Abstract
Objectives
This study evaluated implant success rate, survival rate, marginal bone resorption of implants, and material resorption of sinus bone graft in cases wherein tapered body implants were installed.
Materials and Methods
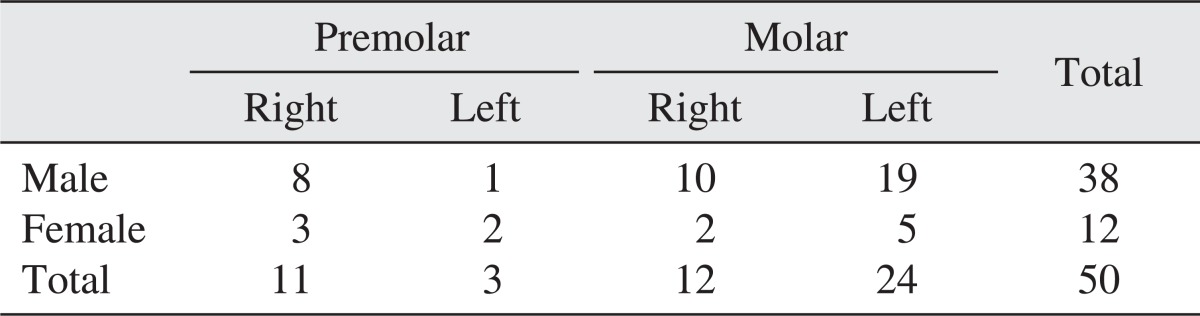
From September 2003 to January 2006, 20 patients from Seoul National University Bundong Hospital, with a mean age of 54.7 years, were considered. The mean follow-up period was 19 months. This study covered 50 implants; 14 implants were placed in the maxillary premolar area, and 36 in the maxillary molar area; 24 sinuses were included.
Results
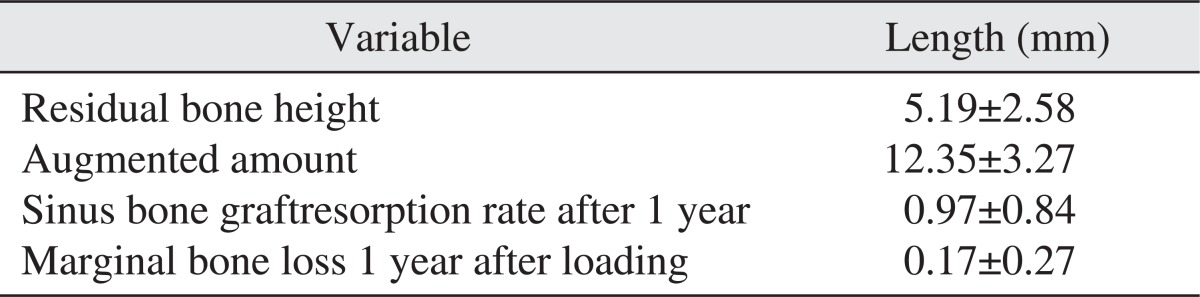
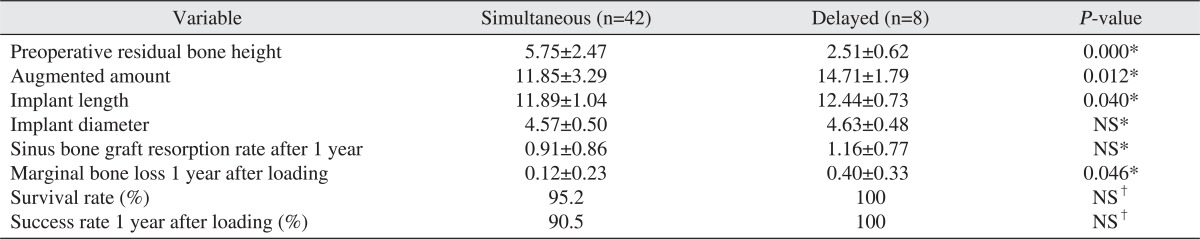
The success rate was 92%, and the survival rate was 96.0%. The mean amount of sinus augmentation was 12.35±3.27 mm. The bone graft resorption rate one year after surgery was 0.97±0.84 mm; that for the immediate implantation group was 0.91±0.86 mm, and that for the delayed implantation group was 1.16±0.77 mm. However, the difference was not statistically significant. The mean marginal bone resorption one year after restoration was 0.17±0.27 mm (immediate group: 0.12±0.23 mm; delayed group 0.40±0.33 mm); statistically significant difference was observed between the two groups.
The implant restoration of maxillary posterior regions is difficult to do for many reasons; it is also known for its lowest success rate owing to poor bone quality, i.e., types III and IV bone. Sinus pneumatization also develops over a lengthy period of time in edentulous condition. This often causes absolute deficiency in bone volume. For the adequate restoration of the masticatory function under posterior occlusal load, the use of implants with sufficient length and diameter is required. Such anatomical concern serves as a major barrier to restoration. Lately, some cases have revealed the results of maxillary posterior restoration using short implants; since they do not have a long follow-up observation period, however, they have not yet to be proven. Still, sinus elevation is widely used to increase the vertical volume of bone followed by the placement of implants with sufficient length1,2.
The use of tapered-body implants can minimize marginal bone resorption by distributing the tension concentrating on the cortical bone. For the anterior region, it minimizes dehiscence or perforations at the talveolar ridge undercut during surgery. In particular, it benefits cases with nearby peripheral dental root since implants can be placed by avoiding the root. Furthermore, tapered-body implants are known for their strong initial stability3,4. Nedir et al.5 found that even for cases with 6 mm or less remaining bone in the maxilla, such implant offered a remarkable level of initial stability; after loading, marginal bone resorption was reduced.
The authors performed sinus bone graft using a lateral approach and conducted a retrospective study to assess the implant survival rate, success rate of tapered-body implants placed in patients, and resorption of peri-implant alveolar crest and sinus bone graft material.
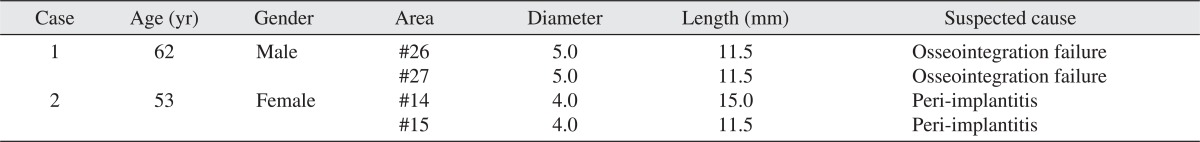
From September 2003 to January 2006, sinus bone graft was carried out via the lateral approach. The study subjects were 20 patients who had Osstem US III (Osstem Implant Co., Busan, Korea) implants placed. This study was conducted after obtaining approval from Seoul National University Bundang Hospital's Institutional Review Board (IRB Nno: B-1005-100-102). A total of 14 male patients and 6 females whose ages ranged from 38 to 72 years (average: 54.7 years) were included and satisfied as following inclusion criteria: patients were in good general health or controlled systemic disease with insufficient bone to need sinus bone graft. Sinus bone graft was done in the left and right regions of four patients, on the right for six patients, and on the left for ten patients. All in all, sinus bone graft was performed in 24 regions. The mean follow-up period was 19 months. Total 50 implants were placed and average implant length was 11.98±1.04 mm, implant diameter 4.58±0.49 mm. Most of implants were in male patients (n=38) and molar area (n=36).(Table 1)
Surgery was carried out under general, intravenous conscious sedation, or local anesthesia. Alveolar crest incision was followed by full-thickness flap elevation. A circular or an oval bony window was then removed from the lateral wall of the sinus. The removed bony window was wrapped in physiological saline-soaked gauze and stored for use as bone graft material. The sinus membrane was carefully elevated, followed by bone grafting. Particulated bone graft material was used in combination with Greenplast (Greencross, Seoul, Korea), a tissue adhesive, to prevent movement. Depending on the volume of the remaining alveolar bone, if initial stability for implants is possible, implants were placed simultaneously. Otherwise, delayed placement was performed only after several months' healing period.
Medical charts were retrospectively analyzed to examine the sinus bone graft method, use of graft material and membrane barrier for the lateral window, types of placed implants, complications, and healing period.
Based on the panoramic and periapical radiography taken right after operation, the one-year post-operative panoramic radiography and that taken at the final observation were compared for measurements of the resorption height of both sinus bone graft material and peri-implant alveolar crest bone. Periapical radiographs were taken using film holders with paralleling technique. For radiographic measurements, an IMPAX system (Agfa-Gevaert Group, Mortsel, Belgium) was used.
The pre-operative height of the remaining alveolar bone from the crest to the sinus floor was measured; afterward, based on the panoramic radiography taken right after operation, the length from the alveolar crest of each implant to the topmost part of the sinus bone graft was measured to evaluate the augmented volume. Based on the length of the placed implants, each expansion rate was considered and evaluated. The panoramic radiography taken one year after the bone graft was used to measure the resorption volume of the graft material.(Fig. 1)
Based on the radiography taken right after operation, the periapical radiography taken one year after the prosthetic function was compared in order to measure the bone resorption amount. The length of the placed implants was basically used to calculate the expansion rate of the periapical radiography for the evaluation of resorption volume. As for the resorption volume of the alveolar crest bone, the average of the resorption volume on the mesial and distal sides was calculated.
Cases with less than 1.5 mm of marginal bone resorption one year after prosthetic function - from among those showing no clinical symptoms such as mobility, pain, inflammation of marginal soft tissue, and radiolucency on the radiography at the point of the final observation - were considered successful.6 Regardless of the circumferential condition, the implants and superstructures that remained at the point of the final observation were considered survival cases. Those removed for some reason or with 1.5 mm or greater resorption of the peri-implant marginal bone were classified as failure.
A total of 15 patients had implants placed simultaneously with sinus bone graft, whereas 5 patients underwent delayed placement; all in all, 50 implants were placed. As for delayed grafting, implant placement was performed 4-7 months after bone grafting; in most cases, however, it was 4 months after. Every case was evaluated for the following: 1) augmented volume of grafted sinus bone; 2) resorption volume of sinus bone graft material one year after operation; and 3) marginal bone resorption, survival and success rates of implants one year after the implant prosthetic function developed.
A chi-squared test was used to compare the survival and success rates of the simultaneous and delayed graft groups; a Mann-Whitney U-test was used for the resorption volume of graft material and crestal bone. Analysis was carried out using SPSS software ver. 12.0 (SPSS Inc., Chicago, IL, USA), and the significance level was set to P<0.05.
Bone graft and implant placement were carried out in the premolar and molar regions.(Table 1)
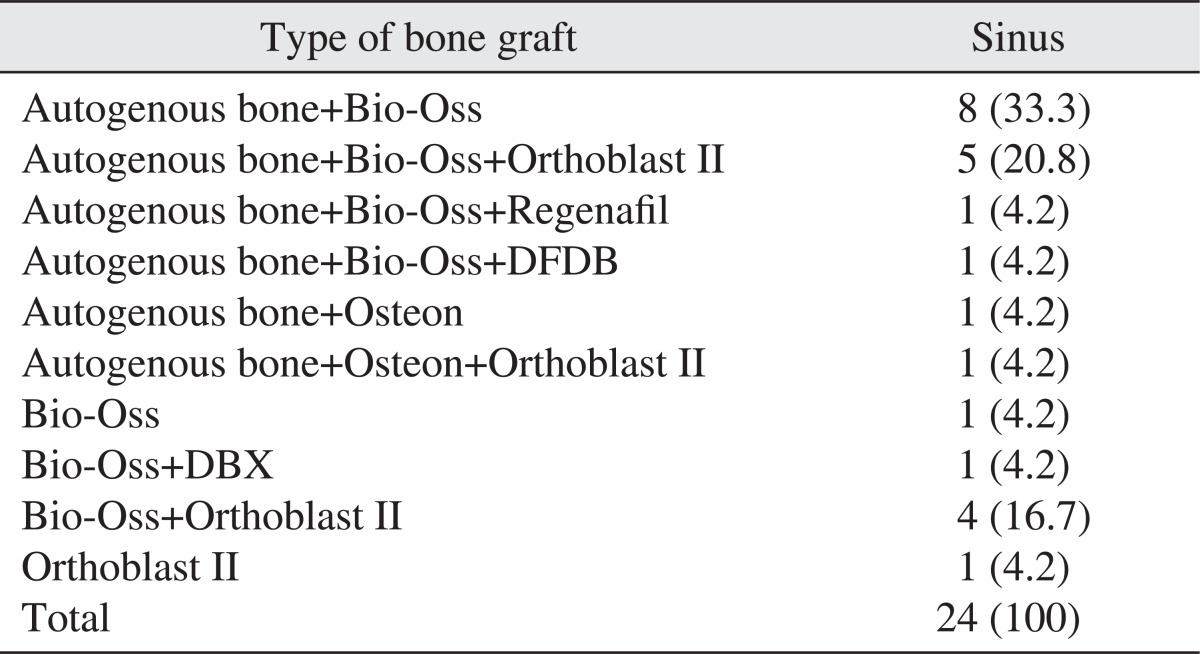
For sinus bone graft, bony windows were all formed on the anterior wall of the sinus. As graft materials, autogenous bone, allograft, xenograft, and alloplastic materials were used individually or in combination. The material used the most was autogenous+xenograft (33.3%), followed by autogenous+allograft+xenograft (29.2%) and allograft+xenograft (20.8%).(Table 2)
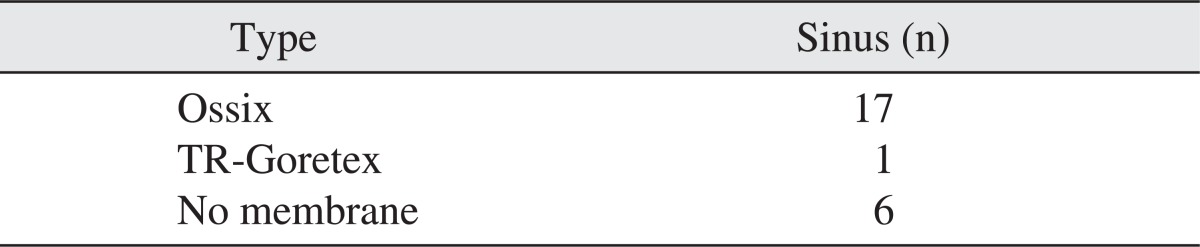
For the lateral bony window, bone graft was performed followed by the overlapping of the barrier membrane prior to suturing. Ossix (Implant Innovations, Palm Beach Gardens, FL, USA) was mostly used. Six regions had no use for barrier.(Table 3)
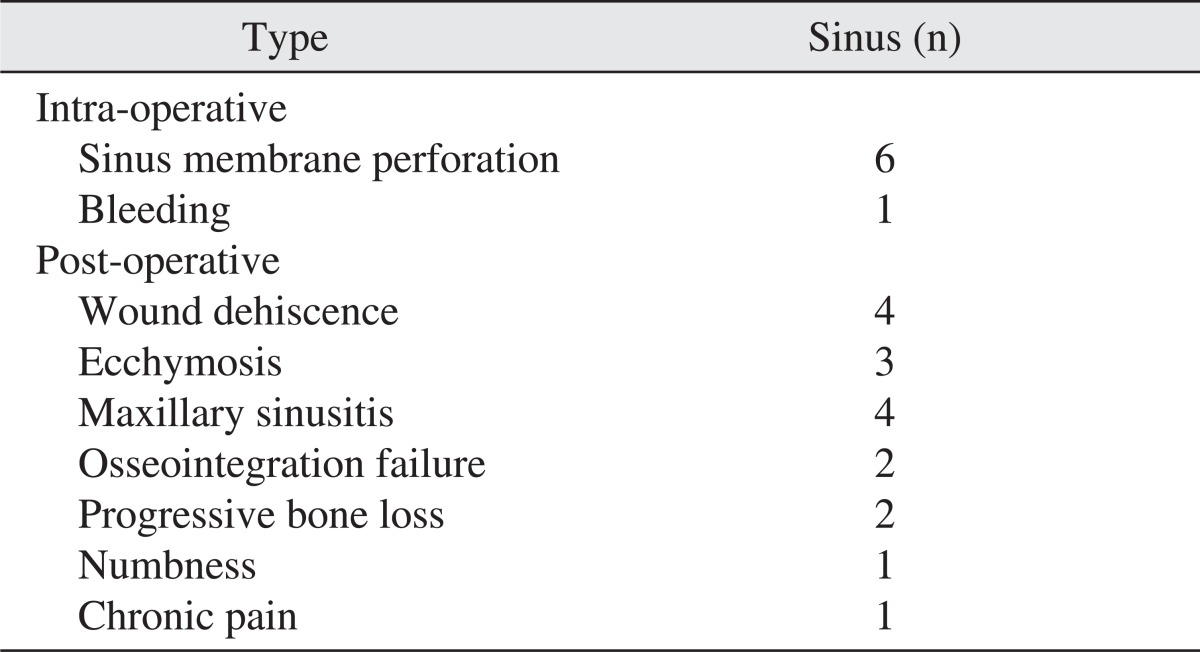
Complications during and after operation occurred variably. Some patients had a complex onset with more than two kinds. During sinus bone grafting, sinus mucosal perforations as the most frequent complication occurred in six cases. Bleeding - which is apparently a consequence of posterior superior alveolar artery damage - was observed in one case. Post-operative complications included four cases of wound dehiscence, four cases of sinusitis, three cases of ecchymosis, two cases of failed osseointegration, two cases of progressive bone loss, one case of neurologic damage, and one case of chronic pain in that order.(Table 4)
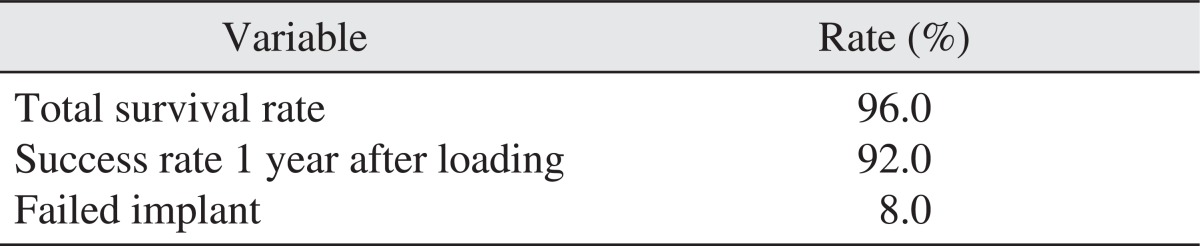
Two implants were removed due to poor initial stability; two other implants were considered a failure because marginal bone resorption due to peri-implantitis was more than 1.5 mm one year after the prosthetic function developed. For those removed due to failed osseointegration, replacement was performed. The replaced implants achieved successful osseointegration, so prosthetic restoration was carried out successfully. For two cases that developed more than 1.5 mm marginal bone resorption, implant removal was not performed. Instead, peri-implantitis was treated and maintenance care is being carried out.(Table 5) At least 4 out of a total of 50 implants were considered failures. Consequently, the success rate one year after prosthetic mounting was 92.0%, and the survival rate at the point of the final observation was 96.0%.(Table 6)
Mean preoperative residual bone height of the simultaneous group was 5.75±2.47 mm, delayed group 2.51±0.62 mm. There was statistically significant difference between two groups (P=0.000). The average augmented height of the total sinus bone graft was 12.35±3.27 mm. The one-year post-operative resorption was 0.97±0.84 mm, and marginal bone resorption was 0.17±0.27 mm.(Table 7) In this study, simultaneous implant placement was performed right after sinus bone graft (n=42) in most cases. Delayed placement was performed for a total of eight implants in five patients between four and seven months later. As for the augmented volume of bone graft, the simultaneous group was 11.85±3.29 mm, and the delayed group was 14.71±1.79 mm; thus showing statistically significant difference (P=0.012). On the other hand, no statistically significant difference in the resorption of graft material was observed between the two groups one year after operation (P=0.367). With regard to the one-year post-operative resorption volume of marginal bone, the simultaneous placement group recorded 0.12±0.23 mm, and the delayed group, 0.40±0.33 mm. The difference was statistically significant (P=0.046). The simultaneous group posted a 95.2% cumulative survival rate and a 90.5% success rate one year after functioning. The delayed group recorded 100% for both cases, with no statistically significant difference.(Table 8)
As a factor influencing the success of sinus bone graft implantation, the height of the remaining alveolar bone is crucial. Jensen and Greer7 found that less than 3 mm of remaining bone tissue showed very low success rate, but that the result was very good with 7-9 mm bone. In this study, the pre-operative height of the remaining bone was 5.19±2.58 mm, the success rate was 92.0%, and the survival rate was 96.0%; thus showing a relatively good result.
In this study, allograft was used in one site (4.2%), and xenograft, in one site, too (4.2%); the mixed material was used in 22 sites (91.6%). In most cases, sinus bone graft was performed using a combination of autogenous bone, xenograft, and allograft. In some studies, the analysis of the survival rates of implants in association with graft materials revealed the following results: 89% for autogenous bone, 93.4% for allograft, 95.5% for xenograft, 98.4% for alloplastic material, and 93.8% for mixed bone graft. Apart from bone graft materials, however, there are other factors affecting implant-bone integration and healing of sinus bone graft. For this reason, the excellence of only one specific material cannot be defined. In their comparative study of various bone material alternatives to be used for sinus bone graft, Scarano et al.8 found that those were all relatively stable without striking differences among the materials. Maiorana et al.9 reported a 97% cumulative survival rate in their study of sinus bone graft using alloplastic material and xenograft and implant placement. They also stated that these materials were not very absorptive, offering an adequate level of initial stability for implants; hence their usability for sinus bone graft. Since this retrospective study used a variety of materials, favoring a material-based prognosis is premature. This study had two implants failing in osseointegration in one sinus with immediate placement. Here, failure occurred only in cases involving the combined use of allograft and xenograft.
Tapered-body implants offer excellent initial stability and minimize the resorption of marginal bone. Thus, such kinds of products have been released in various brands. This study used Osstem US III fixtures with external hex connection based on two stage treatment. They feature double-tapered body, offering high initial stability for weak bone. They are also known for the excellence of tension distribution under masticatory load. They have a resorbable blast media (RBM) surface. A tapered-body implant is known particularly for its outstanding initial stability given the inferior quality of bone. García-Vives et al.4 found in their in vitro test using cow rib - which is similar to human type 4 bone - that tapered implants had greater initial stability than cylindrical ones. O'Sullivan et al.10 reported that with type 4 bone, the initial stability of tapered implants was most excellent. On the other hand, according to Alves and Neves11 the use of tapered implants was successful for type 4 bone of maxilla.
In the study by Nedir et al.5 the placement of tapered implants in the maxillary posterior regions had 100% cumulative survival rate one year after prosthetic mounting and a 94.4% success rate. In the study conducted by Astrand et al.12 for maxilla with types 3 and 4 bone, the cumulative survival rate of tapered implants was 96.9%. Bahat13 reported that tapered implants were placed via the two stage method in the maxilla where more than 10 mm implant placement was possible; after more than three years of observation, a 100% cumulative survival rate in the posterior region was achieved. Minichetti et al.14 recorded a 97.7% success rate in the use of tapered implants accompanied by allograft-based sinus graft.
With regard to covering the lateral window with a membrane barrier after sinus bone graft, a dispute arose; gradually, however, the use of the barrier is becoming more convincing in light of bone healing.15 Almost no difference is found between the use of non-absorptive and absorptive membrane barriers. The lateral window area heals last after sinus bone graft. Therefore, the use of membrane barrier limits soft-tissue invasion, significantly benefiting healing after sinus bone graft.16 In this study, resorbable collagen membrane was used for lateral walls for most cases; no membrane barrier was used in six sinus sites.
Some studies found that the use of tissue adhesive in particulated bone graft material prevented the mobility of particles; thus resulting in bone healing.17 When using the particle type of bone graft materials, the authors of this study generally use homologous tissue adhesive or platelet concentrate gel to stabilize the graft material. All the cases in this study also used the mixture with Greenplast tissue adhesive.
According to Kim's study18 on risky implant factors for sinus bone graft, sinus membrane perforation as the most frequently occurring complication occurred at 38 sites (35.5%), 7 of which (18.4%) had 9 failed implants in 6 patients. Post-operative complications included wound dehiscence (10 cases) followed by severe swelling, hematoma and subcutaneous bleeding (9), maxillary sinusitis (8), nasal bleeding (7), regional infection (3), and upper lip sensory anomaly (3). In particular, maxillary sinusitis developed in 7.5% of those patients with sinus bone graft, with one case of failed implantation recorded. At least 12 patients (13.6%) experienced early failure, which occurred within one year of prosthetic function after implant placement. A total of 17 implants (7.6%) failed. In this study, intra-operative complications included sinus mucosal perforations (6 sites) and bleeding (1). At least 6 different post-operative complications occurred at 14 sinus sites.(Table 4) Two patients had two implants with failed early osseointegration. Two implants failed due to peri-implantitis (8.0%). For those with failed osseointegration, the problem was resolved by removal and replacement. All cases were nonsubmerged implants. Those cases of failure were presumably due to early overload from temporary denture(s) mounted during the healing period after implant placement as well as poor initial stability and poor oral hygiene.(Table 5)
In the analysis of survival rate associated with the implant placement period, 61-100% survived for the simultaneous implantation, and 72.7-100%, for staged implantation. Due to various factors involved and rare cases of standardization, however, the difference by period was not distinctive. On the other hand, Wannfors et al.19 revealed that twice failure rate was observed from the simultaneous implantation group versus phase implantation among patients with sinus bone graft using iliac bone block. Herzberg et al.20 found no statistically significant difference between the simultaneous and delayed implantation groups after sinus bone graft and implantation for 70 patients: the cumulative survival rate for 4.5 years was 95.5%. Del Fabbro et al.21 confirmed through their review of 39 theses published between 1986 and 2002 that the implant survival rate was 91.49%, and that no significant difference was observed between the simultaneous and delayed groups considering their survival rates of 92.17% and 92.93%, respectively. Galindo-Moreno et al.22 performed sinus bone graft by combining autogenous cortical bone, cow bone, and platelet-rich plasma. A total of 263 implants were placed simultaneously or using the delayed method. Two years after prosthetic loading, two implants failed in early osseointegration, for a 99% implant success rate. Two years after the prosthetic mounting, all implants survived, showing no difference between the two implantation groups.
According to Herzberg et al.20, given residual bone height of 4 mm or less, marginal bone resorption was more likely. Rodoni et al.23 conducted a clinical, radiographic study on implants placed in 48 patients' maxillary posterior regions. They performed sinus bone graft and simultaneous and delayed implantations via a lateral approach for those patients whose residual bone was less than 6 mm high. For those with 6-8 mm high residual bone, they performed sinus floor elevation and simultaneous implantation using osteotome. For those patients with 8 mm or higher residual bone, conventional implantation was carried out (control group). For the average observation period of 4.6 years, with regard to marginal bone loss, the sinus bone graft group recorded 1.53 mm, the osteotome group, 2.40 mm, and the control group, 1.96 mm. No statistically significant difference was observed between each group. In the study of Hallman and Zetterqvist24, the mixture of bovine hydroxyapatite and autogenous bone was used for 20 patients. Grafting was done using tissue adhesive. Six months later, implant placement was performed. During 5 functioning years, 15 out of 108 implants were lost, for an 86% success rate. The average marginal bone loss was 1.3±1.1 mm. In this study, in the comparison between simultaneous and delayed implantations, the pre-operative condition showed a difference that was not statistically significant. For the simultaneous group, early osseointegration failure occurred in two cases; there was no failure in the delayed group. The success rate of implants placed one year after the prosthetic function developed was 90.5% for the simultaneous group and 100% for the delayed group, showing a stable result that is close to what was predicted. No statistically significant difference was found, however. With regard to marginal bone resorption, a statistically significant difference was found between the two groups. The delayed group exhibited a significant level of resorption and showed more than 1.5 mm marginal bone resorption in the case of two implants. One year after the start of prosthetic function, the success rate of implants was 92.0%; this was comparable to precedent studies.
Block et al.25 evaluated the height of sinus bone graft via complex motion tomography, which was done for 16 out of 31 patients with autogenous sinus bone graft. This study confirmed that new bone was generated in the sinus that had autogenous bone graft, and that it was retained well; 5-10 years later, the bone around and on top of the implant apex was still present. Out of the 70 implants examined, 90% (63/70) had the implant apex covered with bone. According to a five-year follow-up study following sinus bone graft conducted by Wiltfang et al.26 grafted bone resorption occurred consistently for 1-3 years; 3 years later, a relatively stable state was maintained. One year later, the three implants of two patients had the implant apex exposed to sinus; in these cases, intra-operative sinus perforation occurred. Therefore, intra-operative mucosal perforation presumably affects the loss or resorption of bone graft material. In this study, the 50 implants placed in 24 sinuses of 20 patients were studied, and the measurement of resorption of the sinus bone graft material was similar to the number of cases performed by Block et al.25 The average augmentation of sinus bone graft was 12.35 mm. One year after the bone graft, the resorption level was 0.97 mm on the average, 0.91±0.86 mm for the simultaneous implantation group, and 1.16±0.77 mm for the delayed group. The level was significant, but not statistically.
This retrospective study result has several limitations such as short observation period, use of various types of graft materials, and non-standardization of numerous factors. For the long-term stability evaluation of sinus bone graft materials and placed implants, more than three years' additional observation is required. Since the delayed implantation group did not secure a sufficient number of cases for this study, more cases would ensure better quality and significance.
The authors performed a clinical, radiographic evaluation of sinus bone grafting by considering 20 patients who had tapered implants placed via a lateral approach from September 2003 to January 2006. The following results were obtained:
1. Six different post-operative complications occurred at 14 sinus sites. As post-operative complications, intra-operative sinus mucosal perforation and wound dehiscence and maxillary sinusitis occurred with a high frequency.
2. Prior to operation, the average height of residual alveolar bone was 5.19 mm. Right after the operation, however, the height was 17.53 mm; one year later, it was 16.57 mm.
3. As for the failure of early osseointegration of implants, one patient had two failed implants, for an 8.0% early failure rate. One year after the prosthetic function developed, marginal bone resorption was 0.17 mm on the average. Two implants had 1.5 mm or greater marginal bone resorption. After one-year prosthetic functioning, the success rate of implants was 92.0%, and the cumulative survival rate was 96.0%. All implant with complete prosthesis survived until the point of the final observation. The survival rate for implant prostheses was 100%.
References
1. Chiapasco M, Zaniboni M, Rimondini L. Dental implants placed in grafted maxillary sinuses: a retrospective analysis of clinical outcome according to the initial clinical situation and a proposal of defect classification. Clin Oral Implants Res. 2008; 19:416–428. PMID: 18266875.

2. Lee EJ, Kim W, Choi JY, Kim SM, Oh NS. A systematic review of the survival rate on short implants. J Korean Acad Prosthodont. 2009; 47:457–462.

3. Achilli A, Tura F, Euwe E. Immediate/early function with tapered implants supporting maxillary and mandibular posterior fixed partial dentures: preliminary results of a prospective multicenter study. J Prosthet Dent. 2007; 97(6 Suppl):S52–S58. PMID: 17618934.

4. García-Vives N, Andrés-García R, Rios-Santos V, Fernández-Palacín A, Bullón-Fernández P, Herrero-Climent M, et al. In vitro evaluation of the type of implant bed preparation with osteotomes in bone type IV and its influence on the stability of two implant systems. Med Oral Patol Oral Cir Bucal. 2009; 14:e455–e460. PMID: 19718009.
5. Nedir R, Nurdin N, Szmukler-Moncler S, Bischof M. Placement of tapered implants using an osteotome sinus floor elevation technique without bone grafting: 1-year results. Int J Oral Maxillofac Implants. 2009; 24:727–733. PMID: 19885415.
6. Zarb GA, Albrektsson T. Towards optimized treatment outcomes for dental implants. J Prosthet Dent. 1998; 80:639–640. PMID: 9830065.
7. Jensen OT, Greer RO. Immediate placement of osseointegrated implants into the maxillary sinus augmented with mineralized cancellous allograft and Gore-Tex: second stage surgical and histological findings. In : Laney WR, Tolman DE, editors. Tissue integration in oral, orthopedic, and maxillofacial reconstruction. Chicago: Quintessence;1992.
8. Scarano A, Degidi M, Iezzi G, Pecora G, Piattelli M, Orsini G, et al. Maxillary sinus augmentation with different biomaterials: a comparative histologic and histomorphometric study in man. Implant Dent. 2006; 15:197–207. PMID: 16766904.

9. Maiorana C, Sigurtà D, Mirandola A, Garlini G, Santoro F. Sinus elevation with alloplasts or xenogenic materials and implants: an up-to-4-year clinical and radiologic follow-up. Int J Oral Maxillofac Implants. 2006; 21:426–432. PMID: 16796286.
10. O'Sullivan D, Sennerby L, Meredith N. Measurements comparing the initial stability of five designs of dental implants: a human cadaver study. Clin Implant Dent Relat Res. 2000; 2:85–92. PMID: 11359268.
11. Alves CC, Neves M. Tapered implants: from indications to advantages. Int J Periodontics Restorative Dent. 2009; 29:161–167. PMID: 19408478.
12. Astrand P, Billström C, Feldmann H, Fischer K, Henricsson V, Johansson B, et al. Tapered implants in jaws with soft bone quality: a clinical and radiographic 1-year study of the Brånemark System Mark IV fixture. Clin Implant Dent Relat Res. 2003; 5:213–218. PMID: 15127991.
13. Bahat O. Technique for placement of oxidized titanium implants in compromised maxillary bone: prospective study of 290 implants in 126 consecutive patients followed for a minimum of 3 years after loading. Int J Oral Maxillofac Implants. 2009; 24:325–334. PMID: 19492649.
14. Minichetti JC, D'Amore JC, Hong AY. Three-year analysis of tapered screw vent implants placed into maxillary sinuses grafted with mineralized bone allograft. J Oral Implantol. 2008; 34:135–141. PMID: 18616074.

15. Hockers T, Abensur D, Valentini P, Legrand R, Hammerle CH. The combined use of bioresorbable membranes and xenografts or autografts in the treatment of bone defects around implants. A study in beagle dogs. Clin Oral Implants Res. 1999; 10:487–498. PMID: 10740458.

16. Kim YK, Kim SG, Lee BG. Bone graft and implant. Seoul: Narae Pub Co.;2007. p. 169.
17. Graziani F, Ducci F, Tonelli M, El Askary AS, Monier M, Gabriele M. Maxillary sinus augmentation with platelet-rich plasma and fibrinogen cryoprecipitate: a tomographic pilot study. Implant Dent. 2005; 14:63–69. PMID: 15764947.

18. Kim YK. Implant risk factor of sinus bone graft (I): complication and early failure. J Korean Acad Oral Maxillofac Implantol. 2006; 10:42–55.
19. Wannfors K, Johansson B, Hallman M, Strandkvist T. A prospective randomized study of 1- and 2-stage sinus inlay bone grafts: 1-year follow-up. Int J Oral Maxillofac Implants. 2000; 15:625–632. PMID: 11055129.
20. Herzberg R, Dolev E, Schwartz-Arad D. Implant marginal bone loss in maxillary sinus grafts. Int J Oral Maxillofac Implants. 2006; 21:103–110. PMID: 16519188.
21. Del Fabbro M, Testori T, Francetti L, Weinstein R. Systematic review of survival rates for implants placed in the grafted maxillary sinus. Int J Periodontics Restorative Dent. 2004; 24:565–577. PMID: 15626319.

22. Galindo-Moreno P, Avila G, Fernández-Barbero JE, Aguilar M, Sánchez-Fernández E, Cutando A, et al. Evaluation of sinus floor elevation using a composite bone graft mixture. Clin Oral Implants Res. 2007; 18:376–382. PMID: 17355356.

23. Rodoni LR, Glauser R, Feloutzis A, Hämmerle CH. Implants in the posterior maxilla: a comparative clinical and radiologic study. Int J Oral Maxillofac Implants. 2005; 20:231–237. PMID: 15839116.
24. Hallman M, Zetterqvist L. A 5-year prospective follow-up study of implant-supported fixed prostheses in patients subjected to maxillary sinus floor augmentation with an 80:20 mixture of bovine hydroxyapatite and autogenous bone. Clin Implant Dent Relat Res. 2004; 6:82–89. PMID: 15669708.

25. Block MS, Kent JN, Kallukaran FU, Thunthy K, Weinberg R. Bone maintenance 5 to 10 years after sinus grafting. J Oral Maxillofac Surg. 1998; 56:706–714. PMID: 9632328.

26. Wiltfang J, Schultze-Mosgau S, Nkenke E, Thorwarth M, Neukam FW, Schlegel KA. Onlay augmentation versus sinuslift procedure in the treatment of the severely resorbed maxilla: a 5-year comparative longitudinal study. Int J Oral Maxillofac Surg. 2005; 34:885–889. PMID: 15978775.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download