Abstract
Introduction
The location of parotid gland tumors in the superficial or deep lobes can affect the time and difficulty of operations. Therefore, accurate preoperative evaluation of the tumor location is important for surgical outcomes.
Materials and Methods
A total of 16 patients with parotid gland tumors and who underwent a parotidectomy between April 2003 and March 2011 were retrospectively reviewed in terms of demographic background, tumor location, surgical treatment, and treatment outcomes. Tumor location was estimated by four landmarks on contrast enhanced computerized tomography scans, which were Conn's arc, the facial nerve (FN) line, the Utrecht line, and the retromandibular vein. Tumor location was confirmed by relative position depending on the facial nerve during surgery. It was assumed positive since the tumor lies in the superficial lobe of the parotid gland, the sensitivity, specificity, positive predictive value, negative predictive value, and efficiency of each landmark were evaluated.
Results
Our result revealed that the facial nerve line had a sensitivity of 83.3%, specificity of 100%, positive predictive value of 100%, negative predictive value of 71.4%, and efficiency of 87.5%. Some would be more efficient preoperative evaluation methods of the relationship of parotid gland tumors to the facial nerve than others.
Parotidectomy may cause permanent damage to nerve such as facial paralysis and Frey's syndrome after surgery due to the anatomical location of the parotid gland and facial nerve (FN). Superficial parotidectomy causes minimal risk to the FN, whereas surgery for tumors in the deep lobe has a higher rate of FN injury. If total parotidectomy is required, however, the FN would be injured because of exposing FNs even when they are not sacrificed. Therefore, accurate preoperative evaluation of the location of the parotid gland tumor is important for the surgical outcomes and prognosis of patients because its location significantly affects the time and difficulty of operation1-6.
Although the superficial and deep lobe of the parotid gland are not clearly anatomically divided, however, the surgions divide the lobes by FN path clinically. Generally, the location of the tumor is evaluated before operation using imaging examinations such as computed tomography (CT) and magnetic resonance imaging (MRI), but it is difficult to identify the FN with radiographic image only. In addition, if the tumor is larger, it may be hard to identify the location of tumor with only imaging examinations because of the movement of soft tissue around parotid gland including FN7-9. Therefore, there are several methods of anticipating the location of the parotid gland tumor based on the other anatomical reference point on radiographic image, such as Utrecht (U) line1,2, retromandibular vein (RV)1,2, Conn's arc (CA)10, and FN line10,11. In previous research, efficiency was measured differently by case1,2,9-15; as such, this research divided the location of the parotid gland tumor into superficial lobe and deep lobe based on 4 anatomical reference points on CT, compared it with the true location of the tumor in operation, compared methods to analyze the location of the parotid gland tumor, and analyzed their efficiency.
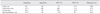
A total of 16 patients with parotid gland tumors and who underwent parotidectomy in Department of Oral and Maxillofacial Surgery, Kyoungpook National University Dental Hospital between April 2003 and March 2011 were retrospectively reviewed.(Table 1) Male patients numbered 6, and female patients numbered 10, with average age of 39.2 (range, 23-62). In the final biopsy result, 13 were diagnosed with a benign tumor (10 pleomorphic adenoma and 3 Warthin's tumor), and 3 patients were malignant tumor (malignant lymphoma, mucoepidermoid carcinoma, and adenocystic carcinoma, respectively). Eleven patients had superficial parotidectomy, and total parotidectomy and subtotal parotidectomy were performed on 2 patients, respectively.
CT (Aquilion 64 TSX101A; Toshiba, Tokyo, Japan) image was obtained by injecting 2 mL/kg contrast (Ultravist; Schering Korea, Seoul, Korea) into potential patients of parotid gland tumor.
Two oral and maxillofacial surgeons were trained by an oral and maxillofacial radiologist predicted the location of the parotid gland tumor by setting 4 anatomical landmarks on the axial view on the obtained CT image. If the two surgeons had different predictions, the opinion of the oral and maxillofacial radiology specialist was referred to. The predicted location was compared with the true location of the tumor based on the surgical chart and photos during operation.
CA is an arc with a radius of 8.5 mm, centered on the most posterior point of mandibular ramus.
FN line connects the lateral surface of the posterior belly of the digastric muscle with the lateral surface of the cortex of the ascending mandibular ramus.
In the CA analysis, the tumor was deemed to have reached deep lobe of the parotid gland even when part of it is in arc. In case of the FN line and U line, the tumor was regarded as being in the superficial lobe of the parotid gland if the entire or most of the tumor is outside of the standard line. Otherwise, it was deemed to be in the deep lobe. In the case of RV analysis, the tumor was regarded as being in the superficial lobe if RV is moved to the inside or the tumor is outside of RV.
The case resulting from the image analysis, the parotid gland was predicted to be in the superficial lobe, and the true location was in the superficial lobe of the parotid gland.
The case resulting from the image analysis, the parotid gland was predicted to be in the deep lobe, and the true location was in the deep lobe of the parotid gland.
(Note: the definition of specificity is "Tumor was predicted to be not located in the superficial lobe, and the true location was not located in the superficial lobe of the parotid gland," but we defined it as above because the purpose of this research was to determine the method of operation such as superficial parotidectomy or total parotidectomy by predicting the location of the parotid gland tumor before the operation.)
The case resulting from the image analysis, the tumor was predicted to be in the superficial lobe when the true location was in the superficial lobe of the parotid gland.
Among 4 anatomical landmarks, the FN line had the highest value in terms of sensitivity for tumor in the superficial lobe of the parotid gland (81.8%), specificity (100%), positive predictive value (100%), and negative predictive value (71.4%). It also had the highest value in terms of efficiency (87.5%).
Among other anatomical landmarks, U line revealed high values in efficiency (81.3%) and positive predictive value (100%) but lower values than the FN line in sensitivity (72.7%) and specificity (40%). The sensitivity of RV was the same as that of the FN line (81.8%), but it had lower values than the FN line in all other values such as efficiency (68.8%), specificity (40%), positive predictive value (75%), and negative predictive value (50%). CA revealed the lowest values except specificity (60%), such as efficiency (50%), sensitivity (45.5%), positive predictive value (71.4%), and negative predictive value (33.3%).(Table 2)
Previous research commented many predicting methods, such as CA, FN line, U line, and RV, to identify the location of the parotid gland tumor before operation using imaging equipment such as CT or MRI and predicted the relationship between the location of the tumor and FN2,9-11.
When identifying tumor location using CT or MRI image, the FN branch in the CT image cannot detect even with contrast media. According to Thibault et al.13, however, it is possible to see the FN branch and part of the parotid gland tissue by lowering the intensity of MRI's T1 image and using a curvilinear view. However, the FN branch is not expressed in all MRI images, and it is impossible to examine the parotid gland due to shadow if there is metal prosthesis in the mouth. In contrast, MRI is advantageous in diagnosing soft tissue mass, but CT using contrast can identify the relationship between the location of the tumor and surrounding tissues14-16. We have diagnosed patients with parotid gland tumor using CT with contrast media due to its various advantages such as low inspection expenses.
In this research, CT with contrast was used; MRI was used additionally for a patient diagnosed with a malignant tumor as a result of the biopsy before operation (patient 12) to identify the relationship between the location of the tumor and surrounding tissues more correctly. With the CT image, anatomical landmarks were obtained based on the mandibular ramus (CA, FN line), posterior belly of the digastric muscle (FN line), ipsilateral half of the vertebra (U line), and RV (U line). For the posterior belly of the digastric muscle that is not distinguished clearly in the CT axial view, anatomical landmark was obtained at the location of the tumor by coming down along the line of the digastric muscle (inside surface of the mastoid bonemiddle tendon of hyoid). For 3 patients who had different opinions on the location of the posterior belly of the digastric muscle on the CT image between oral and maxillofacial surgeons (patient 3, 5, 6), the opinion of the oral and maxillofacial radiologist was consulted to; in both anatomical landmarks obtained by 2 inspectors, however, the tumor was predicted to be in the superficial lobe of the parotid gland. For the patient whose MRI was taken additionally, the location of the posterior belly of the digastric muscle as predicted in the CT image was the same as the predicted location in the MRI image.
In this research, when calculating sensitivity, specificity, positive predictive value, and negative predictive value, positive assumed that the tumor is in the superficial lobe of the parotid gland; negative assumed that it is in the deep lobe1. Therefore, high sensitivity means that the method has high accuracy in the case actual parotid gland tumor is in the superficial lobe, and the high specificity means that the method can accurately predict the tumor in the deep lobe of the parotid gland. A positive predictive value means the possibility that the ture location is in the superficial lobe of the parotid gland when the tumor is predicted to be in the superficial lobe of the parotid gland, whereas a negative predictive value means the possibility that the true location of tumor is in the deep lobe of the parotid gland when the tumor is predicted to be in the deep lobe of the parotid gland. For example, in this research, RV had high sensitivity (83.3%) but low specificity (40%). It can be interpreted to mean that the RV method is effective if a parotid gland tumor is in the superficial lobe but less reliable if the tumor is in the deep lobe. In the actual application of the RV method, a low negative predictive value (50%) was recorded. This means that the RV method is ineffective in predicting the location of the tumor in the deep lobe.
In the previous study of Lim et al.1, the U line method was the most accurate method with high sensitivity (89.3%), specificity (97.7%), positive predictive value (98%), negative predictive value (87.8%), and accuracy (94%). In this study, however, the most effective method in all standards was FN line with efficiency of 87.5%, sensitivity of 81.8%, specificity of 100%, positive predictive value of 100%, and negative predictive value of 71.4%. The U line (76.5%) had lower efficiency than the FN line. This can be attributed to the difference of perspectives in determining the location of muscle caused by the obscure image of digastric muscle in CT1. On the other hand, Ariyoshi and Shimahara11 analyzed the location of the parotid gland tumor using the FN line based on the MRI of dead bodies and achieved 87.5% accuracy. It means muscle layers are distingioshed more clearly in MRI, so the analysis of the tumor's location will be more efficient if MRI is used in preoperative diagnosis.
As shown in this research, the results of 4 analysis methods are different1,8-11,16, possibly because of the relationship between the anatomical landmarks of each method and the parotid gland. Among the 4 anatomical landmarks, RV and U line may be changed by location, size, and growth direction of the tumor because its anatomical landmarks for prediction (RV, vertebra) are on the lateral surface of the parotid gland17. However, the location of the FN line is not changed considerably by the location of the tumor because its references (posterior belly of digastric muscle, ramus) are either outside of the parotid gland or fixed1,2. In this research, RV and U line had low specificity. The reason is, if a tumor is in the superficial lobe of the parotid gland, it is easy to examine due to the great variation of tissue because the RV is outside the parotid gland; if a tumor is in the deep lobe of the parotid gland, however, the variation of the RV is less because internal tissues such as the posterior belly of the digastric muscle, isthmic fat layer, and internal carotid artery show more variation than the lateral surface of the parotid gland18. A parotid gland tumor moves the parotid gland due to its location in the parotid gland, size, or surrounding soft tissues. Therefore, if the reference is a fixed tissue outside of the parotid gland, the analysis of the location of the parotid gland becomes less effective because the anatomical landmark is not changed by tumor growth and location. And the standard line of CA (ramus) is always fixed, so it is not changed by the location of the parotid gland tumor. As shown in this research, prediction by the CA method that was not affected by the location of the tumor had the lowest efficiency; other methods had relatively higher prediction efficiency. In addition, among the analysis methods whose standard line is affected, the FN line using digastric muscle and the ascending ramus of mandible had the highest prediction efficiency.
In short, accuracy of a prediction is relatively lower if the anatomical landmark for analysis is changed greatly by the location of the tumor because of excessive proximity (RV); even when using a fixed anatomical landmarks (CA), it is hard to follow relative change according to the development of tumor. Therefore, the FN line analysis method with a fixed anatomical tissue (lateral surface of the ascending ramus of mandible) and a relatively movable standard line (lateral surface of the posterior belly of the digastric muscle) is effective in identifying the location of the parotid gland tumor before operation.
After analyzing the location of the parotid gland tumor before operation using CA, FN line, U line, and RV and comparing with the true location of tumor, the FN line was found to be the most reliable analysis method. However, additional image such as MRI may be helpful because the posterior belly of the digastric muscle is not always distinguished in CT when using the FN line method.
Figures and Tables
Fig. 1
Comparing with the Conn's arc (CA) (A), facial nerve (FN) line (B), Utrecht (U) line (C), and retromandibular vein (RV) (D) on the same computed tomography image. Clinical photo in operation room (E). CA, FN line, and RV predict that the tumor is in the superficial lobe. However, the U line predicted that the tumor is in the deep lobe. Compared with the clinical photo, the tumor was confirmed to be in the superficial lobe. The tumors and posterior belly of the digastric muscles are denoted by the dashed line.

References
1. Lim CY, Chang HS, Nam KH, Chung WY, Park CS. Preoperative prediction of the location of parotid gland tumors using anatomical landmarks. World J Surg. 2008. 32:2200–2203.

2. de Ru JA, van Benthem PP, Hordijk GJ. The location of parotid gland tumors in relation to the facial nerve on magnetic resonance images and computed tomography scans. J Oral Maxillofac Surg. 2002. 60:992–994.

3. DelBalso AM, Ellis GE, Hartman KS, Langlais RP. Del Balso AM, editor. Diagnostic imaging of the salivary glands and periglandular regions. Maxillofacial imaging. 1990. Philadelphia: WB Saunders;87–93.
4. Smith JR, King WW, Tang WY, Metreweli C. Differentiating tumours of the deep and superficial lobes of the parotid gland by computed tomographic sialography. Clin Radiol. 1987. 38:345–349.

6. Rice DH, Mancuso AA, Hanafee WN. Computerized tomography with simultaneous sialography in evaluating parotid tumors. Arch Otolaryngol. 1980. 106:472–473.

7. Sone S, Higashihara T, Morimoto S, Ikezoe J, Nakatsukasa M, Arisawa J, et al. CT of parotid tumors. AJNR Am J Neuroradiol. 1982. 3:143–147.
8. Wittich GR, Scheible WF, Hajek PC. Ultrasonography of the salivary glands. Radiol Clin North Am. 1985. 23:29–37.
9. de Ru JA, Bleys RL, van Benthem PP, Hordijk GJ. Preoperative determination of the location of parotid gland tumors by analysis of the position of the facial nerve. J Oral Maxillofac Surg. 2001. 59:525–528.

10. Conn IG, Wiesenfeld D, Ferguson MM. The anatomy of the facial nerve in relation to CT/sialography of the parotid gland. Br J Radiol. 1983. 56:901–905.

11. Ariyoshi Y, Shimahara M. Determining whether a parotid tumor is in the superficial or deep lobe using magnetic resonance imaging. J Oral Maxillofac Surg. 1998. 56:23–26.

12. Kurabayashi T, Ida M, Ohbayashi N, Ishii J, Sasaki T. Criteria for differentiating superficial from deep lobe tumours of the parotid gland by computed tomography. Dentomaxillofac Radiol. 1993. 22:81–85.

13. Thibault F, Halimi P, Bely N, Chevallier JM, Bonfils P, Lellouch-Tubiana A, et al. Internal architecture of the parotid gland at MR imaging: facial nerve or ductal system? Radiology. 1993. 188:701–704.

14. Teresi LM, Lufkin RB, Wortham DG, Abemayor E, Hanafee WN. Parotid masses: MR imaging. Radiology. 1987. 163:405–409.

15. Tabor EK, Curtin HD. MR of the salivary glands. Radiol Clin North Am. 1989. 27:379–392.
16. Ragbir M, Dunaway DJ, Chippindale AJ, Latimer J, Mohammed F, McLean NR. Prediction of the position of the intraparotid portion of the facial nerve on MRI and CT. Br J Plast Surg. 2002. 55:376–379.

17. Agur AMR, Lee MJ. Grant's atlass of anatomy. 1999. 10th ed. Philadelphia: Lippincott W&W.
18. Charles WC, John MF, Lee AH, Carles JK, David ES. Otolaryngology-head and neck surgery. 1986. St. Louis: C.V Mosby.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download