Abstract
Objectives
Papilloma frequently develops as a benign tumor of the head and neck area, but its potential for malignant transformation has yet to be studied. This study aims to provide basic information for papillomas using the immunohistochemical staining of matrix metalloproteinase 2 (MMP-2) and human papilloma virus (HPV) 16 and 18.
Materials and Methods
To evaluate the malignant transformation of papillomas, the selected tissue samples were serially diagnosed with pre-cancerous papilloma (with epithelial dysplasia, pseudo-epitheliomatous hyperplasia) or malignant lesion (squamous cell carcinoma, SCC) after the first diagnosis (squamous papilloma, inverted papilloma). The selected tissues were stained with an antibody to MMP-2 and HPV 16-E7, HPV 18-L1. A statistical analysis was performed according to each transformation step.
Results
The epithelial layer of papilloma and pre-cancerous papilloma lesions had a similar MMP-2 expression, but that of the malignant lesion had a significantly increased MMP-2 expression. HPV 16 and 18 infection rates were 28.6%, 33.3% and 63.6% in papillomas, pre-cancerous papilloma lesions, and SCC.
Human papilloma is defined as a benign neoplasm that may involve the oral, nasal, and sinus cavities, larynx, and pharynx. Many of the human papillomas are known to be induced by human papilloma virus (HPV)1. It can be associated with malignancy, albeit rarely. In some cases, the lesion is diagnosed as benign or chronic inflammation with biopsy even though it shows malignant change clinically. Poor prognosis delays proper treatment.
HPV is detected in almost all uterine cervical cancers. The HPV 16, 18, 31, 33, and 35 subtypes are cited as causes of cervical cancer. The HPV 16 and 18 subtypes are most dominant2.
Recent studies report that HPV has an important role in carcinogenesis and metastasis on the head and neck area2-4. HPV infection is reported in about 15-25% of oral squamous cell carcinoma (SCC). The HPV 16 subtype is the most common (90%), with HPV 18 reported in about 2-4%5-7.
Matrix metalloproteinase 2 (MMP-2) erodes the collagen of the basement membrane, making tumor cells penetrate into the basement membrane and metastasize into surrounding tissues8. Likewise, many studies on the influence of MMP-2 expression on cancer are reported9,10. The expression of MMP is also observed in oral cancer, with enhanced MMP-2, 9 expression reported in a higher degree of malignancy11,12.
In cervical cancer, increased expression and activation of MMP with infection of HPV are reported rather than the case of no HPV infection13; some studies report that HPV infection and over-expression of MMP-2, 9 are related to the malignant transformation of inverted papilloma14.
This study sought to identify the expression of MMP-2 and infection of high-risk HPV on malignantly mutated papilloma and such influences.
Selected tissue samples were serially diagnosed with pre-can cerous papilloma (with epithelial dysplasia, pseudoepitheliomatous hyperplasia) or malignant lesion (SCC) after the first diagnosis with squamous papilloma or inverted papilloma.
For the control group, lesions diagnosed as papilloma but did not show any recurrence or malignant transformation were used. This study was approved by the Institutional Review Board of Kyungpook National University Hospital (IRB No. KNUH-2012-07-005).
Tissue sections were deparaffinized and placed in 3% hydrogen peroxide for 3 minutes to block the endogenous peroxidase activity. The step of immersing in sodium citrate buffer (pH 6.0) and subjecting to microwave irradiation for 10 minutes (110℃) was used. Blocking reagent (UltraTek HRP; ScyTek Laboratories Inc., Logan, UT, USA) was applied for 10 minutes, and primary antibody (mouse monoclonal anti-human gelatinase A, clone A-Gel VC2, 1 : 400 dilution; Neomarkers, Fremont, CA, USA) was reacted. Secondary antibody with biotin and peroxidase reagent with avidin were involved, and DAB chromogen was developed. Counter staining was done with haematoxylin.
As negative control, samples were reacted with phosphate-buffered saline instead of primary antibody. As positive control, we used uterine cervical cancer tissues.
Tissue sections were deparaffinized and placed in 3% hydrogen peroxide for 3 minutes to block the endogenous peroxidase activity. The step of immersing in sodium citrate buffer (pH 6.0) and subjecting to microwave irradiation for 10 minutes (110℃) was used. Blocking reagent was applied for 10 minutes, and primary antibody (1 : 50 diluted HPV 16-E7 antibody; Zymed Laboratories Inc., San Francisco, CA, USA) was reacted. Secondary antibody with biotin and peroxidase reagent with avidin were involved, and DAB chromogen was developed. Counter staining was done with haematoxylin.
For HPV 18 staining, 1 : 20 diluted HPV 18-L1 antibody (Novocastra, Newcastle, UK) was used as primary antibody.
We selected 5 fields for each slide randomly and recorded them using a microscope with digital camera (×100, Olympus-Bx41; Olympus Optical, Tokyo, Japan). The expression level was described as negative, weak, moderate, and strong according to the amount of positive cells.
For the epithelium, the expression level of MMP-2 was considered as follows: (-), negative (no positively stained epithelial cells); (+), weak (mild positive, partially stained in granular or spinous layer); (++), moderate (positively stained in the overall epithelium except stratum corneum), and; (+++), strong (positively stained in the entire epithelium).
For connective tissue (CT): (-/+), weak (positively stained in some fibroblasts); (++), moderate (positively stained in most of the fibroblasts); (+++), strong (positively stained in almost all fibroblasts).
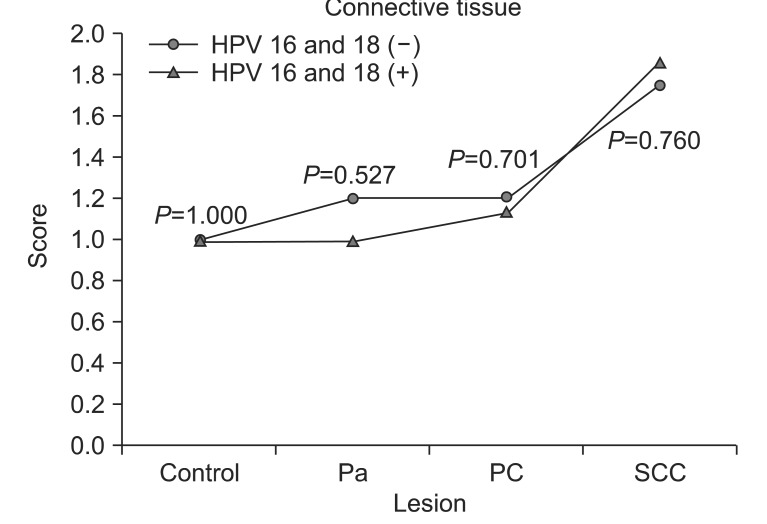
A total of 21 patients (male: 15, female: 6) were included this study. The mean age of the study group was 58.3 years (range, 30-79 years), and 39 tissues were examined.(Table 1)
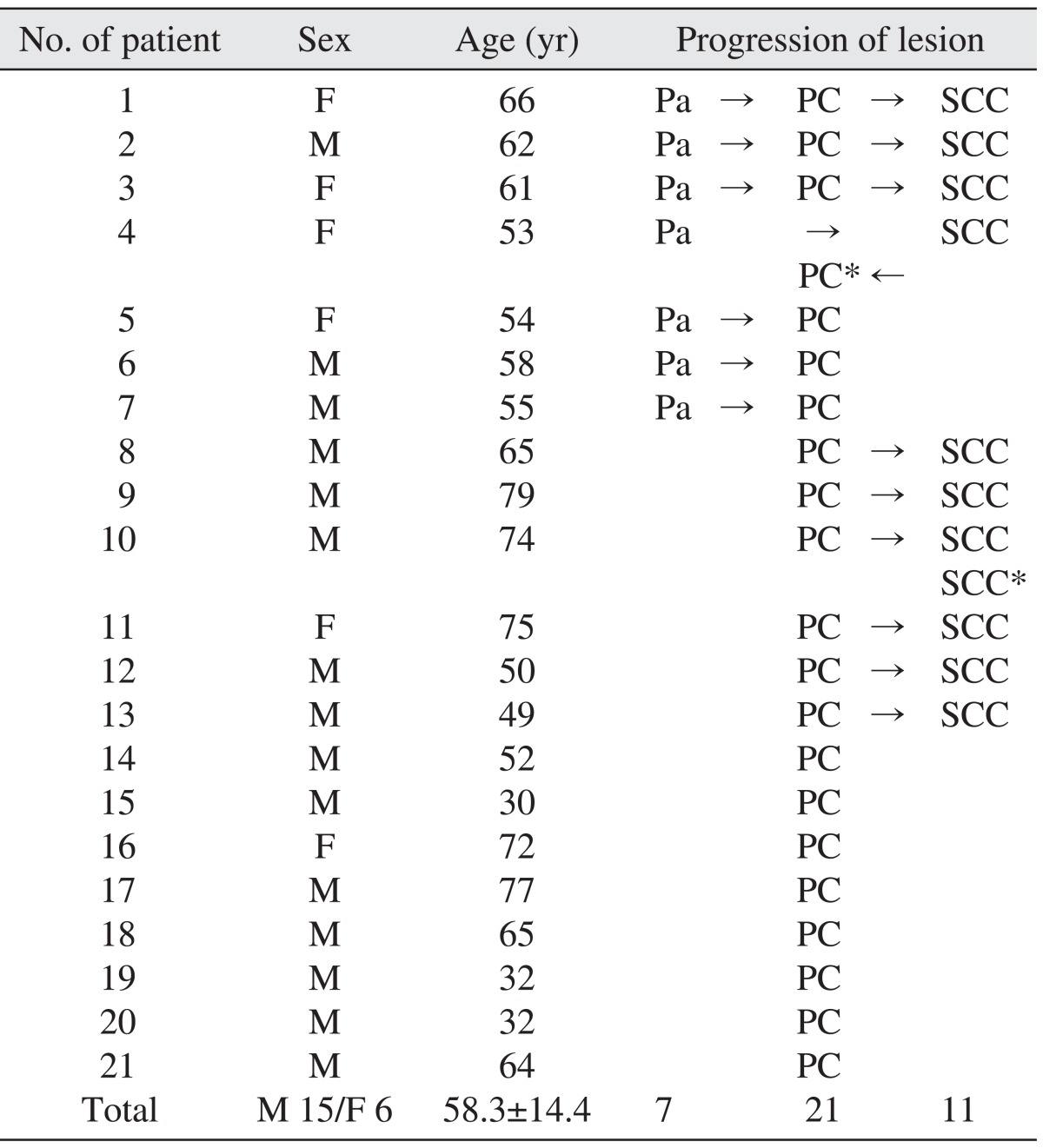
At least 35 tissues of benign papilloma were examined as control group. The mean age of the control group was 48.3 years (range, 8-84 years). The tumor sites of the study group are listed in Table 2.
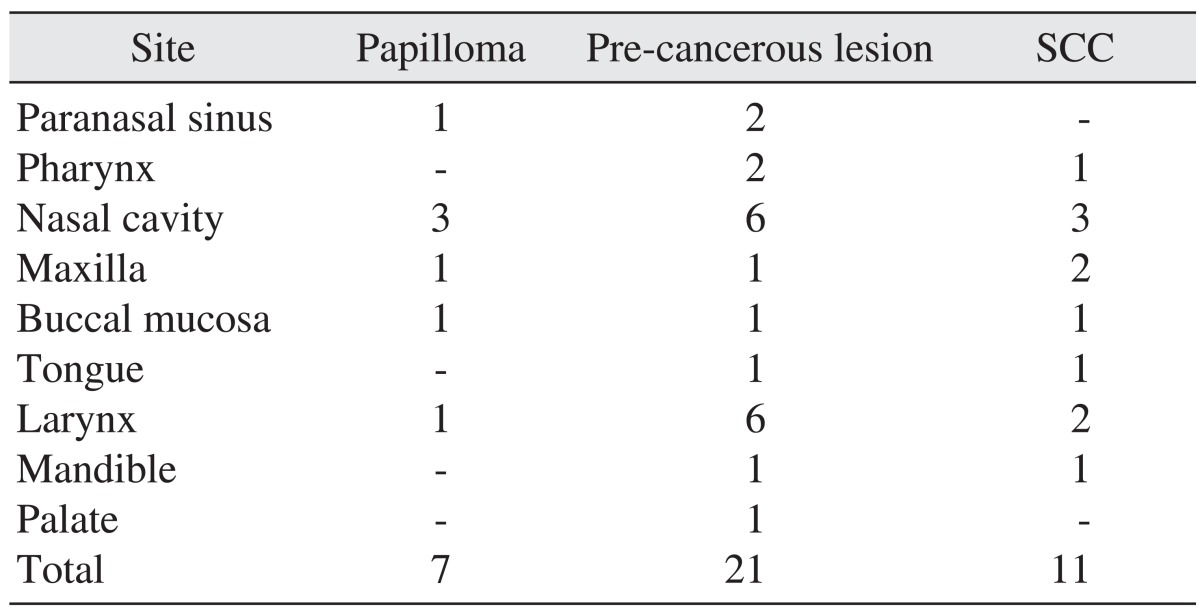
The expression levels of MMP-2 in papilloma, pre-cancerous papilloma, and SCC are presented in Table 3. The result of immunohistochemical staining is shown in Fig. 1. These results revealed that the expression levels of MMP-2 increased in pre-cancerous papilloma and SCC than normal papilloma. The control group exhibited 6 negative, 22 weak, and 7 moderate cases in the expression levels of MMP-2.
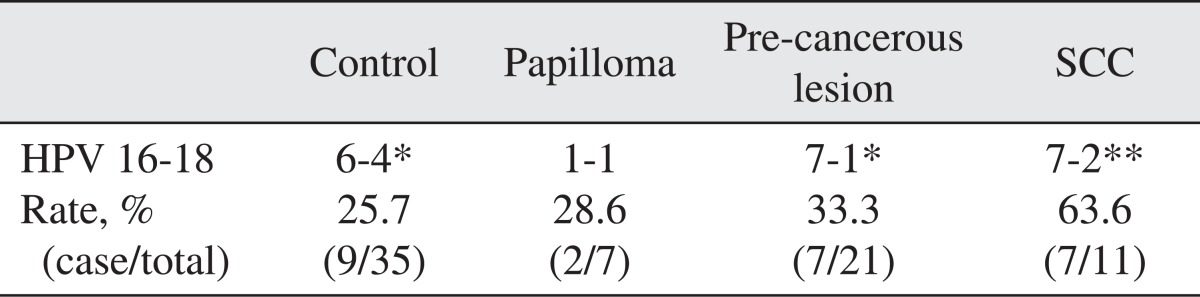
In the papilloma study group, infection of HPV 16 was found in 1 case, and that of HPV 18 in 1 case. For pre-cancerous papilloma, infection of HPV 16 was identified in 5 cases, and that of HPV 18 in 1 case. Double infection of HPV 16 and 18 was found in 1 case of pre-cancerous papilloma. The infection rate of HPV 16 or 18 was 28.6% in the papilloma group and 33.3% in pre-cancerous papilloma.
Concerning SCC, all cases showed koilocytosis as evidence of HPV infection.(Figs. 2, 3) Infection of HPV 16 was found in 7 cases, and that of HPV 18, in 2 cases. Double infection of HPV 16 and 18 was found in 2 cases. The infection rate of HPV 16 or 18 was 63.6% in the SCC group, which was an increased outcome compared with the pre-stage lesions. In the control group, 16 cases showed infection of HPV, and 4 cases, HPV 18 infection; double infection of HPV 16 and 18 was noted in 1 case.(Table 4)
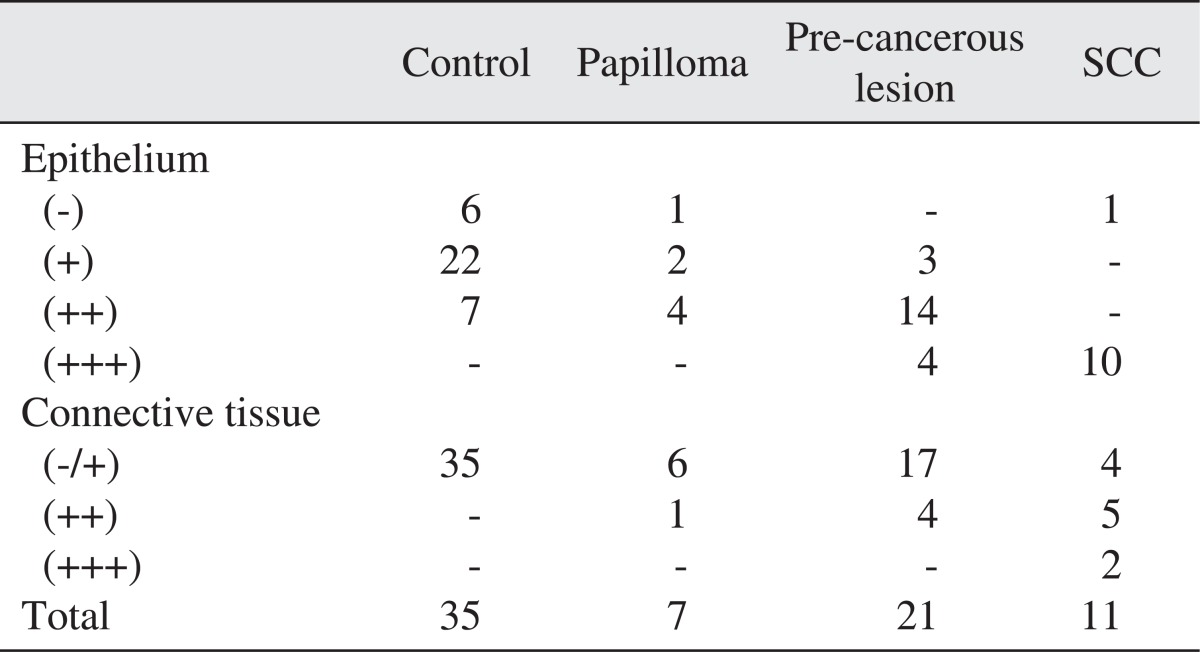
For statistical analysis, we assigned scores according to the degree of expression. In the epithelium, the expression of MMP-2 was scored from 0 (for negative) to 3 (for strong). In CT, it was scored from 1 (for weak) to 3 (for strong).
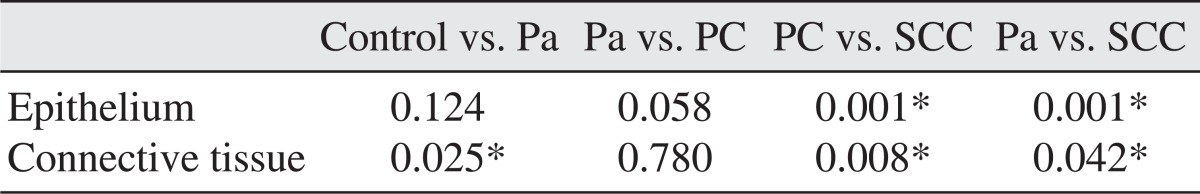
In the papilloma, there was no statistical difference in the expression of MMP-2 between the study and control groups. The epithelium of pre-cancerous lesion showed slightly higher expression of MMP rather than papilloma, but the difference was not statistically significant. Neither was there statistical difference in CT.
SCC exhibited higher expression of MMP-2 than pre-cancerous papilloma or papilloma.(Table 5)
The carcinogenesis, invasion, and metastasis of tumor cell are the result of molecular biological multi-step processes. Proper sequences are needed for tumor cells to invade and metastasize15. First, tumor cells should be separated before they subsequently attach to extracellular matrix (ECM) and invade into surrounding tissues.
Most MMPs are secreted as pro-matrixin and activated by surrounding tissue, plasma proteinase, or bacterial proteinase11. In tumor cells, pro-matrixin is activated in a special membrane called invadopodia. The activated MMP is regulated as compound with tissue inhibitors of metalloproteinases (TIMPSs). MMP is a kind of enzyme that raises the turn-over rate of the ECM proteins-related formation of CT and invasion of tumor.
Thus, the degeneration of basement membrane is an essential process for the progression of tumor. Type IV collagen is the major composition of the basement membrane.
MMP-2 can degenerate the basement membrane by the decomposition of type IV collagen. As a result, it plays an essential role in the invasion of tumor16. Because of such destructive potential, MMP should be precisely regulated. Therefore, we can figure out the invasive growth of tumor cells by analyzing the expression of MMP-2. Davies et al.17 reported the enhanced activation of MMP-2 with the presence of tumor for benign or malignant breast tumors. Some studies also reported that the invasion of tumor was related to the activation of MMP-218. A model study, too, reported decreased invasion of tumor and metastasis with the suppression of MMP-2.
Kim et al.12 analyzed the expression of MMP-2 in irrigation fibroma, leukoplakia, and oral SCC and reported the enhanced expression of MMP-2 in those lesions compared to normal oral mucosa. Moreover, Duffy et al.19 reported that the activation of MMP-2 and MMP-9 increased in malignant tumor than benign tumor in general. In our study, the expression of MMP-2 in epithelium and CT was not statistically significant but increased with the progression of lesion from papilloma to pre-cancerous lesion. Likewise, the expression of MMP-2 in change of papilloma to SCC and pre-cancerous papilloma to SCC increased in epithelium and CT, and the difference was statistically significant.
MMPs are synthesized by ECM cells surrounding the tumor cells rather than tumor cells, suggesting tumor cell-stromal cell co-operation20. Analyzing the expression of MMPs may be essential in predicting the prognosis of tumor, although tumor cells do not produce MMPs themselves16,20. The result of this study showed significant difference of MMP-2 expression in papilloma--control group and papilloma--study group. Papillomas without any pre-cancerous or malignant change showed weak or decreased expression of MMP-2; in contrast, papillomas in the study group showed higher expression of MMP-2. This implies that papillomas in the study group may have higher potential to be invasive lesions.
The infection of HPV is related to several kinds of cancer. After the first study has been reported21, i.e., there are relations between HPV infection and benign or malignant tumor in the head and neck area, many studies were conducted. In 1995, International Agency for Research on Cancer (IARC)22 reported that HPV 16 and 18 caused malignancy in humans. Arndt et al.23 researched the subtypes of HPV in papilloma and leukoplakia on oral and laryngeal region. They found HPV 6, 11 in most of the papilloma and reported that high-risk HPV 16 is in 22% of papilloma and 36% of pre-cancerous papilloma. Gillison et al.6 reported that HPV 16 caused head and neck cancer even in patients who have not been exposed to tobacco or alcohol.
About 25% of head and neck cancers were reported to be related to the infection of HPV5-7. Miller and White24 inspected HPV in head and neck SCC with polymerase chain reaction (PCR) and reported the infection of HPV on 15.8-34.5% of the lesion. In 2001, Miller and Johnstone25 reported the result of a 15-year research (1982-1997) on the relation of oral SCC with the infection of HPV. According to them, HPV can be a risk factor of SCC, and the presence of HPV indicated 0-100%.
In our study, the infection of HPV 16 and 18 was examined with immunohistochemistry. We found one case each for infection of HPV 16 and 18 in a total of 7 cases. In pre-cancerous papilloma, 7/21 cases showed the infection of HPV 16 and double infection was found in 1 case. In SCC, 7/11 cases showed the infection of HPV 16 and double infection was found in 2 cases. In control group, infection rate of HPV 16 was 25.7% and 28.6% for HPV 18.
Although the expression levels of MMP-2 were not significantly different, pre-cancerous papilloma exhibited somewhat higher levels of MMP-2 than papilloma. The infection rate of HPV 16 and 18 was slightly higher in pre-cancerous papilloma than papilloma, but there were hardly differences. Nevertheless, the expression level of MMP-2 significantly increased as pre-cancerous lesions becoming malignant lesion and infection rate of HPV almost doubled. Concerning the study reporting that the infection of HPV is related to the expression of MMP-213, this result suggests that the infection of high-risk HPV may play an important role in the early stage of malignant transformation. As part of their research on MMP-2 and MMP-9 with regard to malignant transformation, Katori et al.14 also stated that the early infection of HPV must be related to malignant transformation.
Our study did not include more reliable or exact methods such as PCR analysis in HPV-type screening; only a small number of samples were analyzed. Despite such limitations, this study yielded useful results by tracking the series of mutations from the papilloma to pre-cancerous lesions and malignant lesion. Moreover, the evaluation of the expression of MMP-2 and high-risk HPV screening with immunohistochemistry is easily applicable to clinical practice because it does not require HPV gene screening. Therefore, papillomas with moderate or higher MMP-2 expression and infection of HPV should be considered to be likely to be changed into pre-cancerous or malignant lesions, in which case long-term follow-up is needed.
This study showed that the moderate or higher expression of MMP-2 and infection of high-risk HPV in papilloma may indicate potential malignancy. Consequently, in clinical diagnosis, the evaluation of the expression of MMP-2 and high-risk HPV screening can help us predict the malignant transformation of papilloma and improve patients' prognosis.
References
1. Sapp JP, Eversole LR, Wysocki GP. Contemporary oral and maxillofacial pathology. St. Louis: Mosby;1997.
2. Underbrink MP, Hoskins SL, Pou AM, Albrecht T. Viral interaction: a possible contributing factor in head and neck cancer progression. Acta Otolaryngol. 2008; 128:1361–1369. PMID: 18607925.

3. Atula S, Auvinen E, Grenman R, Syrjänen S. Human papillomavirus and Epstein-Barr virus in epithelial carcinomas of the head and neck region. Anticancer Res. 1997; 17:4427–4433. PMID: 9494545.
4. Umudum H, Rezanko T, Dag F, Dogruluk T. Human papillomavirus genome detection by in situ hybridization in fine-needle aspirates of metastatic lesions from head and neck squamous cell carcinomas. Cancer. 2005; 105:171–177. PMID: 15822131.

5. Capone RB, Pai SI, Koch WM, Gillison ML, Danish HN, Westra WH, et al. Detection and quantitation of human papillomavirus (HPV) DNA in the sera of patients with HPV-associated head and neck squamous cell carcinoma. Clin Cancer Res. 2000; 6:4171–4175. PMID: 11106228.
6. Gillison ML, Koch WM, Capone RB, Spafford M, Westra WH, Wu L, et al. Evidence for a causal association between human papillomavirus and a subset of head and neck cancers. J Natl Cancer Inst. 2000; 92:709–720. PMID: 10793107.

7. Scheckenbach K, Lieven O, Götte K, Bockmühl U, Zotz R, Bier H, et al. p53 codon 72 polymorphic variants, loss of allele-specific transcription, and human papilloma virus 16 and/or 18 E6 messenger RNA expression in squamous cell carcinomas of the head and neck. Cancer Epidemiol Biomarkers Prev. 2004; 13:1805–1809. PMID: 15533911.
8. Kähäri VM, Saarialho-Kere U. Matrix metalloproteinases and their inhibitors in tumour growth and invasion. Ann Med. 1999; 31:34–45. PMID: 10219712.
9. Mook OR, Frederiks WM, Van Noorden CJ. The role of gelatinases in colorectal cancer progression and metastasis. Biochim Biophys Acta. 2004; 1705:69–89. PMID: 15588763.

10. Roomi MW, Ivanov V, Kalinovsky T, Niedzwiecki A, Rath M. Modulation of human renal cell carcinoma 786-0 MMP-2 and MMP-9 activity by inhibitors and inducers in vitro. Med Oncol. 2006; 23:245–250. PMID: 16720925.

11. Thomas GT, Lewis MP, Speight PM. Matrix metalloproteinases and oral cancer. Oral Oncol. 1999; 35:227–233. PMID: 10621841.

12. Kim MK, Lee EH, Kim J, Lee EW, Cha IH. Immunohistochemical study on expression of MMP-2 and MMP-9 in irritation fibroma, oral leukoplakia and oral squamous cell carcinoma. J Korean Assoc Oral Maxillofac Surg. 2006; 32:352–359.
13. da Silva Cardeal LB, Brohem CA, Corrêa TC, Winnischofer SM, Nakano F, Boccardo E, et al. Higher expression and activity of metalloproteinases in human cervical carcinoma cell lines is associated with HPV presence. Biochem Cell Biol. 2006; 84:713–719. PMID: 17167534.
14. Katori H, Nozawa A, Tsukuda M. Increased expression of matrix metalloproteinase-2 and 9 and human papilloma virus infection are associated with malignant transformation of sinonasal inverted papilloma. J Surg Oncol. 2006; 93:80–85. PMID: 16353190.

15. Chambers AF, Matrisian LM. Changing views of the role of matrix metalloproteinases in metastasis. J Natl Cancer Inst. 1997; 89:1260–1270. PMID: 9293916.

16. Curran S, Murray GI. Matrix metalloproteinases in tumour invasion and metastasis. J Pathol. 1999; 189:300–308. PMID: 10547590.

17. Davies B, Miles DW, Happerfield LC, Naylor MS, Bobrow LG, Rubens RD, et al. Activity of type IV collagenases in benign and malignant breast disease. Br J Cancer. 1993; 67:1126–1131. PMID: 8494711.

18. Tokuraku M, Sato H, Murakami S, Okada Y, Watanabe Y, Seiki M. Activation of the precursor of gelatinase A/72 kDa type IV collagenase/MMP-2 in lung carcinomas correlates with the expression of membrane-type matrix metalloproteinase (MT-MMP) and with lymph node metastasis. Int J Cancer. 1995; 64:355–359. PMID: 7591310.

19. Duffy MJ, Maguire TM, Hill A, McDermott E, O'Higgins N. Metalloproteinases: role in breast carcinogenesis, invasion and metastasis. Breast Cancer Res. 2000; 2:252–257. PMID: 11250717.

20. Jones JL, Walker RA. Control of matrix metalloproteinase activity in cancer. J Pathol. 1997; 183:377–379. PMID: 9496252.

21. Gissmann L, Diehl V, Schultz-Coulon HJ, zur Hausen H. Molecular cloning and characterization of human papilloma virus DNA derived from a laryngeal papilloma. J Virol. 1982; 44:393–400. PMID: 6292500.

22. IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Human papillomaviruses. IARC Monogr Eval Carcinog Risks Hum. 1995; 64:1–378. PMID: 16755705.
23. Arndt O, Johannes A, Zeise K, Brock J. High-risk HPV types in oral and laryngeal papilloma and leukoplakia. Laryngorhinootologie. 1997; 76:142–149. PMID: 9213402.
24. Miller CS, White DK. Human papillomavirus expression in oral mucosa, premalignant conditions, and squamous cell carcinoma: a retrospective review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996; 82:57–68. PMID: 8843455.
25. Miller CS, Johnstone BM. Human papillomavirus as a risk factor for oral squamous cell carcinoma: a meta-analysis, 1982-1997. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001; 91:622–635. PMID: 11402272.

Fig. 1
Immunohistochemical staining of matrix metalloproteinase 2 (MMP-2). (A) shows negative staining of the control group except keratinized layer (×100). (B) illustrates weak immunoreaction to MMP-2 in the papilloma (×100). (C) shows moderate immunoreaction to MMP-2 in the papilloma with dysplasia (×100). (D) exhibits strong immunoreaction to MMP-2 in squamous cell carcinoma, transformed from the papilloma (×100).
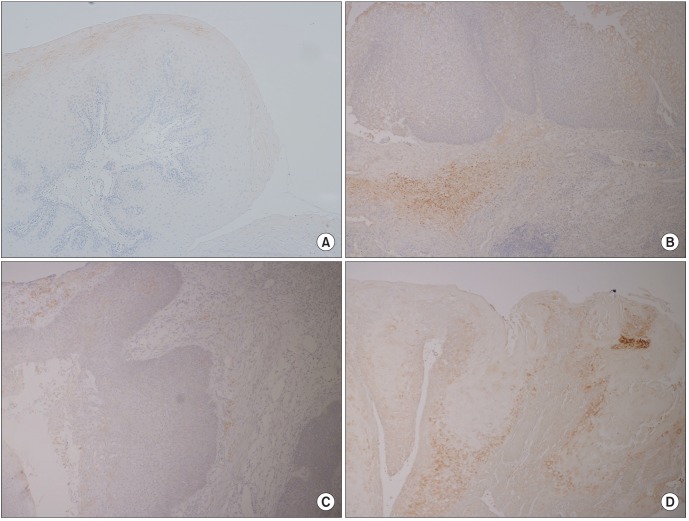
Fig. 2
Koilocytosis is noted, with the epithelial layer showing positive immunoreactivity to human papilloma virus 16 (×400).
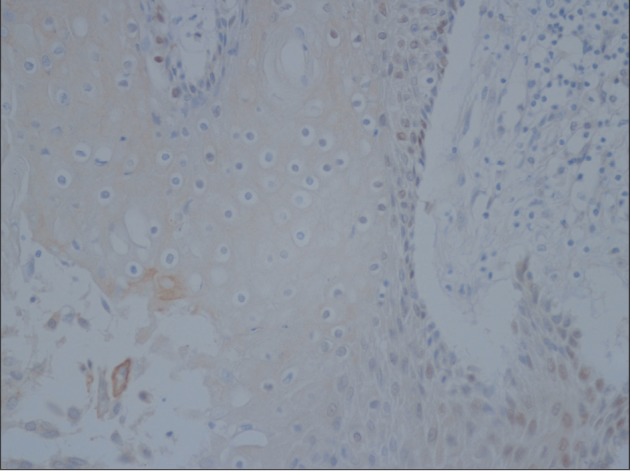
Fig. 3
Epithelial cells showing koilocytosis reacting positively to human papilloma virus 18 antibody (×400).
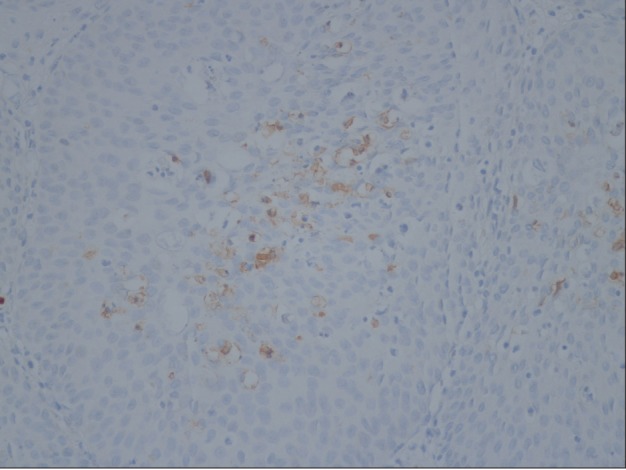
Fig. 4
MMP-2 expression score and HPV 16 and 18 infection for each lesion in the epithelium. *P<0.05. (MMP-2: matrix metalloproteinase 2, HPV: human papilloma virus, Pa: papilloma, PC: pre-cancer lesion, SCC: squamous cell carcinoma)
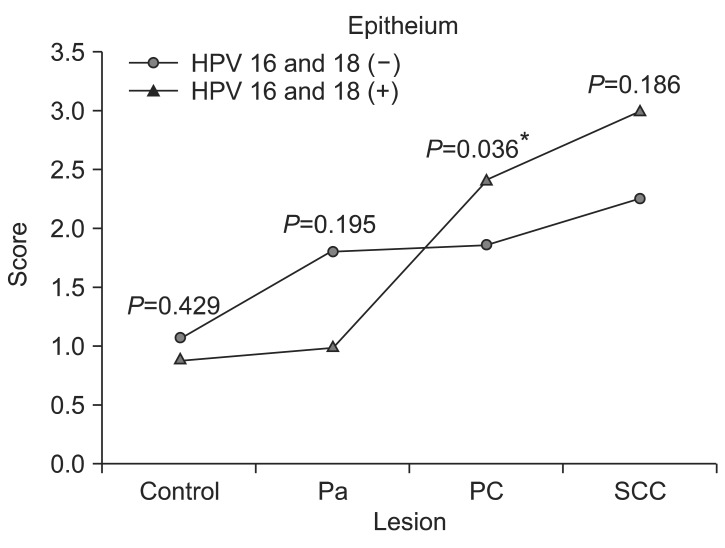
Fig. 5
MMP-2 expression score and HPV 16 and 18 infection for each lesion in connective tissue. (MMP-2: matrix metalloproteinase 2, HPV: human papilloma virus, Pa: papilloma, PC: pre-cancer lesion, SCC: squamous cell carcinoma)




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download