospital one and two weeks after her discharge, without any significant finding. Maximum mouth opening increased considerably, and she no longer complained of any symptom of infection.
Go to :

III. Discussion
As gram-negative anaerobic bacterium,
Fusobacterium necrophorum is considered the major culprit of Lemierre syndrome. Whereas gram-negative bacteria causes sepsis in elderly patients with numerous systemic diseases
2, Lemierre syndrome caused by
F. necrophorum mostly afflicts healthy young adults with oro-pharyngeal infections or those who inject contaminated needles into their internal jugular veins for illegal drug usage. Unlike most reported cases, the patient in this case report was an elderly female without any systemic disease.
Chirinos et al.
3 reported that
F. necrophorum is the culprit of Lemierre syndrome in 81.7% of the cases, but that no bacteria could be cultured in the remaining 12.8%. In this case, no bacteria could be cultured by pus culture. The authors believe that this was due to antibiotic administration before the pus culture. According to Drool et al.
4 and Lai et al.
5, other bacteria such as
Fusobacterium sp.,
Bacteroids sp.,
Peptostreptococcus,
group B and
C streptococcus,
Streptococcus oralis, and
Eikenella corrodens could be found in patients suffering from this syndrome. Therefore, unlike Lemierre's report in 1936, bacteria other than
F. necrophorum can cause Lemierre syndrome.
Palatine tonsil is believed to be the origin of Lemierre syndrome in more than 90% of the cases
4,
6. Other possible causes of this syndrome are dental infection, parotiditis, mastoditis, and otitis media
6. In this case, the origin was dental infection subsequent to the extraction of the upper right 2nd molar. The authors believe that the infection invaded the parapharyngeal area, consequently infecting the carotid sheath. The anatomical structures included in the sheath are the internal jugular vein, carotid artery, vagus nerve, and lymph nodes. Moreover, glossopharyngeal, accessory, and hypoglossal nerves travel in the upper part of the carotid sheath. When these structures are infected, thrombophlebitis in the internal jugular vein, carotid artery erosion, X-XII palsies, or Horner's syndrome may develop.
Chirinos et al.
3 investigated cases of Lemierre syndrome for the past 20 years via MEDLINE search and discovered that 72% of 109 patients suffered from thrombophlebitis of the internal jugular vein. Even though thrombophlebitis is reported to occur on the opposite side
7, thrombophlebitis usually develops on the side of the infection origin. There is no conclusion on the pathway of infection to the internal jugular vein; Baig et al.
8, theorized that infection travels through the lymph channels
1, whereas Dool et al.
4 suggested that it spreads via paratonsil veins. Thrombophlebitis of the internal jugular vein is reported to develop approximately one week after the onset of infection
8,
9. In this case, thrombosis in the right internal jugular vein was observed in the neck CT images. Thrombosis was on the same side of infection in the right masseteric and pterygomandibular areas. One distinguishing aspect of the patient was the pervasive thrombosis from the internal jugular vein to the right sigmoid sinus.
According to Stam
10, approximately 3-4 people in one million suffer from thrombosis of the cerebral veins and sinuses Even though its incidence is extremely rare, it is accom panied by serious complications such as edema, infarction of the brain, and increased intracranial pressure
10. In particular, increased intracranial pressure results in headache, vomiting, altered level of consciousness, etc. The patient in our case complained of constant headache in the right occipital lobe area for two weeks, implying that she was suffering from thrombosis of cerebral veins and sinuses; this was substantiated by neck CT images. The patient was sent to the Department of Neurology for evaluation. The Department of Neurology determined that treating the abscess and cellulitis should be done first with close observation of the patient's blood pressure and state of hydration. They did not use anticoagulation due to its controversial nature. Moreover, they determined that there was no high risk of venous infarction with thrombus in the patient's internal jugular vein. There is no definitive treatment protocol for thrombophlebitis of the internal jugular vein; conclusive scientific data or research are not available. The treatment options of thrombophlebitis are anticoagulation and ligature of the affected vein. The prognosis of the usage of anticoagulation for thrombosis of the internal jugular vein or sigmoid sinus and ligature of the internal jugular vein is not known. Anticoagulation may shorten the recovery time by dissolving thrombus, but the dissolved thrombus can invade other vital anatomical structures
10,
11. Therefore, caregivers should be vigilant when using anticoagulation medications. Dool et al.
4 and Hoehn
12 said that anticoagulation is not recommended if there is no cerebral palsy and/or no thrombus invasion in the cavernous sinus. There are no scientific data or research available on the efficacy of ligature of the internal jugular vein in treating thrombophlebitis in the vein. Anticoagulation and ligature of the internal jugular vein can be deferred as the final options when antibiotics are not successful in treating the patient
13.
Even though the severity of the patient's headache at the right occipital lobe area subsided after the incision and drainage procedure, the patient still suffered from headache even up to the day of her discharge. During the one-month follow-up visit, the patient mentioned that she no longer suffered from headache; the patient's headache can be assumed to have originated not with thrombus but in the primarily infected site and infection.
Thrombophlebitis in the internal jugular vein can travel to other organs in the body, resulting in secondary infections. Thrombus can easily spread to the lungs or liver from the internal jugular vein through the superior vena cava. Metastasis can result in suppurative arthritis, meningitis, cerebral infarction, thrombosis in carotid artery, mediastinitis with pericardial tam ponade, liver abscess, osteomyelitis, thrombosis of cavernous sinus, etc
14-
16.
The typical chief complaints of patients suffering from the syndrome are fever and headache. Moreover, infection in the masseteric and pterygomandibular areas causes trismus and difficulty in swallowing. Moreover, inflammation of the internal jugular vein can cause pain upon palpation of the anterior aspect of the sternocleidomastoid muscle. If either lung is infected secondarily, difficulty in breathing and chest pain may develop
5,
11. According to Edibam et al.
14, more than 75% of the patients complain of abdominal pain with liver hypertrophy and jaundice as thrombus invades the liver. This illustrates that the symptoms of patients suffering from Lemierre syndrome may vary, and that diagnosing the syndrome accurately may pose a challenge. In our case, the patient had trismus of 5 mm, fever, and headache but no other symptoms. When there is abscess formation in the pterygomandibular area, trismus can occur without any facial swelling; therefore, if a patient has trismus, whether the patient is suffering from abscess or cellulitis of the pterygomandibular area should be checked, including whether he/she shows signs and symptoms of Lemierre syndrome.
Since this syndrome is not commonly known, and its differential diagnosis is difficult, appropriate treatments are not usually provided immediately; definitive diagnosis is possible only with radiographic images. CT, MRI, and ultrasounds are various methods of visualizing thrombo phlebitis of the internal jugular vein. Ultrasonography with Doppler can be utilized, but contrast-enhanced CT is generally recommended
17. CT images not only offer information on the origin of the infection and secondary lesions but also display thrombophlebitis as negative defects in the internal jugular vein. If there are nodules in the lungs in the chest CT images, septic emboli can be suspected
15. If the contrasted CT image does not show any pathology, digital subtraction angiography or retrograde venography can be utilized, but caution is required since it is invasive. In our case, enhanced PNS CT, MRI, and enhanced neck CT were taken to diagnose the syndrome and evaluate the primary and secondary lesions.
The treatment of choice is surgical drainage of the primary infection focus source and usage of appropriate antibiotics. Even though there is no definitive treatment protocol for thrombophlebitis of the internal jugular vein, there is a need to drain surgically the infection origin as well as the secondarily infected anatomical structures. Appropriate antibiotics are clindamycin, metrodinazole, antipseudomonal penicillin, and penicillin-sulbactam
3-
6,
9,
11. The combined usage of penicillin and metrodinazole increases the potency, resulting in greater effect; this combination of antibiotics was utilized in the treatment in our case. The gold standard in the duration of usage of antibiotics in treating Lemierre syndrome is not known, but authors recommend that it be long enough for the penetration of antibiotic into thrombophlebitis in the internal jugular vein, lung, or liver
18.
During the course of treatment, patients should be carefully monitored for sepsis or metastasis. The occurrence of sepsis might indicate that the current treatments are not sufficient in treating the syndrome, suggesting the utilization of more invasive procedures such as anticoagulation and ligature of the internal jugular vein. If metastasis is suspected, new radiographs should be taken, and surgical drainage should be performed immediately.
When a patient visits a dental clinic complaining of trismus, abscess and cellulitis of masticatory areas should be suspected, and Lemierre syndrome should be ruled out based on proper imaging modalities and clinical signs and symptoms.
Lemierre syndrome is caused by infection in the oropharyngeal region with subsequent thrombophlebitis in the internal jugular vein. In our case report, we have presented the case of a 71-year-old female patient with Lemierre syndrome with thrombophlebitis extended to the right sigmoid sinus from the right internal jugular vein. Even though thrombus in the cranial veins and sinuses could have worsened the prognosis, the patient was successively treated with conservative treatments, i.e., incision and drainage of primarily affected regions and antibiotic administration.
Oral and maxillofacial surgeons who frequently encounter infections in oro-pharyngeal regions are required to know not only the signs and symptoms of Lemierre syndrome but also the proper diagnostic methods and available treatment options. Moreover, they should be aware of the possibility and complications of metastasis of thrombophlebitis from the internal jugular vein to other vital anatomical structures.
Go to :