Abstract
Alloplastic total replacement of the temporomandibular joint (TMJ) was developed in recent decades. In some conditions, previous studies suggested the rationale behind alloplastic TMJ replacement rather than reconstruction with autogenous grafts. Currently, three prosthetic products are available and approved by the US Food and Drug Administration. Among these products, customized prostheses are manufactured, via computer aided design/computer aided manufacturing (CAD/CAM) system for customized design; stock-type prostheses are provided in various sizes and shapes. In this report, two patients (a 50-year-old female who had undergone condylectomy for the treatment of osteochondroma extending to the cranial base on the left condyle, and a 21-year-old male diagnosed with left temporomandibular ankylosis) were treated using the alloplastic total replacement of TMJ using stock prosthesis. The follow-up results of a favorable one-year, short-term therapeutic outcome were obtained for the alloplastic total TMJ replacement using a stock-type prosthesis.
With stainless steel implant of glenoid fossa attempted for the correction of ankylosis in the 1960s, total temporomandibular joint (TMJ) replacement--which minimizes foreign body reaction and consists of highly biocompatible materials such as Cr-Co-Mo alloy, titanium, and ultra-high-molecular-weight polyethylene--began to be applied1-3. US Food and Drug Administration-approved products are now used worldwide, and their long-term follow-up data are constantly reported4,5. Nonetheless, concerns of early failure or long-term stability to TMJ prosthesis such as knee or hip joint remain after multiple complication from the installation of Proplast-Teflon (Vitek Inc., Houston, TX, USA) in TMJ in the United States in the 1980s6. Meanwhile, the use of stock prosthesis (Biomet Microfixation, Jacksonville, FL, USA) was approved in Korea in 2012. A report of two cases of total TMJ replacement using stock prosthesis for patients who had undergone treatment of osteochondroma and ankylosis of TMJ is presented below.
A 50-year-old female patient who had no specific medical history visited the hospital with facial asymmetry (chin deviation to the right side), limitation of mouth opening, and jaw pain that had persisted for two years. The clinical examination showed limitation of mouth opening (approximately 20 mm) along with TMJ pain on the left side and deviation of chin top to the right side. The radiography and computed tomography showed signs of considerable osseous proliferation extended to the cranial base and multiple radiopaque lesions suspected as phlebolith.(Fig. 1) The initial diagnosis was osteochondroma on the left condyle. She underwent condylectomy, and her chin top--which deviated to the right side--was also reduced to the midsagittal plane. Active physical therapy was conducted, and clinical favorable mouth opening (approximately 32 mm) was finally achieved in four months.(Fig. 2) Two years after surgery, however, she complained of limitation of mouth opening and discomfort of mastication. The X-ray revealed trauma from occlusion (TFO) in the maxillary molar area on the ipsilateral side as well as progressive osteoarthritis on the previous resection area. Total TMJ replacement using stock prosthesis on the ipsilateral joint was finally planned.
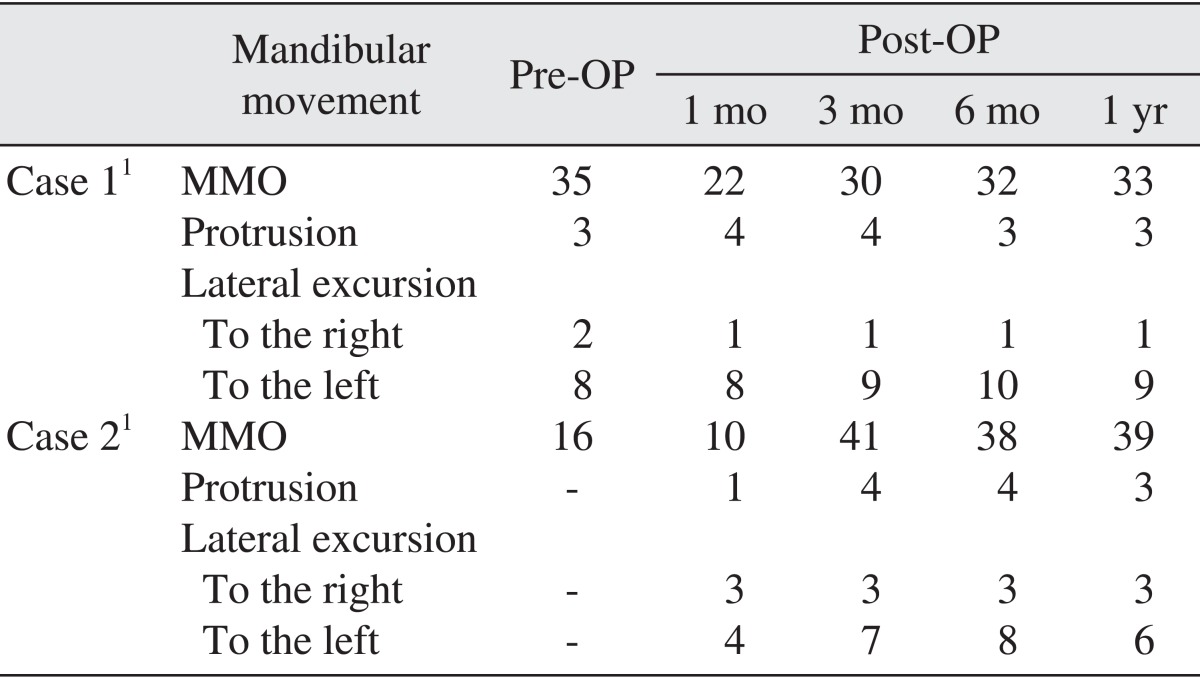
Stock TMJ prosthesis consists of fossa and condylar components, each of which requiring preauricular and retromandibular approaches. After condylectomy was performed to secure spaces for prosthesis via the preauricular approach, retromandibular incision was conducted. Bone trimming of uneven surface on articular eminence was followed by the installation of fossa component, and subsequent positioning of the condylar component was accomplished. After the optimal occlusion of the patient was maintained, fixation of the mandibular component was done with titanium screw7.(Fig. 3) Since the TMJ replacement, the patient had not suffered from remarkable postoperative complications including ipsilateral facial nerve weakness, paresthesia, pain, and dysfunction. She began light mouth opening exercise two weeks after the surgery and subsequently performed active exercise. Finally, she was able to maintain approximately 30 mm mouth opening, favorable mastication capability, and alleviation of TMJ pain since two months postoperative.(Table 1)
A 21-year-old male patient--who had undergone closed reduction for the fracture of bilateral mandibular condyle caused by a traffic accident five years ago--visited the hospital with limitation of mouth opening and pain on the left TMJ. He also had no specific medical history and showed limitation of mouth opening (approximately 16 mm) accompanying TMJ pain and crepitus on the left side along with troubled lateral excursion. The computed tomography image revealed signs of fibrous ankylosis and heterotopic bone formation on the postero-lateral surface of the left condyle head and temporal bone.(Figs. 4, 5) The plan of combined gap arthroplasty and total TMJ replacement was finally established.
Gap arthroplasty was performed, including condylectomy and excision of the 40×30×30 mm lesion of fibrous and bony ankylosis in the left TMJ.(Fig. 6. A) After normal range of jaw movement (approximately 30 mm) was secured, retromandibular incision was done. Bone trimming of articular eminence was consequently conducted, followed by the installation of prosthetic components7.(Fig. 6B-D) Postoperatively, the patient also began light mouth opening exercise followed by subsequent active exercise and achieved approximately 40 mm mouth opening in 2 months. He showed no loosening or missing of screws in the prosthetic component (Figs. 7, 8) and substantial alleviation of pain on the ipsilateral joint and maintained up to 40 mm mouth opening.(Fig. 9, Table 1)
Condylar reconstruction plates, condylar prostheses, costochondral graft, and distraction osteogenesis have been executed as reconstruction procedures for mandibular defects1. In marked contrast to autograft, the use of alloplastic material has neither morbidity of donor site nor requirement of prolonged maxillo-mandibular fixation and substantially reduces the time of operation and hospitalization. Other advantages are the high stability of occlusion, relatively higher predictability, and extensive reconstruction of joint defects. Indications of alloplastic total TMJ replacement include ankylosis of TMJ with severe anatomic alteration, failure of reconstruction with autogenous graft, severe inflammatory disease such as rheumatoid arthritis, and idiopathic condylar resorption8-11. In Case 2, the 21-year-old patient opted for alloplastic reconstruction considering the higher risk of re-ankylosis, morbidity of donor site and severe anatomic alteration of TMJ rather than combined gap arthroplasty and autogenous reconstruction.
For decades, literature has reported constant pain on TMJ or penetration of mandibular prosthesis into the cranial base in rare cases wherein only the condylar head is reconstructed with prosthesis. Thus, total joint replacement has been widely performed in the USA and Europe of late. Three of the major products are as follows: TMJ Implants (TMJ Implants Inc., Golden, CO, USA), TMJ Concepts (TMJ Concepts Inc., Ventura, CA, USA), and Biomet Microfixation. These products are categorized into stock type and customized type. TMJ Concepts is based on computer aided design/computer aided manufacturing (CAD/CAM) technology, and only the customized type is available, whereas TMJ Implants and Biomet Microfixation are both available in the customized type and stock type12. Stock prosthesis has obtained approval from the Ministry of Food and Drug Safety in Korea in July 2012.
Relatively more literature reviews are suggested with long-term follow-up surveys on customized prosthesis than stock prosthesis. Mercuri et al.4 reported statistically significant results with regard to the decrease in pain score as well as the improvement of mandibular function and diet consistency during an average of 11.4 years' follow-up survey conducted among 61 patients (41 bilateral replacements and 20 unilateral replacements) after replacement using customized prosthesis. In the case of extensive congenital bone defect, customized prosthesis is likely to be more desirable than stock prosthesis and is available with an efficient design for posterior stop after orthognathic surgery13. Meanwhile, some literatures suggested that the titanium backing of fossa component osseointegrated with the temporal bone may be unfavorable for re-operation14.
In terms of stock prosthesis, Leandro et al.5, who reported a 10 years' follow-up survey, suggested that there had been remarkable improvement on the jaw function, pronunciation, diet, and pain according to an average of 3.5 years' follow-up survey (minimum of 1 year, maximum of 10 years) among 300 patients (201 unilateral replacements and 99 bilateral replacements) who underwent total TMJ replacement using stock prosthesis. On the other hand, Westermark15 reported more than 34 mm mouth opening and improved masticatory activity and pain as a result of a 2 to 8 years' follow-up survey among 12 patients (5 unilateral replacements and 7 bilateral replacements) who underwent replacement using stock prosthesis10. Stock prosthesis minimizes the need for a complex process of three-dimensional model production and offers cheaper cost of operation than customized prosthesis. Nonetheless, concerns on the possibility of fine gap between host bone and prosthesis, removal of intact bone for fitting components, and perforation of surrounding anatomical structure remain due to the lack of support to prevent posterior displacement of the fossa component13.
Postoperative complication and short-term failure of alloplastic total TMJ replacement may be related to infection, loosening of screw or prosthesis, fracture of prosthesis, metal allergy, post-surgical neuroma, and re-ankylosis of surrounding bone. In the long-term aspects, the lifespan of TMJ prosthesis and large number of progress data have not been established to date. Integration of clinical follow-up data was also achieved only in the last two decades12. Nevertheless, alloplastic total TMJ replacement is considered a reliable procedure in terms of safety and durability of material, based on several results of recent studies, e.g., absence of giant cell reaction found in Proplast-Teflon implant, advance verification of the same material in existing literatures on orthopedic joint replacement, and favorable results of follow-up survey in previous literature4-6,11,15,16.
In these cases, the patients underwent unilateral TMJ replacement; no surgical modality was conducted on contralateral TMJ. In a similar case report, Guarda-Nardini et al.17 introduced post-surgical protocol including the combination of passive and active exercises combined with the injection of hyaluronate on the contralateral non-operated TMJ. Meanwhile, contralateral excursion and preservation of ipsilateral excursion had a limitation due to the detachment of the lateral pterygoid muscle during surgery.(Table 1) According to Voiner et al.18, unilateral TMJ replacement showed a wider range of mandibular motion than bilateral TMJ replacement, and the difference was statistically significant. Looking into the treatment progress in Case 1 closely, at postoperative 1-year period, the outcome of TMJ replacement was favorable with regard to pain, jaw function, and quality of life, but the range of postoperative mouth opening was not sufficiently improved in contrast to the preoperative value. Such tendency is attributed to the lack of efforts to maintain periodic active mouth opening exercise; the chronic condition of masticatory muscle and contralateral TMJ contributed to TMJ dysfunction.
The report of these two cases is in accordance with the abovementioned indications suggested by literature, confirming its suitability and short-term stability in terms of improvement of the jaw function, pain, diet, and, ultimately, quality of life. Although there are some mechanical and morphological limitations compared to the customized TMJ prosthetic system, stock TMJ prosthetic systems provide cost- and time-effective means of joint reconstruction, and successful outcomes can be expected with skilled operative techniques and proper case selections.
References
1. Driemel O, Braun S, Müller-Richter UD, Behr M, Reichert TE, Kunkel M, et al. Historical development of alloplastic temporomandibular joint replacement after 1945 and state of the art. Int J Oral Maxillofac Surg. 2009; 38:909–920. PMID: 19464145.

2. Westermark A, Leiggener C, Aagaard E, Lindskog S. Histological findings in soft tissues around temporomandibular joint prostheses after up to eight years of function. Int J Oral Maxillofac Surg. 2011; 40:18–25. PMID: 21044827.

3. Mercuri LG. Alloplastic temporomandibular joint reconstruction. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998; 85:631–637. PMID: 9638694.

4. Mercuri LG, Edibam NR, Giobbie-Hurder A. Fourteen-year follow-up of a patient-fitted total temporomandibular joint reconstruction system. J Oral Maxillofac Surg. 2007; 65:1140–1148. PMID: 17517298.

5. Leandro LF, Ono HY, Loureiro CC, Marinho K, Guevara HA. A ten-year experience and follow-up of three hundred patients fitted with the Biomet/Lorenz Microfixation TMJ replacement system. Int J Oral Maxillofac Surg. 2013; 42:1007–1013. PMID: 23769150.

6. Huh JK. Alloplastic total temporomandibular joint replacement. J Korean Dent Assoc. 2012; 50:256–261.
7. Granquist EJ, Quinn PD. Total reconstruction of the temporomandibular joint with a stock prosthesis. Atlas Oral Maxillofac Surg Clin North Am. 2011; 19:221–232. PMID: 21878254.

8. Mercuri LG. Total joint reconstruction--autologous or alloplastic. Oral Maxillofac Surg Clin North Am. 2006; 18:399–410. PMID: 18088840.

9. Mercuri LG. A rationale for total alloplastic temporomandibular joint reconstruction in the management of idiopathic/progressive condylar resorption. J Oral Maxillofac Surg. 2007; 65:1600–1609. PMID: 17656290.

10. Chung CJ, Choi YJ, Kim IS, Huh JK, Kim HG, Kim KH. Total alloplastic temporomandibular joint reconstruction combined with orthodontic treatment in a patient with idiopathic condylar resorption. Am J Orthod Dentofacial Orthop. 2011; 140:404–417. PMID: 21889086.

11. Mercuri LG. The use of alloplastic prostheses for temporomandibular joint reconstruction. J Oral Maxillofac Surg. 2000; 58:70–75. PMID: 10632168.

12. Guarda-Nardini L, Manfredini D, Ferronato G. Temporomandibular joint total replacement prosthesis: current knowledge and considerations for the future. Int J Oral Maxillofac Surg. 2008; 37:103–110. PMID: 18022347.

13. Mercuri LG. Alloplastic temporomandibular joint replacement: rationale for the use of custom devices. Int J Oral Maxillofac Surg. 2012; 41:1033–1040. PMID: 22771166.

14. Jones RH. Temporomandibular joint reconstruction with total alloplastic joint replacement. Aust Dent J. 2011; 56:85–91. PMID: 21332746.

15. Westermark A. Total reconstruction of the temporomandibular joint. Up to 8 years of follow-up of patients treated with Biomet(®) total joint prostheses. Int J Oral Maxillofac Surg. 2010; 39:951–955. PMID: 20594807.

16. Granquist EJ, Chou JC, Giannakopoulos H, Livolsi VA, Quinn PD. Post-surgical neuromas in patients with total alloplastic temporomandibular joint reconstruction: a retrospective case series. Int J Oral Maxillofac Surg. 2011; 40:366–371. PMID: 21123031.

17. Guarda-Nardini L, Manfredini D, Ferronato G. Total temporomandibular joint replacement: a clinical case with a proposal for post-surgical rehabilitation. J Craniomaxillofac Surg. 2008; 36:403–409. PMID: 18657432.

18. Voiner J, Yu J, Deitrich P, Chafin C, Giannakopoulos H. Analysis of mandibular motion following unilateral and bilateral alloplastic TMJ reconstruction. Int J Oral Maxillofac Surg. 2011; 40:569–571. PMID: 21376536.

Fig. 1
Pre-condylectomy radiography and computed tomography (Case 1). Radiopaque mass extendingantero-superiorly from left condyle. A. Panoramic view. Well-demarcated lesion extended to the cranial base, on left condyle (arrowheads). B. Cross-sectional view. C. Coronal view. D. Sagittal view.
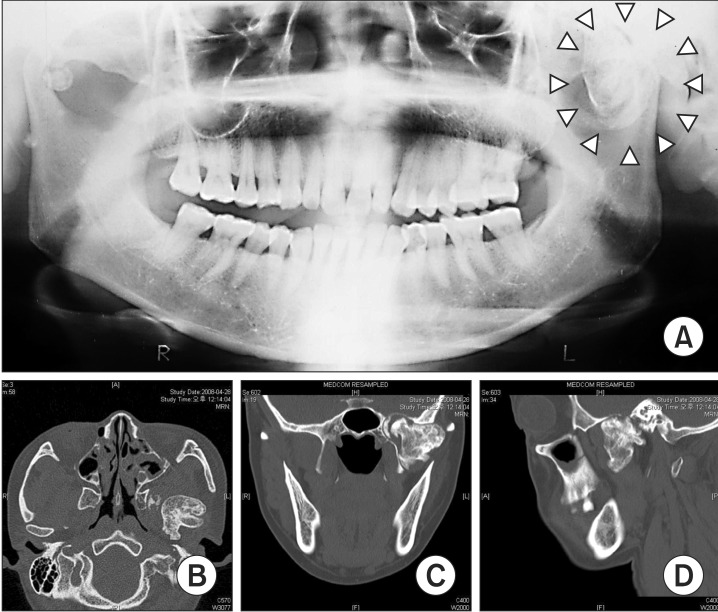
Fig. 2
Preoperative radiography (Case 1) show previous condylectomy area on left temporomandibular joint (TMJ) (arrow). A. Panoramic view. B. Postero-anterior cephalogram. C. TMJ tomogram. D. Lateral cephalogram.
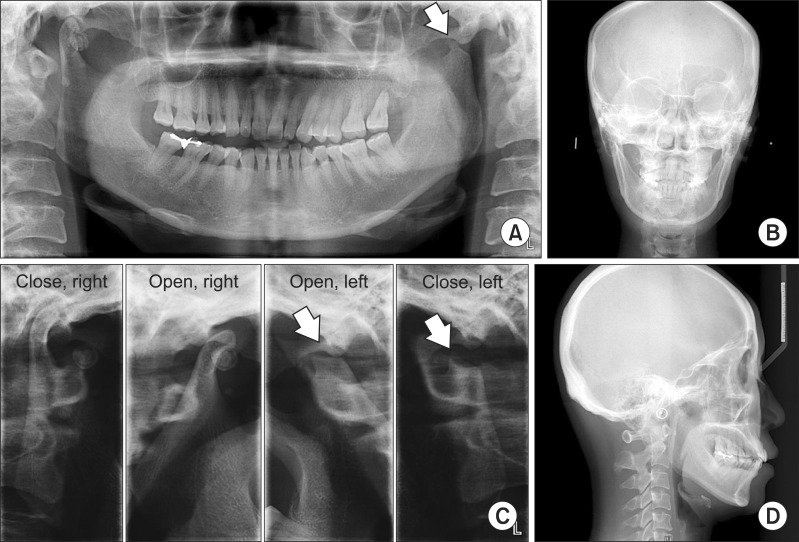
Fig. 3
Postoperative 1-year radiography (Case 1). A. Panoramic view. B. Postero-anterior cephalogram. C. Temporomandibular joint tomogram. D. Lateral cephalogram.
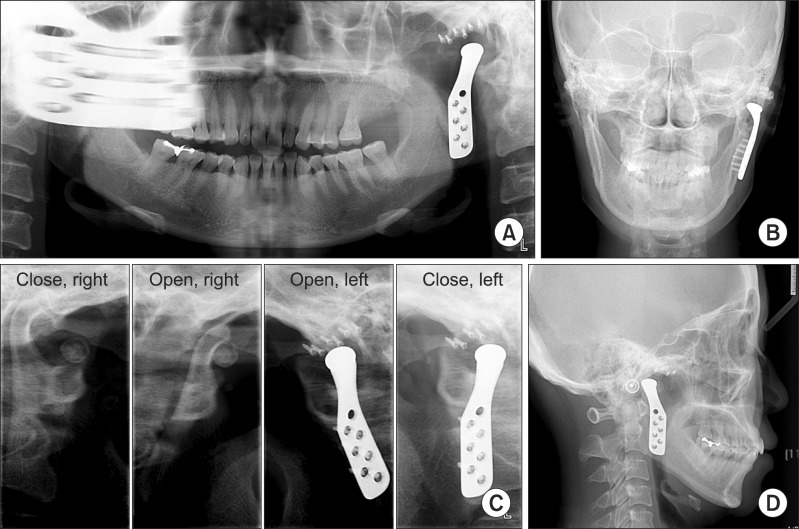
Fig. 4
Preoperative radiography (Case 2). The lesion of fibrous and bony ankylosis was suspected on left temporomandibular joint (TMJ) (arrowheads). A. Panoramic view. B. Postero-anterior cephalogram. C. Llimitation of translation of left condyle on TMJ tomogram. D. Lateral cephalogram.
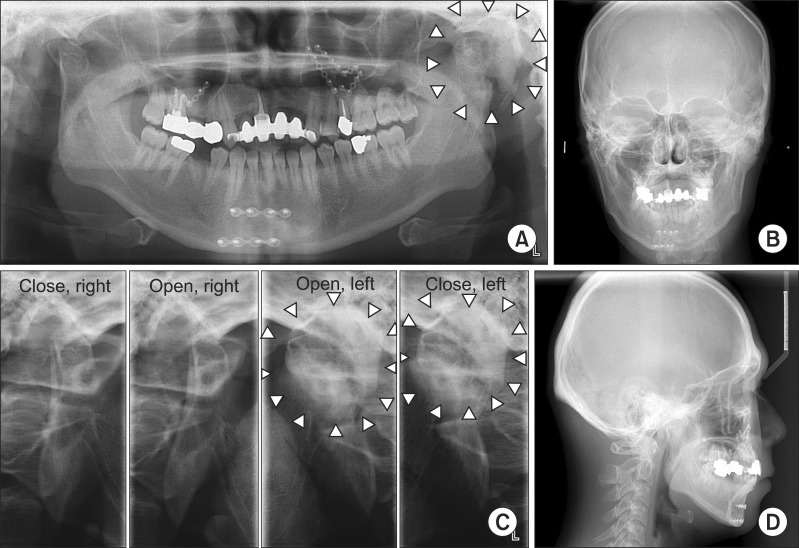
Fig. 5
Preoperative computed tomography (Case 2). A. Cross sectional view. B. Coronal view. C. Sagittal view.
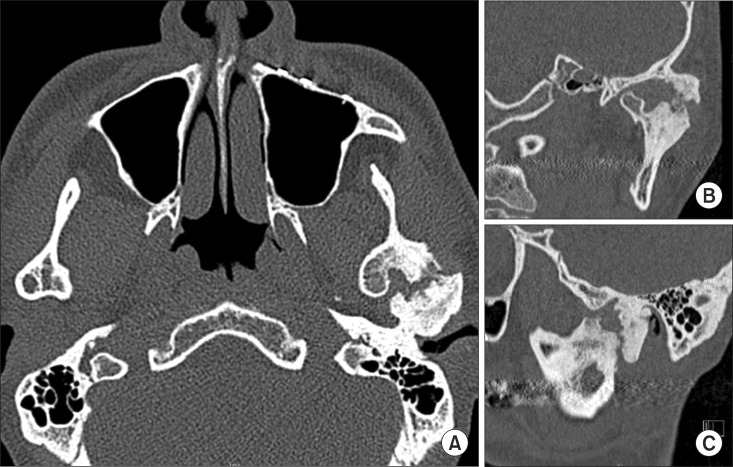
Fig. 6
Intraoperative photographs (Case 2). A. Removal of lesion of fibrous and bony ankylosis on left temporomandibular joint. B. Adaptation of fossa component. C. Adaptation of condyle component. D. Confirmation of range of motionwith the maximal mouth opening above 30 mm.
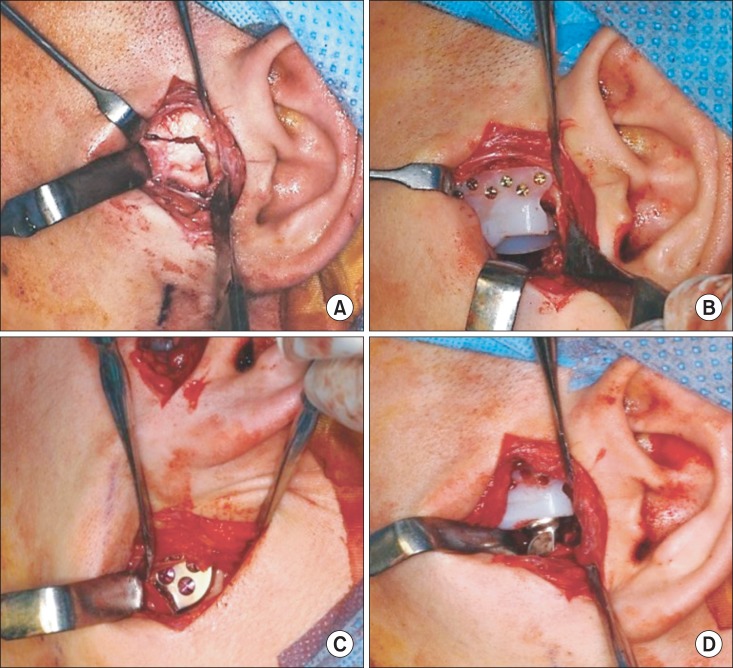
Fig. 7
Computed tomogram of 5 days after surgery. Axial (A), coronal (B), sagittal (C) view and 3 dimensional reconstruction images (D, E) comparing preoperative and postoperative 5 days.
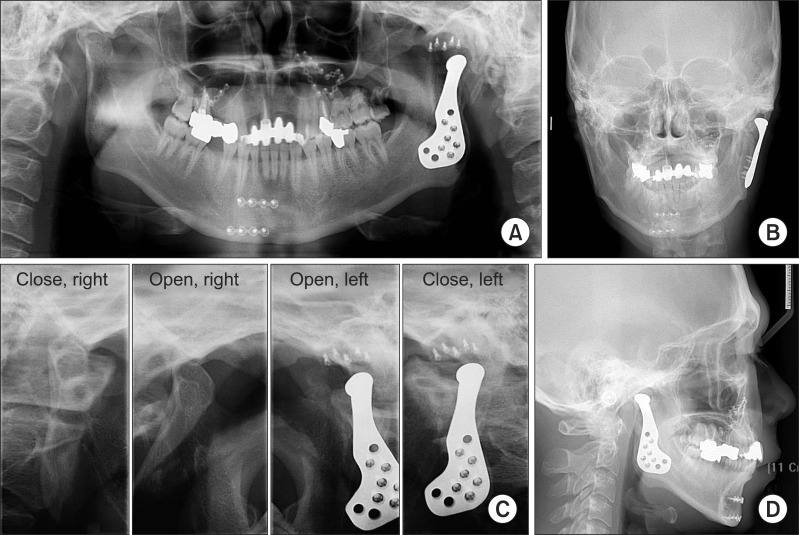
Fig. 8
Postoperative 1-year radiography (Case 2). A. Panoramic view. B. Postero-anterior cephalogram. C. Temporomandibular joint tomogram. D. Lateral cephalogram.
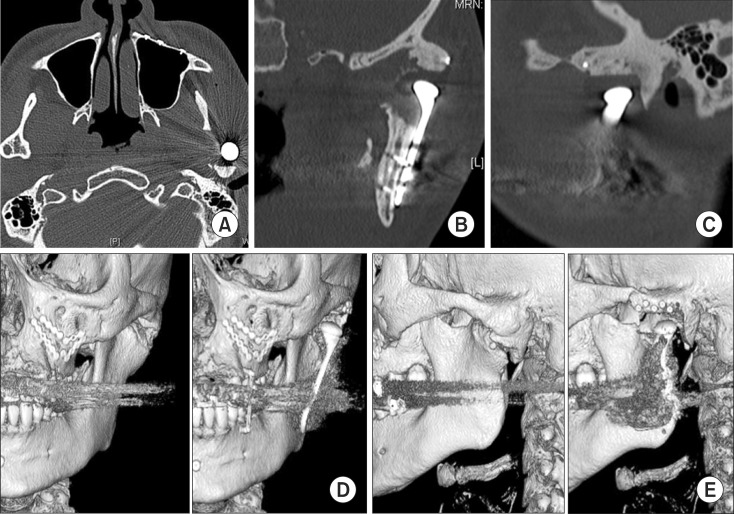
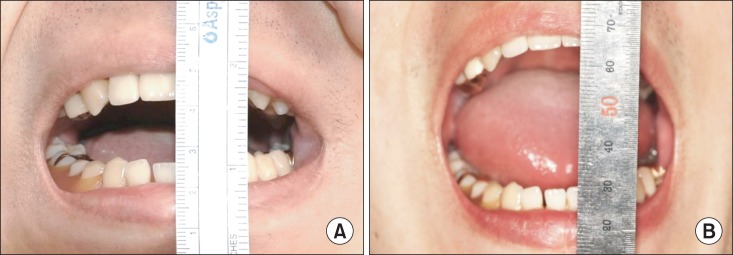
Fig. 9
Preoperative and postoperative (6 months) maximal mouth opening (MMO) (Case 2). A. Preoperative MMO was 16 mm. B. At postoperative 6 months MMO have increased to 38 mm.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download