1. Karlis V, Glickman R. Nonsurgical management of temporomandibular disorders. In : Miloro M, Ghali GE, Larsen PE, Waite P, editors. Peterson's principles of oral and maxillofacial surgery. 2004. 2nd ed. Hamilton: BC Decker;p. 949–950.
2. Ohnuki T, Fukuda M, Nakata A, Nagai H, Takahashi T, Sasano T, et al. Evaluation of the position, mobility, and morphology of the disc by MRI before and after four different treatments for temporomandibular joint disorders. Dentomaxillofac Radiol. 2006; 35:103–109. PMID:
16549437.

3. Choi JH, Kim IK, Oh NS, Oh SS, Kim ES, Lee SH, et al. A clinical study in the prognosis of the temporomandibular disorder. J Korean Assoc Oral Maxillofac Surg. 2000; 26:497–506.
4. Peterson LJ. Temporomandibular joint disease. In : Peterson LJ, editor. Contemporary oral and maxillofacial surgery. 1993. 2nd ed. St. Louis: Mosby-Year Book;p. 713–736.
5. Yustin D, Neff P, Rieger MR, Hurst T. Characterization of 86 bruxing patients with long-term study of their management with occlusal devices and other forms of therapy. J Orofac Pain. 1993; 7:54–60. PMID:
8467297.
6. Nitzan DW. Intraarticular pressure in the functioning human temporomandibular joint and its alteration by uniform elevation of the occlusal plane. J Oral Maxillofac Surg. 1994; 52:671–679. PMID:
8006730.

7. Sato S, Kawamura H, Motegi K. Management of nonreducing temporomandibular joint disk displacement. Evaluation of three treatments. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995; 80:384–388. PMID:
8521099.
8. Barkin S, Weinberg S. Internal derangements of the temporomandibular joint: the role of arthroscopic surgery and arthrocentesis. J Can Dent Assoc. 2000; 66:199–203. PMID:
10789172.
9. Alkan A, Kilic E. A new approach to arthrocentesis of the temporomandibular joint. Int J Oral Maxillofac Surg. 2009; 38:85–86. PMID:
19108990.

10. Alpaslan C, Kahraman S, Güner B, Cula S. Does the use of soft or hard splints affect the short-term outcome of temporomandibular joint arthrocentesis? Int J Oral Maxillofac Surg. 2008; 37:424–427. PMID:
18356022.

11. Dworkin SF, LeResche L. Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J Craniomandib Disord. 1992; 6:301–355. PMID:
1298767.
12. American Association of Oral and Maxillofacial Surgeons. 1984 criteria for TMJ meniscus surgery. 1984. Chicago: The Association;p. 1–40.
13. Nitzan DW, Dolwick MF, Martinez GA. Temporomandibular joint arthrocentesis: a simplified treatment for severe, limited mouth opening. J Oral Maxillofac Surg. 1991; 49:1163–1167. PMID:
1941330.

14. Holmlund A, Hellsing G. Arthroscopy of the temporomandibular joint. An autopsy study. Int J Oral Surg. 1985; 14:169–175. PMID:
3920161.
15. McCain JP. Arthroscopy of the human temporomandibular joint. J Oral Maxillofac Surg. 1988; 46:648–655. PMID:
3165118.

16. Carraro JJ, Caffesse RG. Effect of occlusal splints on TMJ symptomatology. J Prosthet Dent. 1978; 40:563–566. PMID:
281508.

17. de Leeuw R, Boering G, Stegenga B, de Bont LG. Symptoms of temporomandibular joint osteoarthrosis and internal derangement 30 years after non-surgical treatment. Cranio. 1995; 13:81–88. PMID:
8697504.

18. Emshoff R. Clinical factors affecting the outcome of occlusal splint therapy of temporomandibular joint disorders. J Oral Rehabil. 2006; 33:393–401. PMID:
16671984.

19. Chung SC, Kim HS. The effect of the stabilization splint on the TMJ closed lock. Cranio. 1993; 11:95–101. PMID:
8495513.

20. Randolph CS, Greene CS, Moretti R, Forbes D, Perry HT. Conservative management of temporomandibular disorders: a posttreatment comparison between patients from a university clinic and from private practice. Am J Orthod Dentofacial Orthop. 1990; 98:77–82. PMID:
2114059.

21. Major PW, Nebbe B. Use and effectiveness of splint appliance therapy: review of literature. Cranio. 1997; 15:159–166. PMID:
9586519.

22. Lundh H, Westesson PL, Eriksson L, Brooks SL. Temporomandibular joint disk displacement without reduction. Treatment with flat occlusal splint versus no treatment. Oral Surg Oral Med Oral Pathol. 1992; 73:655–658. PMID:
1437030.
23. Sanders B. Arthroscopic surgery of the temporomandibular joint: treatment of internal derangement with persistent closed lock. Oral Surg Oral Med Oral Pathol. 1986; 62:361–372. PMID:
3464910.

24. Murakami KI, Iizuka T, Matsuki M, Ono T. Recapturing the persistent anteriorly displaced disk by mandibular manipulation after pumping and hydraulic pressure to the upper joint cavity of the temporomandibular joint. Cranio. 1987; 5:17–24. PMID:
3467862.
25. Nitzan DW, Dolwick MF, Heft MW. Arthroscopic lavage and lysis of the temporomandibular joint: a change in perspective. J Oral Maxillofac Surg. 1990; 48:798–801. PMID:
2374054.

26. Diraçoğlu D, Saral IB, Keklik B, Kurt H, Emekli U, Ozçakar L, et al. Arthrocentesis versus nonsurgical methods in the treatment of temporomandibular disc displacement without reduction. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009; 108:3–8. PMID:
19272808.
27. Kropmans TJ, Dijkstra PU, Stegenga B, de Bont LG. Therapeutic outcome assessment in permanent temporomandibular joint disc displacement. J Oral Rehabil. 1999; 26:357–363. PMID:
10373081.

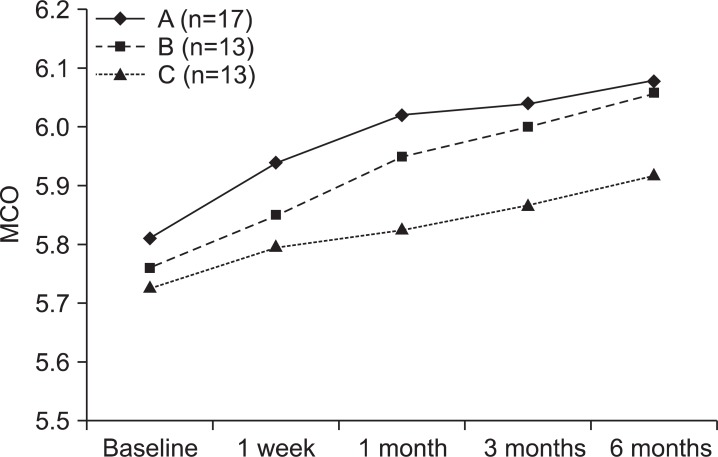
28. Park YH, Lee SH, Yoon HJ. An effect of combination with arthrocentesis and stabilization splint treatment on temporomandibular joint disorder patient. J Korean Assoc Maxillofac Plast Reconstr Surg. 2010; 32:32–36.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download