This article has been corrected. See "Erratum" in Volume 38 on page 256.
Abstract
Objectives
This study sought to evaluate trabecular changes in the mandible using fractal analysis and to explain the transient osteopenia related to rapid orthodontic tooth movement after orthognathic surgery.
Materials and Methods
Panoramic radiographs were taken of 26 patients who underwent bilateral sagittal split ramus osteotomy. Radiographs taken before the surgery and 1 month after surgery were overlapped, and 40×40 pixel square regions of interest were selected near the mandibular canines and 1st molars. After the image processing procedure, the fractal dimension was calculated using the box-counting method.
Introduced by Mandelbrot in 1983, fractal means geometry based on self-similarity and decimal dimension, e.g., part of lightning or river resembles the entire shape of lightning or river1. Based on this concept, it is possible to identify the shape and structure of an object using fractal analysis, and they are expressed numerically using fractal dimension (FD). In other words, FD increases or decreases according to the complexity of the object2.
Fractal structure with self-similarity is not only in nature but in the human body as well, such as bronchial tubes, blood vessel, and convolutions of the brain. Therefore, many research studies have been conducted using fractal analysis to identify the complexity of shapes and structures in the human body3-5. In the dentistry field, Cha et al.6 selected a region of interest (ROI) in the mandible alveolar bone of furcation involvement and alveolar ridge from 30 radiographs of the normal periapical area and 30 radiographs of periodontitis patients' periapical area to compare FD. Since the difference was statistically significant, they reported that fractal analysis is a useful method for diagnosing periodontitis. Rothe et al.7 investigated the relationship between the relapse of mandibular incisors crowding and the amount/structure of mandible by applying fractal analysis to photos of dental cast model, lateral cephalometric radiographs, and periapical area radiographs of patients who had completed orthodontic treatment for more than 10 years, which were taken at the first examination, end of treatment, and 10 years after the treatment; according to them, thinner cortical bone in the mandible increases the rate of relapse. Similarly, Wagle et al.8 reported that, after applying orthodontic force to the first molar of Sprague-Dawley rat for 6 hours to manufacture dried and demineralized tooth samples and calculating FD in the periodontal ligament and bone interface, FD increases in proportion to the orthodontic force. Research studies using radiographs and fractal analysis have also been used widely in dental prosthetics because the latter is noninvasive; moreover, FD is not greatly affected by the amount of exposure and projection angle of radiographs9.
In clinical orthodontics, rapid tooth movement is often performed temporarily during the treatment after orthognathic surgery. It is called RAP. Introduced by Frost, RAP is a tendency wherein treatment is accelerated because excessive bone metabolic products are concentrated during the healing of the damaged structure. It is also called transient osteopenia10-13. Park et al.14 and Gwack et al.15 conducted a immunohistochemical research and found that tooth movement is accelerated under cortical punching in the palate of rats. Note, however, that aggressive bone remodeling may have undesirable side effects due to rapid tooth movement during the treatment after surgery. Though some researchers performed biological and histological analysis on orthodontic tooth movement and RAP, very few radiological research studies have been conducted16-18.
Therefore, we conducted this study to evaluate the change of sponge bones around teeth caused by orthognathic surgery using panoramic radiographs before/after orthognathic surgery and fractal analysis.
Panoramic radiographs taken of 26 patients (13 are male and 13 are female) who visited Department of Orthodontics in Pusan National University Dental Hospital, who were diagnosed with skeletal malocclusion, and who underwent bilateral sagittal split ramus osteotomy (BSSRO) were selected. The average age of the patients was 23.1±2.7, and there was no specific medical history. Panoramic radiographs were taken before the surgery (stage 0) and 1 month after the surgery (stage 1) (PM 2002 CC, Planmeca, Helsinki, Finland).
Panoramic radiographs of digitalized stage 0 and stage 1 were overlapped to match the apex/root apex of canine, crown/mesiodistal root apex of the first molar using Photoshop version 7.0 (Adobe Systems Inc., San Jose, CA, USA). In this process, any vertical distortion of stage 0 and stage 1 panoramic radiographs was corrected. Afterward, near both mandibular canines whose hyoid bone is not overlapped in the opposite mandible angle and trabecular bone in the root apex of the first molars, 40×40 pixel ROI were selected based on stage 0 and stage 1 panoramic radiographs (Fig. 1), and 104 samples were collected at 4 pairs per patient.
All ROI images obtained from stage 0 and stage 1 panoramic radiographs (n=104) were processed according to the method developed by White and Rudolph18 as follows: first, the fine and middle-sized structures were removed with Gaussian filter (sigma=20 pixel), and the original images (Fig. 2. A) were blurred (Fig. 2. B); these blurred images were deducted from the original images, and 128 was added to make binary images (Fig. 2. C); to reduce noise, binary images were eroded and dilated once and processed as skeletonized images.(Fig. 2. D)
The FD of all skeletonized images obtained by the image processing procedure was calculated by box-counting method using Image J software 1.40 g (National Institutes of Health, Bethesda, Maryland, USA). The change of FD of stage 0 and stage 1 was analyzed, and the change before/after surgery was then calculated by canine area and first molar area. Finally, the change in the canine area and the first molar area was compared and evaluated.
To verify tester error, the same tester measured all measure -ment items among 8 randomly selected people after 7 days. In the intraclass correlation, the mean measurement error was 0.02±0.01 in the canine area and 0.01±0.01 in the first molar area. Standard error was measured by Dahlberg's formula (error of method2=Σd2/2n, d=difference of the first and second measurement, n=number of measurement). The standard error of the canine area was 0.016, and that of the first molar area was 0.004. The difference in the measurement error of the tester in this study was not statistically significant.
The difference of FD between stage 0 and stage 1 was analyzed by paired t-test, and the relationship between the change of the canine area and the first molar area was evaluated by independent t-test. All statistical processes were done using the SPSS version 12.0k (SPSS Inc., Chicago, IL, USA) program.
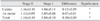
The mean FD of ROI was 1.14±0.10 before BSSRO (stage 0) and 1.04±0.10 after BSSRO (stage 1), and the difference was statistically significant (P<0.05).(Table 1) The mean FD in the mandible canine area before surgery was 1.16±0.10 but decreased to 1.04±0.11 after surgery, and the difference was statistically significant (P<0.05).(Table 1) In the first molar area, the mean FD before surgery was 1.12±0.09 and 1.05±0.08 after surgery. Similar to the canine area, FD decreased, showing statistically significant difference (P<0.05).(Table 1) As a result of comparing and evaluating the change of FD in the canine area and in the first molar area before/after surgery, statistically significant difference was verified (P<0.05).(Table 2)
This study sought to explain transient osteopenia generated in treatment when maxillary bone receives traumatic impact such as orthognathic surgery using panoramic radiographs and fractal analysis and to provide a guide to determining the time of orthodontic treatment after proper surgery. FD is a non-invasive method of measuring and comparing the change of bone density without being affected greatly by the contrast of radiographs and change of projection direction. As such, fractal analysis has been widely used as a diagnosis and evaluation tool, generally for osteoporosis that may cause loss of overall bones and inflammation of alveolar bone6,19.
Ellis et al.20 reported that after SSRO, the surgical site can be cured by direct and indirect osteogenesis based on the rigidity of fixation, and that the medullary space is filled with mature bone until 6 weeks from the surgery. Therefore, loss of bone density after surgery can be explained in the same context. Heo et al.21 also measured FD in the part of BSSRO before the surgery and 1-2 days/1 month/6 months/1 year after the surgery and reported that FD decreased right after the surgery with statistical significance and then increased gradually over time. A statistically significant decrease of FD in ROI before and after surgery is an index of change of bone metabolism and density. In other words, because the trabecular has a typical fractal structure, and FD reflects the trabecular's morphological complexity, FD increases when complexity increases or osteogenesis is in process and decreases when bone density decreases. Note, however, that these research studies investigated the change in maxillary bone near the surgical site, but there were few research studies on the change of trabecular in the maxillary bone around teeth like this study.
In bone damaged by bone fracture, arthropathy, osteotomy, or bone graft, the overall osteopenia process is accelerated due to aspecific inflammatory reaction such as inflammation-mediated osteopenia22. Damaged bone is cured through granulation, callus, modeling, and remodeling stages, with the RAP generated in these stages accelerating the speed of each stage by 2-10 times. Such phenomenon is started within a few days of damage, reaching its peak after 1-2 month(s) and disappearing gradually after 6-24 months12.
Similarly, RAP is a physiological reaction for the rapid remodeling of the surrounding tissue. If teeth are affected during this process, very rapid tooth movement than the tooth movement before orthognathic surgery may occur; this in turn may yield the result of undesirable tooth movement. Through an immunohistochemical research wherein Osteo-protegerin and receptor activator of nuclear factor kappa-B (RANK) ligand- indicators of activity of osteoblast and osteoclast- were more aggressive in rats with cortical punching, Park et al.14 reported that cortical punching caused rapid tooth movement. In addition, Gwack et al.15 reported that the remodeling of connective tissues around tooth was faster in rats with cortical punching.
In this study, FD decreased after orthognathic surgery, showing statistically significant difference (P<0.05); in the comparison of the canine area and the first molar area, it also decreased, and the difference was statistically significant (P<0.05). This means that bone density in panoramic radiographs decreases clinically following orthognathic surgery. Therefore, similar to the research studies of Park et al.14 and Gwack et al.15, rapid tooth movement may result from the loss of bone density right after orthognathic surgery. This suggests the need to prevent undesirable tooth movement by controlling rapid tooth movement right after orthognathic surgery.
Furthermore, in this study, change of FD in the canine area and the first molar area showed statistically significant difference. In particular, there was great difference of bone density in stage 0 and stage 1 of the canine area on the opposite side of the surgical site because, even though overall bone density decreased due to transient osteopenia after orthognathic surgery, the speed of osteogenesis differed since bone metabolism is faster in the first molar near the surgical site due to RAP. In addition, similar to the research of Gwack et al.15, remodeling of not only hard tissue muscles but also soft tissue muscles becomes faster after orthognathic surgery, and proximal segment moves forward and upward whereas distal segment moves backward and downward. As a result, stretching of muscles also caused the difference of bone healing between two areas15,23. Therefore, after orthognathic surgery, it is important not to apply excessive force to maxi-llary bone when using inter-maxillary elastics right after removing the inter-maxillary holder because such may result in the extrusion of all teeth.
As mentioned above, bone metabolism is accelerated by surgery; as a result, the start of tooth movement is fast-tracked from 4-6 weeks to 1-2 week(s) due to transient osteopenia. If a surgeon applied aggressive force in the early orthodontic treatment after surgery and met the patient after 4-6 weeks as in normal orthodontic treatment, however, excessive orthodontic tooth movement may yield an undesirable result. In most cases, orthodontists should inspect the patient weekly in the first month and meet the patient every 2 weeks in the next 2 months. Generally, the interval of visit can be increased 3-4 months after surgery when the early healing stage is finished and occlusion is stabilized24.
In conclusion, with this study, we can verify that overall mandibular bone density is reduced by traumatic impact and assume the reason for rapid tooth movement after orthognathic surgery. This study can provide a guide as to the time and method of orthodontic treatment after orthognathic surgery if more research studies on the healing process after orthognathic surgery are conducted.
To identify the change of cancellous bones around teeth caused by orthognathic surgery using panoramic radiographs before/after the surgery and fractal analysis, this study selected ROI in cancellous bones near both mandibular canines and first molars from the panoramic radiographs of patients who underwent BSSRO and calculated and compared trabecular change before/after surgery. As a result, FD decreased after orthognathic surgery, showing statistically significant difference (P<0.05). The change of FD on the canine side compared with that on the 1st molar side had greater statistical significance (P<0.05).
As mentioned above, this study radio graphi cally identified that orthognathic surgery such as BSSRO decreases overall bone density temporarily and suggests that the reason for rapid tooth movement after orthognathic surgery is related to the RAP. This study can provide a guide as to the time and method of orthodontic treatment after orthognathic surgery if more research studies on the change of mandibular bones after orthognathic surgery are conducted.
Figures and Tables
Fig. 2
Steps used in image processing. A. Original image. B. Blurred image. C. Binary image. D. Skeletonized image.

References
1. Mandelbrot BB. The fractal geometry of nature. 1983. 3rd ed. New York: Freeman Publishing.
2. Mandelbrot BB. Peitgen HO, Jurgens H, Saupe D, editors. Length, area and dimensions: measuring complexity and scaling properties. Chaos and fractals. 1992. 1st ed. New York: Springer-Verlag Publishing;173–214.
3. Podsiadlo P, Dahl L, Englund M, Lohmander LS, Stachowiak GW. Differences in trabecular bone texture between knees with and without radiographic osteoarthritis detected by fractal methods. Osteoarthritis Cartilage. 2008. 16:323–329.

4. Prouteau S, Ducher G, Nanyan P, Lemineur G, Benhamou L, Courteix D. Fractal analysis of bone texture: a screening tool for stress fracture risk? Eur J Clin Invest. 2004. 34:137–142.

5. Lespessailles E, Poupon S, Niamane R, Loiseau-Peres S, Derommelaere G, Harba R, et al. Fractal analysis of trabecular bone texture on calcaneus radiographs: effects of age, time since menopause and hormone replacement therapy. Osteoporos Int. 2002. 13:366–372.

6. Cha SY, Han WJ, Kim EK. Usefulness of fractal analysis for the diagnosis of periodontitis. Korean J Oral Maxillofac Radiol. 2001. 31:35–42.
7. Rothe LE, Bollen AM, Little RM, Herring SW, Chaison JB, Chen CS, et al. Trabecular and cortical bone as risk factors for orthodontic relapse. Am J Orthod Dentofacial Orthop. 2006. 130:476–484.

8. Wagle N, Do NN, Yu J, Borke JL. Fractal analysis of the PDL-bone interface and implications for orthodontic tooth movement. Am J Orthod Dentofacial Orthop. 2005. 127:655–661.

9. Jolley L, Majumdar S, Kapila S. Technical factors in fractal analysis of periapical radiographs. Dentomaxillofac Radiol. 2006. 35:393–397.

10. Frost HM. The regional accelerated phenomenon. Orthop Clin North Am. 1981. 12:725–726.
11. Frost HM. The regional acceleratory phenomenon: a review. Henry Ford Hosp Med J. 1983. 31:3–9.
12. Frost HM. The biology of fracture healing. An overview for clinicians. Part I. Clin Orthop Relat Res. 1989. 248:283–293.
13. Frost HM. Skeletal structural adaptations to mechanical usage (SATMU): 2. Redefining Wolff's law: the remodeling problem. Anat Rec. 1990. 226:414–422.

14. Park WK, Kim SS, Park SB, Son WS, Kim YD, Jun ES, et al. The effect of cortical punching on the expression of OPG, RANK, and RANKL in the periodontal tissue during tooth movement in rats. Korean J Orthod. 2008. 38:159–174.

15. Gwack C, Kim SS, Park SB, Son WS, Kim YD, Jun ES, et al. The expression of MMP-1, -8, and -13 mRNA in the periodontal ligament of rats during tooth movement with cortical punching. Korean J Orthod. 2008. 38:187–201.

16. Verna C, Zaffe D, Siciliani G. Histomorphometric study of bone reactions during orthodontic tooth movement in rats. Bone. 1999. 24:371–379.

17. Melsen B. Biological reaction of alveolar bone to orthodontic tooth movement. Angle Orthod. 1999. 69:151–158.
18. White SC, Rudolph DJ. Alterations of the trabecular pattern of the jaws in patients with osteoporosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999. 88:628–635.

19. Ruttimann UE, Webber RL, Hazelrig JB. Fractal dimension from radiographs of peridental alveolar bone. A possible diagnostic indicator of osteoporosis. Oral Surg Oral Med Oral Pathol. 1992. 74:98–110.
20. Ellis E 3rd, Carlson DS, Billups J. Osseous healing of the sagittal ramus osteotomy: a histologic comparison of rigid and nonrigid fixation in Macaca mulatta. J Oral Maxillofac Surg. 1992. 50:718–723.

21. Heo MS, Park KS, Lee SS, Choi SC, Koak JY, Heo SJ, et al. Fractal analysis of mandibular bony healing after orthognathic surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002. 94:763–767.

22. Schilling T, Muller M, Minne HW, Ziegler R. Influence of inflammation-mediated osteopenia on the regional acceleratory phenomenon and the systemic acceleratory phenomenon during healing of a bone defect in the rat. Calcif Tissue Int. 1998. 63:160–166.

23. Miloro M, Ghali GE, Larsen PE, Waite PD. Peterson's principles of oral and maxillofacial surgery. 2004. 2nd ed. Hamilton: BC Decker Publishing;1259–1260.
24. Miloro M, Ghali GE, Larsen PE, Waite PD. Peterson's principles of oral and maxillofacial surgery. 2004. 2nd ed. Hamilton: BC Decker Publishing;1133–1134.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download