Abstract
Objectives
The interforminal region, between the mandibular foramen, is known as a relatively safe area that is free of anatomic structures, such as inferior alveolar nerve, submandibular fossa, and lingual side of the mandible is occasionally neglected for its low clinical importance. Even in the case of a severely constricted alveolus, perforation of the lingual cortical bone had been intended. However, anterior extension of the inferior alveolar canal, important anatomic structure, such as concavity of lingual bone, lingual foramina, and lingual canal, has recently been reported through various studies, and untypical bleeding by perforation of the lingual plate on implantation has also been reported. Therefore, in this study, we performed radiographic and statistical analysis on distribution and appearance frequencies of the lingual foramina that causes perforation of the mandibular lingual cortical bone to prevent complications, such as untypical bleeding, during surgical procedure.
Materials and Methods
We measured the horizontal length from a midline of the mandible to the lingual foramina, as well as the horizontal length from the alveolar crest to the lingual foramina and from the lingual foramina to the mandibular border by multi-detector computed tomography of 187 patients, who visited Dankook University Dental Hospital for various reasons from January 1, 2008 to August 31, 2012.
Results
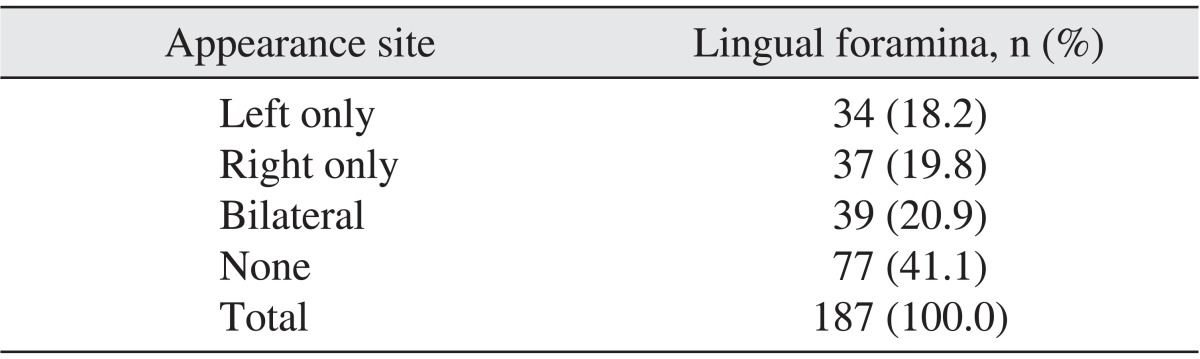
From a total of 187 human mandibles, 110 (58.8%) mandibles had lingual foramina; 39 (20.9%) had bilateral lingual foramen; 34 (18.2%) had the only left lingual foramen; and 37 (19.8%) had the only right lingual foramen.
Conclusion
When there is consistent bleeding during a surgical procedure, clinicians must consider damages on the branches of the sublingual artery, which penetrate the lingual foramina. Also, when there is a lingual foramina larger than 1 mm in diameter on a pre-implantation computed tomography, clinicians must beware of vessel damage. In order to prevent these complications and progress with a safe surgical procedure, a thorough radiographic examination before the surgery is indispensable. Further, clinicians should retract lingual flap definitely to confirm the shape of the lingual bone and existence of the lingual foramina.
The success of mandibular bone operations, such as implant placements, can depend on the radiological exam, which helps determine the parameters of implant placement by revealing the structure of the mandible, alveolar bone shape, and volume. Panoramic and tomographic radiograms are used to carry out these analyses. However, the radiogram appears only in two dimensions, and the extent of magnification (10% to 30%) depends on the patient anatomy as parts of the mandible can obscure key elements in the image. Recently, cone-beam computed tomography (CBCT) has begun to be widely used prior to implant surgeries. Multi-planar slices of CBCT, which has fixed magnification, is clinically useful in determining implant parameters and preventing damage to vulnerable structures, such as the inferior alveolar neural tubes and maxillary antrum1,2. Since CBCT has a lower resolution than multi-detector computed tomography (MDCT), it has limitations in examining soft tissues, soft tissue lesions, and blood vessels compared to MDCT3.
The most common complications of implant surgery in the mandible are paresthesia and hemorrhage caused by damage to inferior alveolar nerves. Since the alveolar and basal bone areas between the mandibular mental foramina are relatively safe areas, the lingual aspect of the mandible has been viewed as less clinically significant. Even in cases of alveolar bone atrophy, penetration of lingual cortical bone is recommended for denture implants4. Recent studies, however, have demonstrated the existence of structures that could in fact cause complications: the anterior dilation of inferior alveolar neural tubes, concavity of lingual bones, lingual foramina, and lingual tubes. Moreover, many cases of atypical hemorrhage have been caused by lingual plate perforation5-8.
The sublingual and submental arteries run under the lingual aspect of the mandible, sending branches to the mylohyoid muscle, peripheral muscles, mucous membrane, and gingiva. These mucosal branches settle along the lingual aspect of the mandible and may require special care prior to surgery since they are known to deposit lingual cortical bone into the mandible9-15. This study performed radiological and statistical analyses on the appearance frequency and distribution of lingual foramina in mandibular cortical bone in Koreans, with the aim of preventing clinical complications during surgical procedures.
We examined 187 patients who had undergone CT scans at Dankook University Dental Hospital (Cheonan, Korea) between January 1, 2008 and August 31, 2012. Mandibles with intraosseous lesions or fractures in the target area were excluded.
Three observers measured the locations of the lingual foramina three times a week, using discriminable images of the axial, sagittal, and coronal views from MDCT (WCT-345-130, Somatom Emotion 6; Siemens AG, Munich, Germany). Of 187 patients, 121 were male and 66 were female. The average age (±standard deviation [SD]) was 33.13±15.40 years.
The sagittal and axial CT images were used for measurements. In the sagittal view, three horizontal base lines and one vertical base line were established. The first horizontal base line (line A) was tangent to the mandibular margin in the buccolingual direction; the vertical base line (line V) was perpendicular to line A. The second horizontal line (line B) was perpendicular to line V, passing through the lingual foramina. The third horizontal line (line C) was tangential to the top of the alveolar bone crest, perpendicular to line V. According to these standards, vertical distance 1 (VD1) and vertical distance 2 (VD2) were measured in order, as shown in Fig. 1.
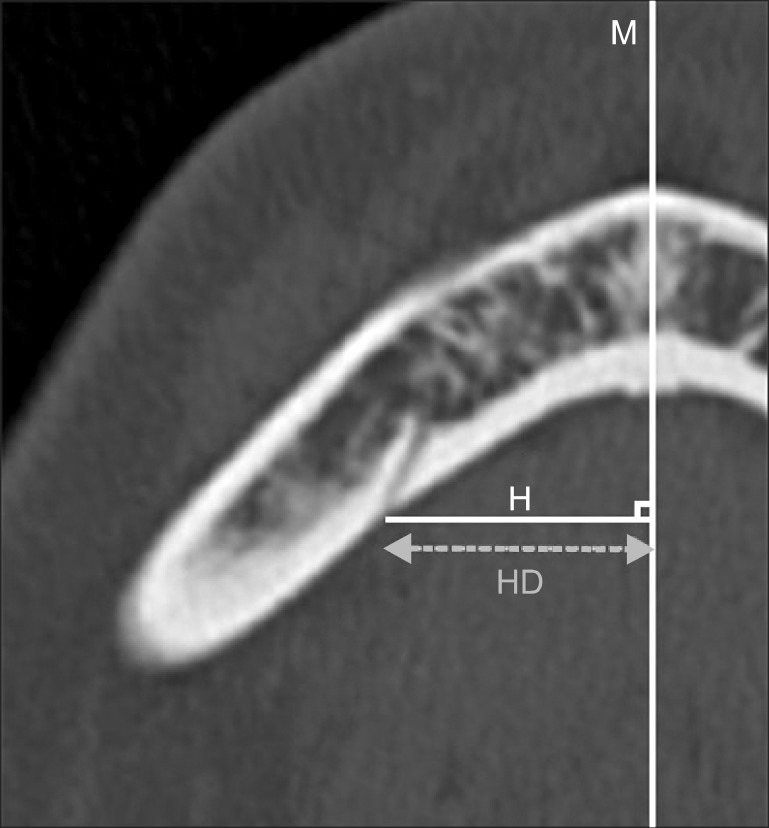
Next, one horizontal base line (line M) and one vertical base line (line H) were set. Line M was a straight line that precisely divided the mandible into two in the axial view. Line H was perpendicular to line M, passing through the fenestra of the lingual foramina. The horizontal distance (HD) was measured using images acquired based on these standards, as shown in Fig. 2.
Lingual foramina existed in 110 (58.8%) of 187 mandibles; the remaining 77 cases (41.1%) had no lingual foramina. With regard to distribution of the foramina, 39 (20.9%) cases were bilateral, 34 (18.2%) were left-sided, and 37 (19.8%) were right-sided.(Table 1)
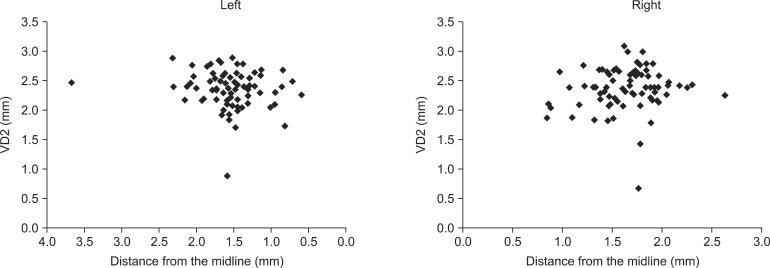
HD refers to the distance from the lingual foramina to the central base line that divides the mandible into two sections. For the left-sided foramina, the mean HD value (±SD) was 1.57±0.41 mm, the minimum value was 0.84 mm, and the maximum value was 3.68 mm. For right-sided foramina, the mean HD value (±SD) was 1.61±0.33 mm, the minimum value was 0.84 mm, and the maximum value was 2.62 mm.
VD1, the vertical distance from the lingual foramina to the top of the alveolar bone crest, had a mean value (±SD) of 2.40±0.31 mm, minimum value of 0.90 mm, and the maximum value of 2.90 mm on the left side and a mean value (±SD) of 2.40±0.34 mm, minimum value of 0.70 mm, and maximum value of 3.10 mm on the right side.
VD2, the distance from the lingual foramina to the inferior margin of the mandible, had a mean value (±SD) of 0.68±0.25 mm, minimum value of 0.34 mm, and maximum value of 2.29 mm on the left side and a mean value (±SD) of 0.68±0.28 mm, minimum value of 0.31 mm, and maximum value of 2.61 mm on the right side.
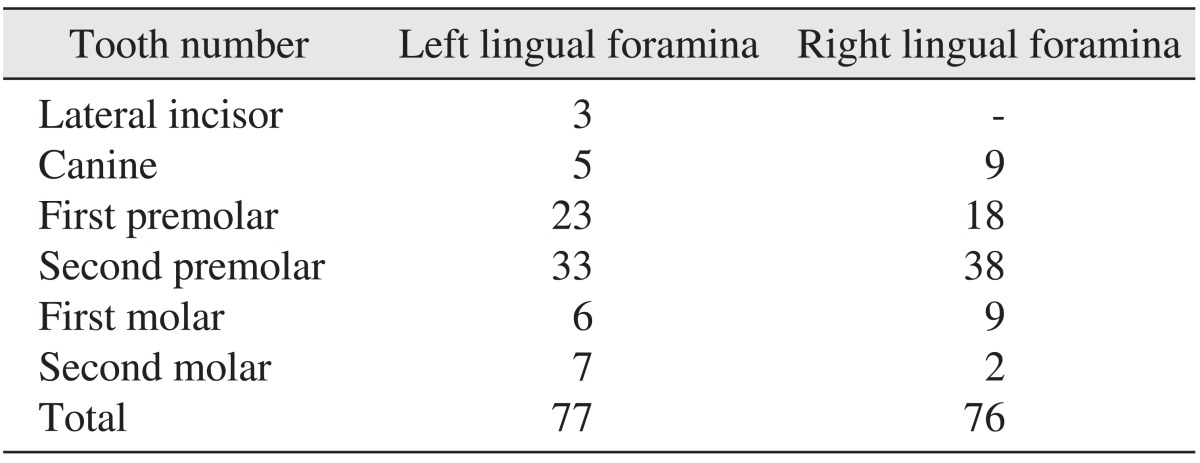
Since lingual foramina can be located relative to tooth numbers, teeth are important reference points in implant surgery. A tooth number was recorded when the baseline of VD1 met the alveolar ridge line. The second mandibular premolar was the most frequently recorded tooth on both sides, followed by the first mandibular premolar. No lingual foramina were noted in association with the lower lateral incisor on the right side.(Table 2)
Small foramina are often observed on the anterior surface of the mandible and near the premolars of the lingual mandible. Tagaya et al.16 named these median lingual foramina and lateral lingual foramina, respectively17.
In a study by McDonnell et al.9, 311 (99%) of 321 mandibles had median lingual foramina. According to Tepper et al.10, who examined 70 subjects via CT scan, either median lingual foramina or lateral lingual foramina existed between mental foramens in the lingual mandible.
The anatomical research on 194 Korean mandibles by Kim et al.18 divided the foramina vertically into incisor, premolar, and molar regions, as well as three horizontal regions. The appearance frequency of lateral lingual foramina on the medial surface of the mandible was reported to be highest in the lowest 1/3 region of tooth and premolar tooth. Moreover, foramina appeared more frequently on the right side (32.9%) than the left side (27.8%). The average count of lateral lingual foramina was three, with appearance frequencies correlating with tooth stage: 2.01 for mixed dentition, 3.03 for permanent dentition, and 3.15 for mandibles with lost permanent teeth18.
Loukas et al.19 reported that the lateral lingual foramina were located an average of 10.3 mm (5.6 to 18.9 mm) above the basal area of the mandible, and that the average diameter was 0.8 mm (0.6 to 1.0 mm). Liang et al.20 found 31 (62%) lateral lingual foramina in 56 dried human mandibles, 15 of which were bilateral, eight were present only on the left side, and eight that were present only on the right side. Of a total of 56 units, at least 35 cases of lateral lingual foramina were found on the right side and 21 on the left side. In 14 cases, lateral lingual formation was observed on the upper or middle third of the mandible.
Since the first study of its kind by Krenkel and Holzner21 in 1986, there have been numerous case reports of severe hemorrhage during surgical procedures on the area between the lingual mandible and mental foramen (dental extraction, removal of lingual torus, biopsy, mandibulectomy, and denture implantation)21-27. According to these studies, most complications are caused by perforations to the lingual cortical bone during implant placement in the canine region28; this region contains the sublingual branches of the lingual and facial arteries, which anastomose before entering the lingual foramina, forming branches of the inferior alveolar artery8.
According to these cases, immediate bleeding and severe edema during implant surgery are due mostly to direct damage of the sublingual arteries, as a consequence of lingual cortical bone perforation. In cases of delayed bleeding, the possibility of damage by perforating sublingual artery branches must be considered. Moreover, bleeding risk must be assessed if the patient has hypertension or hemostatic disorder or takes anticoagulant drugs. Pre-surgical risk should also be assessed if the diameter of the foramen is greater than 1 mm on CT scan. Elderly patients who need alveoloplasty for denture procedures and patients who have severe alveolar bone atrophy are at increased risk, as their lingual foramina are close to the alveolar ridge; the appearance frequency of lingual foramina in these patients is also high.
Edema must be recognized as a key indicator of surgical bleeding. Damage to the perforating artery as it passes through the lingual foramen can cause edema, in which case, pressure should be applied to the lingual face of the mandible, and antihemorrhagics emergently adminstered29. When the bleeding ceases, antibiotics and steroids should be considered30.
Mandibular lingual foramina are difficult to identify on a panoramic X-ray because the cervical vertebrae overlap with the beam's trajectory31. However, high-resolution CT is able to visualize the complex neurovasculature of the inter-foraminal space without distortion. CT scans are thus indispensable to pre-surgical evaluation, particularly for procedures such as dental implants, mandibular augmentation, and genioplasty. Pre-surgical scans should be used to evaluate volume, width, and shape of the mandible, as well as other anatomical structures.
This study aimed to investigate atypical hemorrhage and edema resulting from implant placement between the mental foramen, an area known to be 'safe' due to its lack of anatomically vulnerable structures. Our research on the lingual foramina, which are yet unclassified structures, investigated 187 patients presenting to Dankook University Dental Hospital via MDCT. We drew the following conclusions:
1. Lingual foramina existed in 110 (58.8%) of 187 mandibles. With regard to the distribution of the foramina, 39 (20.9%) cases were bilateral, 34 (18.2%) were left-sided, and 37 (19.8%) were right-sided.
2. The location of the lingual foramina varied from the lower lateral incisor to the second molar tooth, appearing most frequently in the second premolar tooth. Fig. 3 shows the vertical distance of the lingual foramina according to the distance from the center line.
3. VD2, the distance from the lingual foramina to the inferior margin of the mandible, had a mean value (±SD) of 0.68±0.25 mm, a minimum value of 0.34 mm, and a maximum value of 2.29 mm on the left side and a mean value (±SD) of 0.68±0.28 mm, a minimum value of 0.31 mm, and a maximum value of 2.61 mm on the right side.
References
1. Abrahams JJ, Hayt MW. Dental CT in pathologic changes of the maxillo-mandibular region. Radiologe. 1999; 39:1035–1043. PMID: 10643027.
2. Dula K, Buser D, Porcellini B, Berthold H, Schwarz M. Computed tomography/oral implantology (I). Dental CT: a program for the computed tomographic imaging of the jaws: the principles and exposure technic. Schweiz Monatsschr Zahnmed. 1994; 104:450–459. PMID: 8209215.
3. Angelopoulos C, Scarfe WC, Farman AG. A comparison of maxillofacial CBCT and medical CT. Atlas Oral Maxillofac Surg Clin North Am. 2012; 20:1–17. PMID: 22365427.

4. Laboda G. Life-threatening hemorrhage after placement of an endosseous implant: report of case. J Am Dent Assoc. 1990; 121:599–600. PMID: 2229738.

5. Mason ME, Triplett RG, Alfonso WF. Life-threatening hemorrhage from placement of a dental implant. J Oral Maxillofac Surg. 1990; 48:201–204. PMID: 2299461.

6. Mordenfeld A, Andersson L, Bergström B. Hemorrhage in the floor of the mouth during implant placement in the edentulous mandible: a case report. Int J Oral Maxillofac Implants. 1997; 12:558–561. PMID: 9274086.
7. Kattan B, Snyder HS. Lingual artery hematoma resulting in upper airway obstruction. J Emerg Med. 1991; 9:421–424. PMID: 1787287.
8. Kalpidis CD, Setayesh RM. Hemorrhaging associated with endosseous implant placement in the anterior mandible: a review of the literature. J Periodontol. 2004; 75:631–645. PMID: 15212344.

9. McDonnell D, Reza Nouri M, Todd ME. The mandibular lingual foramen: a consistent arterial foramen in the middle of the mandible. J Anat. 1994; 184:363–369. PMID: 8014127.
10. Tepper G, Hofschneider UB, Gahleitner A, Ulm C. Computed tomographic diagnosis and localization of bone canals in the mandibular interforaminal region for prevention of bleeding complications during implant surgery. Int J Oral Maxillofac Implants. 2001; 16:68–72. PMID: 11280364.
11. Gahleitner A, Hofschneider U, Tepper G, Pretterklieber M, Schick S, Zauza K, et al. Lingual vascular canals of the mandible: evaluation with dental CT. Radiology. 2001; 220:186–189. PMID: 11425994.

12. Yoshida S, Kawai T, Okutsu K, Yosue T, Takamori H, Sunohara M, et al. The appearance of foramen in the internal aspect of the mental region of mandible from Japanese cadavers and dry skulls under macroscopic observation and three-dimensional CT images. Okajimas Folia Anat Jpn. 2005; 82:83–87. PMID: 16350420.

13. Kawai T, Sato I, Yosue T, Takamori H, Sunohara M. Anastomosis between the inferior alveolar artery branches and submental artery in human mandible. Surg Radiol Anat. 2006; 28:308–310. PMID: 16547603.

14. Lustig JP, London D, Dor BL, Yanko R. Ultrasound identification and quantitative measurement of blood supply to the anterior part of the mandible. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003; 96:625–629. PMID: 14600700.

15. Liang X, Jacobs R, Lambrichts I, Vandewalle G, van Oostveldt D, Schepers E, et al. Microanatomical and histological assessment of the content of superior genial spinal foramen and its bony canal. Dentomaxillofac Radiol. 2005; 34:362–368. PMID: 16227480.

16. Tagaya A, Matsuda Y, Nakajima K, Seki K, Okano T. Assessment of the blood supply to the lingual surface of the mandible for reduction of bleeding during implant surgery. Clin Oral Implants Res. 2009; 20:351–355. PMID: 19298289.

17. Shiller WR, Wiswell OB. Lingual foramina of the mandible. Anat Rec. 1954; 119:387–390. PMID: 13197797.

18. Kim HJ, Choi BY, Lee HY, Chung IH. Morphological study of the mental spine, lingual foramen and nutrient foramen and innominate foramen in Korean mandibles. Korean J Phys Anthropol. 1993; 6:129–140.

19. Loukas M, Kinsella CR Jr, Kapos T, Tubbs RS, Ramachandra S. Anatomical variation in arterial supply of the mandible with special regard to implant placement. Int J Oral Maxillofac Surg. 2008; 37:367–371. PMID: 18262766.

20. Liang X, Jacobs R, Lambrichts I, Vandewalle G. Lingual foramina on the mandibular midline revisited: a macroanatomical study. Clin Anat. 2007; 20:246–251. PMID: 16683247.

21. Krenkel C, Holzner K. Lingual bone perforation as causal factor in a threatening hemorrhage of the mouth floor due to a single tooth implant in the canine region. Quintessenz. 1986; 37:1003–1008. PMID: 3489246.
22. Isaacson TJ. Sublingual hematoma formation during immediate placement of mandibular endosseous implants. J Am Dent Assoc. 2004; 135:168–172. PMID: 15005432.

23. Budihardja AS, Pytlik C, Haarmann S, Holzle F. Hemorrhage in the floor of the mouth after second-stage surgery: case report. Implant Dent. 2006; 15:148–152. PMID: 16766897.

24. Niamtu J 3rd. Near-fatal airway obstruction after routine implant placement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001; 92:597–600. PMID: 11740473.

25. Ferneini E, Gady J, Lieblich SE. Floor of mouth hematoma after posterior mandibular implants placement: a casereport. J Oral Maxillofac Surg. 2009; 67:1552–1554. PMID: 19531435.
26. Givol N, Chaushu G, Halamish-Shani T, Taicher S. Emergency tracheostomy following life-threatening hemorrhage in the floor of the mouth during immediate implant placement in the mandibular canine region. J Periodontol. 2000; 71:1893–1895. PMID: 11156047.

27. Mardinger O, Manor Y, Mijiritsky E, Hirshberg A. Lingual perimandibular vessels associated with life-threatening bleeding: an anatomic study. Int J Oral Maxillofac Implants. 2007; 22:127–131. PMID: 17340906.
28. Kalpidis CD, Konstantinidis AB. Critical hemorrhage in the floor of the mouth during implant placement in the first mandibular premolar position: a case report. Implant Dent. 2005; 14:117–124. PMID: 15968182.

29. Woo BM, Al-Bustani S, Ueeck BA. Floor of mouth haemorrhage and life-threatening airway obstruction during immediate implant placement inthe anterior mandible. Int J Oral Maxillofac Surg. 2006; 35:961–964. PMID: 16829038.
30. Goldstein BH. Acute dissecting hematoma: a complication of oral and maxillofacial surgery. J Oral Surg. 1981; 39:40–43. PMID: 6969794.
31. Dreiseidler T, Mischkowski RA, Neugebauer J, Ritter L, Zöller JE. Comparison of cone-beam imaging with orthopantomography and computerized tomography for assessment in presurgical implant dentistry. Int J Oral Maxillofac Implants. 2009; 24:216–225. PMID: 19492636.
Fig. 1
Reference lines used in measurement on the coronal views of multi detector computed tomography. (C: third horizontal reference line, V: vertical reference line, B: second horizontal reference line, A: first horizontal reference line, VD1: vertical distance 1, VD2: vertical distance 2)
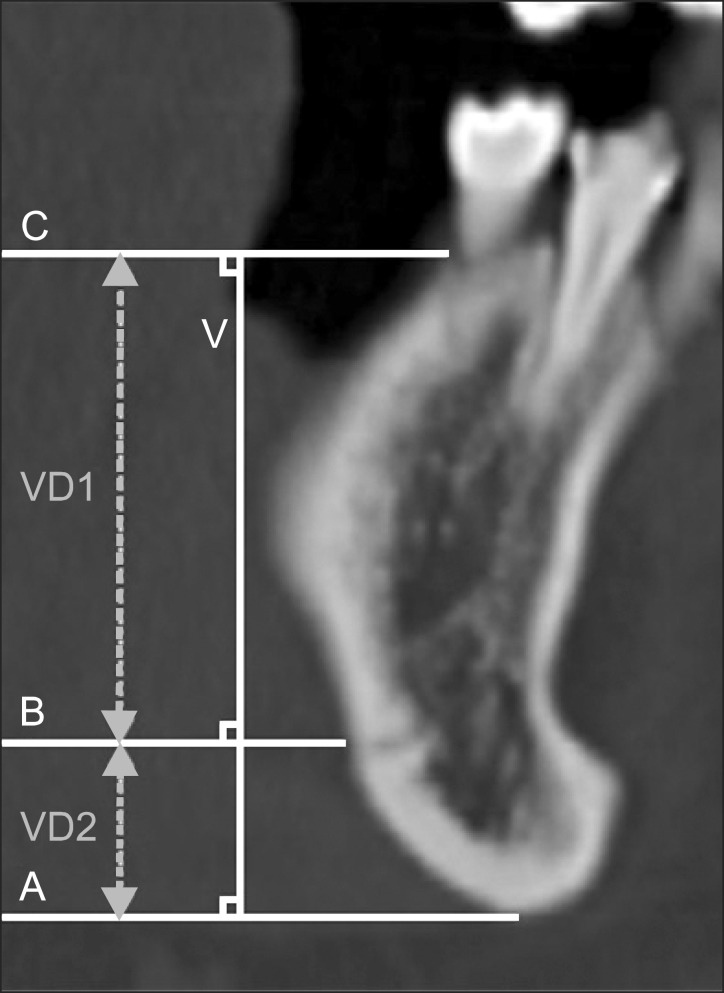
Fig. 2
Reference lines used in measurement on the axial views of multi detector computed tomography. (M: midline of mandible, H: vertical base line, HD: horizontal distance from midline to lingual foramina)




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download