Abstract
Objectives
Stress may have an impact on treatment types that patients receive for temporomandibular disorders (TMDs). This study sought to investigate the relationship between the stress index and type of treatments in patients with TMD.
Materials and Methods
The psychosocial well-being index-short form (PWI-SF) was used to evaluate stress levels in ninety-two patients with TMD. Treatment types were classified into two groups: one group received counseling, physical therapy or medication, while the second group received splint therapy or surgical intervention.
The increase of emotional stress may be a factor in the occurrence, progress, and treatment of a temporomandibular disorders (TMDs) since it causes the rise of tension in the head and neck muscles, decline of physiological tolerance of noxious stimuli, and persistence of adverse muscle activities including clenching and bruxism1,2. Acute and chronic stress is known to cause and exacerbate depression3 which is considered to be worsened by negative stress incidents such as death of a loved one, divorce, and unemployment even further4,5. Therefore, emotional stress may be a crucial clinical factor in the assessment and treatment of TMD patients since it contributes to the occurrence and aggravation of various psychiatric disorders such as depression and TMD2. Due to the patient's lack of understanding and cooperation, however, it is difficult to conduct the Axis II test6 which provides the criteria for diagnosing the psychosocial conditions for the Research Diagnostic Criteria for TMD presented as a methodology for studies on TMD and to require the collaboration with the psychiatric department based on the test result. This study sought to explain the TMD more clearly to the patient and approach to the TMD of a patient visiting a dental clinic with depression, anxiety, and emotional stress. A simple survey on emotional stress was used to identify the relationship between emotional stress and TMD and was made as simple as possible.
It was assumed that if emotional stress affected the occurrence, progress, and treatment of the TMD; logically, the varying stress levels called for different types of treatments. To confirm this assumption, TMD patients visiting our dental clinic for the first time were assessed in terms of their level of emotional stress with the help of the psychosocial well-being index-short form (PWI-SF)7 as a stress-measuring instru ment. The patients were allocated to a group receiving coun seling, self-physiotherapy, or medication and to another group treated with splint or surgical procedures and then studied retrospectively in connection with the initial stress indices and relationship with treatment types.
Ninety two patients are included in this study out of the 169 patients who had visited Gangnam Severance Hospital and Yongin Severance Hospital for TMD, agreed to a survey, and completed the survey. This study excluded patients who needed to make no more appointments at first visit because of their slight disease status and was instructed self-care and/or medication or whose medical records were not fully completed.
During the first visit, the TMD patients' stress levels were assessed based on the PWI-SF form, a stress questionnaire adapted to Korea7 with proven feasibility in selecting groups for the treatment of psychiatric disorders such as depression and anxiety disorder. The 18 questions in the PWI-SF form can be answered and are scored with 0, 1, 2, or 3 points; the higher the points, the more severe the stress level. As suggested by the developer of PWI-SF7, the subjects of this study were divided into the healthy group with less than 8 points, potential stress group with 9-26 points, and high-risk group with 27 points or higher. In this study, the authors divided two groups; low- and high risk group. Low-risk group was set with 26 points or less since there was 1 subject in the healthy group. The type of treatment given to each patient were divided into two groups. The treatment type of one group was one of counseling, self-care and self-physiotherapy (mandibular exercise, trigger point massage, moist heat pack, etc.), and medication. The treatment type of another group was one of splint therapy or arthroplasty of temporomandibular joint. If a patient has received 2 or more types of treatment, counseling, self-care and self-physiotherapy, medication, splint therapy, and surgical treatment were prioritized (e.g., surgical treatment has higher priority than medication) and were compared with stress levels. The gender groups and 3 age groups (10-20s, 30-40s, and 50-60s) were analyzed with PWI-SF results, stress groups, and treatment type distribution.
An independent sample t-test was conducted to see if different gender groups had different PWI-SF points. A chi-square test was done to identify the difference in stress and treatment types in different gender groups and 3 age groups (10-20s, 30-40s, and 50-60s). The difference in PWI-SF points in varying age groups were verified by one-way ANOVA. Multiple logistic regression was performed to identify the effect of each of gender, age, and stress level on the treatment type. The level of significance was set at 0.05, and PASW 18.0 (IBM Co., Armonk, NY, USA) was used for statistical analysis.
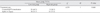
Of the 92 subjects of this study, 22 were male (23.9%) and 70 were female (76.1%), i.e., there were 3 times more women than men, and their average age was 29.5±11.7. In terms of the frequency distribution of the stress group based on their stress levels, the low-risk group (1 subject in the healthy group, 57 subjects in the potential stress group) had 58 subjects (63.0%), whereas the high-risk group had 34 subjects (37.0%). Among the subjects, the mean stress levels of males and females were 19.45±9.57 and 25.30±7.38 each, indicating that women's stress level was significantly higher than that of men (P=0.003).(Table 1) A frequency difference analysis of the low- and high-risk groups by gender did not reveal a significant difference (χ2=2.513, P=0.113).(Table 1) No significant difference was observed in the comparison of the mean stress level and stress group distribution (low-risk and high-risk groups) based on age groups (10-20s, 30-40s, and 50-60s; mean stress level: F=0.071, P=0.931; stress group: χ2=0.095, P=0.954).
The distribution of varying treatment types showed that more subjects preferred splint or surgical treatment to counseling, self-physiotherapy, or medication. More specifically, 55 subjects (59.8%) chose the former, whereas 37 (40.2%) chose the latter. Distribution of the treatment type depending on the gender and age group was not significant (gender group: χ2=1.151, P=0.283; age group: χ2=0.608, P=0.738).
In the low-risk group, 28 of the 58 subjects (48.3%) were treated by counseling, self-physiotherapy, and medication, and 30 (51.7%) received splint therapy or surgical treatment (1 subject). In other words, both types of treatment were used almost equally. In the high-risk group, 9 of 34 subjects (26.5%) used counseling, self-physiotherapy, and medication, whereas 25 (73.5%) received splint and surgical treatment (2 subject). This suggested that the latter type of treatment was preferred.(Table 2) The treatment types (counseling, self-physiotherapy, and/or medication and splint or surgical treatment) used by varying stress groups were analyzed by chi-square test, which showed that the high-risk group significantly preferred splint and surgical treatment more than the low-risk group (χ2=4.239, P=0.040).(Table 2) Multiple logistic regression was performed to consider the gender, age, and stress groups and their effect on the treatment types selected.(Table 3) The result showed that gender and age did not wield a significant influence, and that the stress groups did not show a statistically significant difference, but the high-risk group preferred splint and surgical treatment than the low-risk group (gender: P=0.388; age: P=0.227; stress level: P=0.070).
TMD is a generic term referring to the dysfunction of the masticatory system including muscles and skeleton and is reportedly caused by malocclusion, emotional stress, trauma, introduction of heart pain, and abnormal function activity, among others8-10. Psychiatric factors, e.g., emotional stress, anxiety, and depression, may cause general functional disorders and TMD. Increase of emotional stress level intensifies the head and neck muscle tension and lowers the patient's physiological tolerance to noxious stimuli1. In addition, increased emotional stress may cause adverse muscle activities including clenching and bruxism to persist. Anxiety may also contribute to TMD as reported by Fricton et al.11, i.e., 26% of the 164 TMD patients displayed a clinically clear anxiety syndrome. Gerschman et al.12, also reported that 17% of TMD patients suffered serious anxiety. Such anxiety may be the result of the pain and result in the dropping of the threshold of the patient's pain level10,13. According to Manfredini et al.14, among TMD patients, the group of patients with facial muscle pain compared to the group suffering no pain had a higher prevalence rate of psychiatric syndromes including depression and panic disorder. Such study results suggest that some of the TMD patients also suffer from anxiety disorder.
Depression may also lower the pain threshold of TMD patients13. According to studies reporting a direct relationship between depression and physical symptoms15,16, more than half of the depression patients experienced prominently evident physical symptoms including fatigue and general muscle pain, which were purely physical. As indicated by a multinational report by World Health Organization (WHO)17, 69% of depression patients were initially treated for physical symptoms only. Depression was also more common among patients suffering from physical symptoms18, and there was a direct quantitative relationship between the number of physical symptoms suffered and occurrence rate of depression19. Gerschman et al.12, also reported that 18% of the 368 TMD patients suffered from severe depression. Therefore, the pain threshold for many TMD patients may likely be lowered as well by concomitant depression.
TMD is observed to be related closely to stress; therefore, the stress level should be assessed when treating patients with these disorders. Speculand et al.20, studied the occurrences of stress for 6 months prior to the manifestation of TMD in 85 patients and a control group with the same number of subjects. The patient group suffered from twice as many as the occurrences of stress from day-to-day life compared to the control group. Kanehira et al.2, studied the relationship between stress and TMD based on a survey. Cracking jaw, pain, and mouth opening limitation as the 3 major symptoms of this disorder along with undesirable habits such as clenching and bruxism were also significantly related with stress. Nifosì et al.21, assessed the stress level of the TMD patients with masticatory muscle disorders and only with temporomandibular joint disorders, with the former found to have higher level of stress. This study revealed that women suffered significantly higher mean stress level than men. Although the result may vary depending on the sociocultural background of the subjects or method of research, women were shown to have twice as high depression than men22; four times as many women than men were also known to suffer from anxiety disorders such as panic disorder23. Although this study did not include diagnostic interviews with subjects, PWI-SF has already been proven to be feasible in selecting groups for studies in depression, anxiety, and other psychiatric disorders7,24. Therefore, this study's result shows that women may be more susceptible to emotional stress among TMD patients as in the case of other general demographic groups.
The PWI-SF form is an abbreviated form with 18 questions of General Health Questionnaire (GHQ)-60 PWI and 45 questions to suit Koreans. Developed more to measure the stress level of normal people than to diagnose psychiatric issues, this tool assigns 0, 1, 2, or 3 points to each item based on the 4-point Likert scale with "Always", "Almost always", "Sometimes", and "Never". Points given to each item are added up, with the subjects garnering 8 points or less categorized as the healthy group, those with 9-26 points as potential stress group, and those with 27 points or more as high-risk stress group. The healthy, potential stress, and high-risk groups were found to account for 19.4%, 61.3%, and 19.3%, respectively, among the general working population. In this study, almost none of the subjects belonged to the healthy group. Thus, the healthy group and potential stress group were combined and named low-risk group. Only 1 belonged to the healthy group, and this subject had received splint therapy for masticatory muscle disorders and temporomandibular joint disorders. Since the developer of PWI-SF noted that 19.4% of the general working population belonged to the healthy group7, the fact that the healthy group in this study on TMD patients may be far smaller should be considered.
In this study, 37% of all subjects belonged to the high-risk stress group. This percentage is much higher than 19.3% of the general working population as noted by the developer of PWI-SF, indicating that TMD patients are likely to suffer from concomitant emotional stress. The 2 types of treatment considered in this study were counseling/self-physiotherapy/medication and splint therapy/surgical treatment. Patients who have long suffered from jaw or masticatory muscle pain or mouth opening limitation along with jaw or masticatory muscle pain or those who had not responded to prior treatment chose the latter. Counseling included helping patients develop awareness of and understand the cause and condition of the disorder and guiding the patients to avoid undesirable habits such as resting the chin on one hand, sleeping on one's stomach, and excessive chewing habit. On the other hand, self-physiotherapy included lower jaw exercise, painful spot massage, moist heat pack, etc., which could be done anywhere outside of the clinic facilities or easily using a simple instrument at home; medication included the use of muscle relaxant and anti-inflammatory pain killer and - depending on the condition of the patient - anti-depressant and minor tranquilizer. Splint therapy included the use of occlusal stabilizing splint or anterior positioning appliance, whereas surgical treatment included open joint surgeries such as articular disc repositioning or removal, eminoplasty, and condyloplasty, one of which can be selected depending on the condition of the patients. Multiple methods were used on the subjects of this study25. Patients with chronic and minor TMD were asked to use counseling, self-physiotherapy, and medication, whereas those who suffered from a severe condition or who had not responded to self-physiotherapy or medication were directed to use splint or surgical treatment methods. Considering the fact that only 1 patient underwent surgery among all subjects, we can conclude that the high-risk group is more likely to use splint therapy. Therefore, if a patient is found to belong to the high-risk group upon the first visit, splint therapy may be considered. According to Gerrits et al.26, depression or anxiety disorder patients suffering from pain were more likely to suffer chronically. Though this study did not include professional diagnostic interviews, as mentioned earlier, a majority of patients in the high-risk group are likely to suffer concomitant depression or anxiety disorders. Moreover, concomitant depression and anxiety disorders may lower the pain threshold, aggravate, and make chronic the symptoms of TMD13, as a result of which additional splint or surgical treatment may be provided. Therefore, in future studies, it may be necessary to use not only PWI-SF but also the Beck Depression Inventory (BDI)27 or Beck Anxiety Inventory (BAI)28 which is self reporting instrument for depression and anxiety disorder, among other clinical scales and diagnostic interviews for psychiatric conditions in order to identify concomitant psychiatric conditions. The existence of concomitant depression or anxiety disorders should be accurately assessed; if they do exist, they should be adequately understood by the patients concerned so that collaboration with the psychiatric department is enabled at the right time for professional treatment.
This study had the following limitations: 1) difficulty in analyzing the relationship between masticatory muscle disorders or joint disorders with stress since most patients visiting the study institution suffered from joint disorders, not other types of disorders; 2) difficulty in accurately concluding whether TMD actually involved depression and anxiety disorders among other psychiatric conditions since only the stress level was measured by PWI-SF without using clinical scales such as BDI or BAI or psychiatric diagnostic interviews; 3) lack of research on socioeconomic or educational backgrounds - except gender and age - among other demographic and social factors that may affect the selection of treatment types; 4) lack of diversity of subjects since they were only divided into low-risk and high-risk groups regardless of stress levels, and treatment types only included counseling-self-physiotherapy-medication or splint-surgical treatment, and; 5) possibility that the TMD patients included in the study were only those who had visited a certain clinic in a defined area and might have suffered from actually more severe condition or concomitant psychiatric issues, thereby making it impossible to generalize the result of this study. The socio-demographic factors and psychiatric diagnosis procedure are expected to be considered comprehensively with more patients in future studies to enable understanding of the relationship between TMD and emotional stress as well as concomitant psychiatric disorders.
In the TMD patient group under more emotional stress, splint therapy or surgical treatment was preferred to counseling, self-physiotherapy, and/or medication; thus showing that more emotional stress likely led to more severe symptoms and chronic development of the condition. In addition, women were found more likely to experience greater emotional stress and concomitant psychiatric disorders; thus suggesting the need to consider gender and emotional stress in the clinical assessment and treatment of TMD patients. In conclusion, considering psychiatric factors such as stress will be helpful in determining the overall treatment plan for TMD patients visiting the clinic, since emotional stress may be a crucial factor in the selection of method for treating TMD. The high-risk stress group is highly likely to have concomitant psychiatric disorders, which requires appropriate measures including counseling, medication, and collaboration with the psychiatric department.
Figures and Tables
Table 1
Comparison of the mean PWI-SF score and proportions of the stress group and treatment type between male and female TMD patient groups

References
1. Larsman P, Kadefors R, Sandsjö L. Psychosocial work conditions, perceived stress, perceived muscular tension, and neck/shoulder symptoms among medical secretaries. Int Arch Occup Environ Health. 2012. 02. 12. [Epub ahead of print].

2. Kanehira H, Agariguchi A, Kato H, Yoshimine S, Inoue H. Association between stress and temporomandibular disorder. Nihon Hotetsu Shika Gakkai Zasshi. 2008. 52:375–380.

3. Brown J, Cooper-kuhn CM, Kempermann G, Van PH, Winkler J, Gage FH, et al. Enriched environment and physical activity stimulate hippocampal but not olfactory bulb neurogenesis. Eur J Neurosci. 2003. 17:2042–2046.

4. Aneshensel CS, Stone JD. Stress and depression: a test of the buffering model of social support. Arch Gen Psychiatry. 1982. 39:1392–1396.
5. Phifer JF, Murrell SA. Etiologic factors in the onset of depressive symptoms in older adults. J Abnorm Psychol. 1986. 95:282–291.

6. Dworkin SF, Leresche L. Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J Craniomandib Disord. 1992. 6:301–355.
7. Chang SJ. The Korean Society for Preventive Medicine. Stress. Standardization of collection and measurement of health statistics data. 2000. Seoul: GyeChukMunWhaSa Publishing Co.;92–143.
8. Yoo JH, Kang SH, Baek SH, You TM, Kim JB. Effect on explanation of pathogenesis and stress management as primary care of TMJ disorder. J Korean Assoc Oral Maxillofac Surg. 2002. 28:358–363.
9. Okeson JP. Management of temporomandibular disorders and occlusion. 2009. 6th ed. Seoul: Narae Publishing.
10. Rugh JD, Woods BJ, Dahlström L. Temporomandibular disorders: assessment of psychological factors. Adv Dent Res. 1993. 7:127–136.

11. Fricton JR, Kroening R, Haley D, Siegert R. Myofascial pain syndrome of the head and neck: a review of clinical characteristics of 164 patients. Oral Surg Oral Med Oral Pathol. 1985. 60:615–623.

12. Gerschman JA, Wright JL, Hall WD, Reade PC, Burrows GD, Holwill BJ. Comparisons of psychological and social factors in patients with chronic orofacial pain and dental phobic disorders. Aust Dent J. 1987. 32:331–335.

13. Cimmino MA, Ferrone C, Cutolo M. Epidemiology of chronic musculoskeletal pain. Best Pract Res Clin Rheumatol. 2011. 25:173–183.

14. Manfredini D, Bandettini DPA, Cantini E, Dell'osso L, Bosco M. Mood and anxiety psychopathology and temporomandibular disorder: a spectrum approach. J Oral Rehabil. 2004. 31:933–940.

15. Tylee A, Gastpar M, Lépine JP, Mendlewicz J. DEPRES II (Depression Research in European Society II): a patient survey of the symptoms, disability and current management of depression in the community. DEPRES Steering Committee. Int Clin Psychopharmacol. 1999. 14:139–151.

16. Simon GE, VonKorff M, Piccinelli M, Fullerton C, Ormel J. An international study of the relation between somatic symptoms and depression. N Engl J Med. 1999. 341:1329–1335.

17. Akechi T, Nakano T, Akizuki N, Okamura M, Sakuma K, Nakanishi T, et al. Somatic symptoms for diagnosing major depression in cancer patients. Psychosomatics. 2003. 44:244–248.

18. Terre L, Poston WS, Foreyt J, St JS. Do somatic complaints predict subsequent symptoms of depression? Psychother Psychosom. 2003. 72:261–267.

19. Nakao MYE. Reporting of somatic symptoms as a screening marker for detecting major depression in a population of Japanese white-collar workers. J Clin Epidemiol. 2003. 56:1021–1026.

20. Speculand B, Hughes AO, Goss AN. Role of recent stressful life events experience in the onset of TMJ dysfunction pain. Community Dent Oral Epidemiol. 1984. 12:197–202.

21. Nifosì F, Violato E, Pavan C, Sifari L, Novello G, Guarda Nardini L, et al. Psychopathology and clinical features in an Italian sample of patients with myofascial and temporomandibular joint pain: preliminary data. Int J Psychiatry Med. 2007. 37:283–300.

22. Ministry of Health and Welfare. The epidemiological survey of psychiatric illness in Korea 2006. 2008. Seoul: Ministry of Health and Welfare.
23. Joyce PR, Bushnell JA, Oakley-browne MA, Wells JE, Hornblow AR. The epidemiology of panic symptomatology and agoraphobic avoidance. Compr Psychiatry. 1989. 30:303–312.

24. Lee SY, Jeong SH, Lee CY, Choi KS. The approach to mass screening of psychiatric patients using psychosocial well-being index (PWI). J Korean Soc Biol Ther Psychiatry. 1997. 3:175–184.
25. Cha YH, Kim BJ, Lim JH, Park KH, Kim HG, Huh JK. Analysis of treatment patterns of temporomandibular disorders. J Korean Assoc Oral Maxillofac Surg. 2010. 36:520–527.

26. Gerrits MM, Vogelzangs N, van Oppen P, van Marwijk HW, van der Horst H, Penninx BW. Impact of pain on the course of depressive and anxiety disorders. Pain. 2012. 153:429–436.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download