Abstract
Objectives
Oral and maxillofacial defects often require bone grafts to restore missing tissues. Well-recognized donor sites include the anterior and posterior iliac crest, rib, and intercalvarial diploic bone. The proximal tibia has also been explored as an alternative donor site. The use of the tibia for bone graft has many benefits, such as procedural ease, adequate volume of cancellous and cortical bone, and minimal complications. Although patients rarely complain of pain, swelling, discomfort, or dysfunction, such as gait disturbance, both patients and surgeons should pay close attention to such after effects due to the possibility of tibial fracture. The purpose of this study is to analyze tibial fractures that occurring after osteotomy for a medioproximal tibial graft.
Materials and Methods
An analysis was intended for patients who underwent medioproximal tibial graft between March 2004 and December 2011 in Inha University Hospital. A total of 105 subjects, 30 females and 75 males, ranged in age from 17 to 78 years. We investigated the age, weight, circumstance, and graft timing in relation to tibial fracture.
Autogenous, allogenous, or heterogenous bone can be used for contouring bony-defect sites in the oromaxillofacial area. Autogenous bone is typically the best selection because of its osteogenic, osteoconductive, and osteoinductive properties1-3. Typical donor sites include jaw, ileum, tibia, cranium, and rib. Tibia can also be used as a bone graft due to its low complication rate, simple technique, and sufficient cancellous bone including cortical bone compared to any other site except the jaw.
Catone et al.4 stated that pain control was easy, and esthetic problems, neurological impairment, infection, hematoma, and fracture did not typically occur after tibial bone graft. Even in cases of elderly patients, similar results were reported. However, as a tibial fracture can be evoked by intensive exercise or external force, they concluded that care must be taken to avoid fracture until three months after surgery.
The subjects of this study were patients who underwent proximal-medial-tibial bone graft under general anesthesia between March 2004 and December 2011, at the Department of Oral and Maxillofacial Surgery in Inha University Hospital (Incheon, Korea), and the operations were performed by two surgeons.
Surgical procedures in all cases was performed as follows5,6: (1) the location of the tibial tuberosity was palpated and identified on the anterior surface of the proximal end of the tibia, (2) a 1.0 cm or 1.5 cm horizontal line following skin creases was drawn just below the tibial tuberosity, (3) local anesthesia was infiltrated subcutaneously at the level of the periosteum, (4) a horizontal incision was made with a #15 blade, and reflection of the periosteum was performed with a periosteal elevator in order to expose the tibial bone, (5) a circular bony window 1.0 cm in diameter was made with a fissure bur and osteotome, and (6) with a bone curette, cancellous bone was harvested as needed.
Patient age ranged from 17 to 78 years (mean, 43.2 years). A total of 105 subjects (30 females, 75 males), underwent surgery. The reason for operation was cystic lesion in 92 cases, benign tumor in 12 cases, and oral-maxillary sinus fistula in one case. We investigated the age, weight, circumstance, and graft timing in relation to tibial fracture in all patients.
Between March 2004 and December 2011, tibial fracture occurred in four of 105 tibial bone grafts. They took place between February and May 2010. There were no significant differences in graft region, shape, or scale between fractured and non-fractured patients on X-ray imaging before and after grafting.
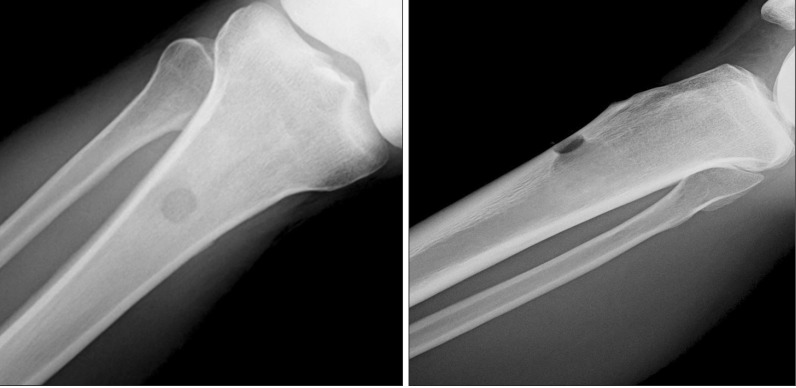
Patient 1 was a 46-year-old, 68.2 kg male. He underwent right tibial graft surgery due to an oroantral fistula.(Fig. 1) Fracture occurred when he jumped from a truck 20 days after surgery.(Fig. 2) Noninvasive reduction and fixation were performed for 56 days (Figs. 3, 4), and the fracture was completely healed after six months.(Fig. 5)
Patient 2 was a 63-year-old, 56.6 kg female. She underwent right tibial graft surgery due to a mandibular radicular cyst. Fracture occurred when she jumped to exit a bus 12 days after surgery.(Fig. 6) Noninvasive reduction and fixation were performed for 80 days (Figs. 7, 8), and the fracture was completely healed after six months.(Fig. 9)
Patient 4 was a 35-year-old, 68.7 kg male who underwent right tibial graft surgery due to an odontogenic keratocyst of an anterior mandibular tooth and the premolar region. Fracture occurred when he bumped into a vending machine 18 days after surgery. Open reduction and fixation were performed at another hospital, and he fully recovered. X-ray images could not be obtained.
The ileum was initially recognized as the ideal region for cancellous bone collection and, until lately, has remained the favored donor site for auto-cancellous bone. Numerous studies have reported ileum graft surgery and its complications. In 1991, O'Keeffe et al.7 collected proximal-tibial cancellous bone and used it as graft preparation. They reported that tibial bone had easy accessibility for operation, appropriate qualitative and quantitative properties, and a rare complication rate, leading to its useful application.
One of the possible complications of a tibial graft is that it can damage the articular surface and change the growth pattern for non-mature patients8,9. Additionally, a study by Besly and Ward Booth10 comparing tibial and iliac grafts reported that complications such as pain, swelling, and gait disturbance might be present, in addition to the scarring at the operation site that is often considered acceptable by patients after tibia graft. One study5 about tibial grafts reported complications including swelling, gait disturbance for 3-4 weeks, and dehiscence of suture site. Likewise, Lezacano et al.11 explained that articular surface damage, tendon or nerve damage, and rare tibial fracture as potential complications.
A comparison study10 with tibial and iliac grafts reported tibia graft advantages of low blood loss and fast gait recovery. In that study, all patients with tibial graft were able to walk within one day. Moreover, a study by Marchena et al.12 showed that, for outpatient procedures, complications such as infection, swelling, and fracture did not occur.
On the other hand, O'Keeffe et el.7 reported that tibial fracture occurred in one of 230 proximal tibial bone graft harvestings and suggested that patients should avoid external pressure on the region for at least six weeks after surgery. In two case series by van Damme and Merkx8,9, two of nine patients experienced fracture at one week after the tibial bone graft surgery, while playing tennis in one patient and while running in the other. Both patients were treated with noninvasive reduction for tibial fracture. These authors insisted that patients should avoid exercise for at least 4-6 weeks after tibial bone graft surgery. Hughes and Revington13 reported that fracture occurred in two of 75 patients due to exercising at three months and falling at nine days after surgery. Both patients were treated with immobilization using plaster of Paris splints for tibial fractures. Thor et al.14 reported that tibial fracture occurred for one patient who had 5 mL of compressed cancellous bone harvested for implantation after falling on the stairs at two weeks after surgery. They considered the fall a major factor in the fracture, but the design of the cortical bone window, the bone-harvesting technique, and immediate weight-bearing were suspected to be additional contributing factors.
The conventional surgical procedure for medio-proximal tibial graft is performed through a vertical or oblique incision at the medial portion of the tibial tuberosity2,8,9,11. In contrast, we created a horizontal incision in the wrinkle line just below the tibial tuberosity in order to reduce scar formation5,6. Accordingly, the bony window was located 1.0 cm lower than in the conventional procedure. However, no articles related to the frequency and risk of tibial fracture in accordance with the location of bony window were found in the studied literature.
Alt et al.15 conducted a study to evaluate the relation between volume of harvested cancellous bone and fracture risk during tibial bone graft. They collected cancellous bone from one cadaver tibia and did not collect from the other tibia. They made a 1-1.5 cm diameter bony window 1.5 cm inferior to the tibial tubercle and collected most of cancellous bone from each sites, which was then measured using a 10 mL syringe. Subsequently, they pressed on the major axis of tibia in order to create a fracture. In five of eight cadavers, higher power was necessary to create fractures in the intact tibias, while the three other cadavers showed decancellated tibias that were more resistant to force than the intact tibias. Furthermore, the magnitude of force for fracture showed no statistically significant difference between the two groups. As a result, they concluded that collecting the cancellous bone does not increase the risk of tibial fracture.
Another study by Vittayakittipong et al.16 showed that the mean maximal compressive strength was 9,087.50 N in a group of decancellated tibias and 9,491.13 N in a group of intact tibias. There was no significant difference between the two groups, although greater collection of bone tended to cause a decrease in bone resistance. Accordingly, they recommended abstaining from exercise for 2-3 months after the surgery. A similar cadaver study by Gerressen et al.17 showed that tibias from which cancellous bone was not collected were able to resist a greater amount of pressure in the major axis (mean, 5,126.4 N) than the group from which bone was collected (mean, 3,766.9 N). This difference was considered to be meaningful to patients. In this regard, Morrison18 suggested that pressure exerted on the tibia during walking reached 2-4 times the force of one's weight regardless of sex. Nisell19 described that isokinetic knee extension exerted 5-9 times the force of one's weight on the tibia. Gerressen et al.17 concluded that fractures could occur at lower pressures after tibial graft regardless of sex or age, and that tibial graft might greatly increase the possibility of tibial fracture. Consequently, they recommended limiting activities to those involving a pressure equal to only half the body weight during the first week after surgery and resuming normal activities five weeks following surgery.
In the present study, all patients were instructed to walk carefully starting the day after operation. Additionally, we instructed patients not to perform exercise for at least three months after surgery and to be cautious about the risk of fracture due to external force. Only four of 105 tibial graft patients experienced tibial fracture, and all fractures occurred between two and seven weeks after surgery. Since tibial fractures occurred only during this certain period, we conclude that patient education is a very important factor to prevent tibial fractures. In addition, all fractures were caused by external trauma. Indirect vertical force caused by jumping in Cases 1 and 2 and direct lateral force caused by bumping into objects in Cases 3 and 4 were the causes of fracture in this study. From these results, we can assume that tibial fractures are vulnerable to direct or indirect external trauma rather than due to physical condition, such as body weight or age.
References
1. Lee CY. An in-office technique for harvesting tibial bone: outcomes in 8 patients. J Oral Implantol. 2003; 29:181–184. PMID: 12964798.
2. Jakse N, Seibert FJ, Lorenzoni M, Eskici A, Pertl C. A modified technique of harvesting tibial cancellous bone and its use for sinus grafting. Clin Oral Implants Res. 2001; 12:488–494. PMID: 11564109.

3. Herford AS, King BJ, Audia F, Becktor J. Medial approach for tibial bone graft: anatomic study and clinical technique. J Oral Maxillofac Surg. 2003; 61:358–363. PMID: 12618977.

4. Catone GA, Reimer BL, McNeir D, Ray R. Tibial autogenous cancellous bone as an alternative donor site in maxillofacial surgery: a preliminary report. J Oral Maxillofac Surg. 1992; 50:1258–1263. PMID: 1333008.

5. Hernández-Alfaro F, Martí C, Biosca MJ, Gimeno J. Minimally invasive tibial bone harvesting under intravenous sedation. J Oral Maxillofac Surg. 2005; 63:464–470. PMID: 15789317.

6. Baek MK, Kim IK, Cho HY, Chang KS, Park SH, Park JW, et al. A retrospective analysis of the medioproximal tibial bone graft for oral and maxillofacial reconstruction. J Korean Assoc Maxillofac Plast Reconstr Surg. 2008; 30:241–248.
7. O'Keeffe RM Jr, Riemer BL, Butterfield SL. Harvesting of autogenous cancellous bone graft from the proximal tibial metaphysis. A review of 230 cases. J Orthop Trauma. 1991; 5:469–474. PMID: 1762010.
8. van Damme PA, Merkx MA. A modification of the tibial bone-graft-harvesting technique. Int J Oral Maxillofac Surg. 1996; 25:346–348. PMID: 8961013.

9. van Damme PA, Merkx MA. Fracture of the tibia after the modified tibial bone-graft-harvesting technique: a report of two cases. J Craniomaxillofac Surg. 1998; 26(Suppl 1):197. PMID: 9777498.
10. Besly W, Ward Booth P. Technique for harvesting tibial cancellous bone modified for use in children. Br J Oral Maxillofac Surg. 1999; 37:129–133. PMID: 10371319.

11. Lezcano FJ, Cagigal BP, Cantera JM, de la Peña Varela G, Blanco RF, Hernández AV. Technical note: medial approach for proximal tibia bone graft using a manual trephine. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007; 104:e11–e17. PMID: 17482845.
12. Marchena JM, Block MS, Stover JD. Tibial bone harvesting under intravenous sedation: morbidity and patient experiences. J Oral Maxillofac Surg. 2002; 60:1151–1154. PMID: 12378490.

13. Hughes CW, Revington PJ. The proximal tibia donor site in cleft alveolar bone grafting: experience of 75 consecutive cases. J Craniomaxillofac Surg. 2002; 30:12–16. PMID: 12064877.

14. Thor A, Farzad P, Larsson S. Fracture of the tibia: complication of bone grafting to the anterior maxilla. Br J Oral Maxillofac Surg. 2006; 44:46–48. PMID: 15907349.

15. Alt V, Meeder PJ, Seligson D, Schad A, Atienza C Jr. The proximal tibia metaphysis: a reliable donor site for bone grafting? Clin Orthop Relat Res. 2003; (414):315–321. PMID: 12966306.

16. Vittayakittipong P, Nurit W, Kirirat P. Proximal tibial bone graft: the volume of cancellous bone, and strength of decancellated tibias by the medial approach. Int J Oral Maxillofac Surg. 2012; 41:531–536. PMID: 22133867.

17. Gerressen M, Riediger D, Marx R, Saxe J, Ghassemi A. Stability behavior of human tibias after bone removal--comparative examination in 15 cadaver tibia pairs. J Oral Maxillofac Surg. 2010; 68:60–67. PMID: 20006156.

18. Morrison JB. The mechanics of the knee joint in relation to normal walking. J Biomech. 1970; 3:51–61. PMID: 5521530.

19. Nisell R. Mechanics of the knee. A study of joint and muscle load with clinical applications. Acta Orthop Scand Suppl. 1985; 216:1–42. PMID: 3865491.




 PDF
PDF ePub
ePub Citation
Citation Print
Print












 XML Download
XML Download