IV. Discussion
Classification of the timing of open bite recognition is correlated with the etiological factors of open bite. Note, however, that this investigation was performed within the category of patients with TMD; therefore classification of the timing of open bite recognition should not to be regarded straight ahead as the classification of causative factors. This investigation was intended for better understanding of process of an open bite occurrence. Firstly, the patient group that anterior open bite was observed at initial examination regardless of patient's recognition formed relatively large portion of 32.7% (17 patients). This patient group can be explained in two aspects as muscular factors and condylar resorption. First, there were patients showing only joint space narrowing together with an anterior open bite without any morphological change in their condylar heads in their panoramic radiographs and lateral tomograms. We think the excessive tension of the masticatory muscle serves as an excessively heavy load on the TMJ portion, resulting in the narrowing of the joint space and - instead of molar intrusion - the clockwise rotation of the mandible with the most posterior molar playing the role of the lever fulcrum, considered to induce an anterior open bite. Second, there were patients showing an obvious morphological change in their condylar heads in their radiographs. Most patients in this group showed the aspect of anterior open bite due to idiopathic or progressive condylar resorption. Arnett et al.
11,
12 presented two main causative factors of idiopathic or progressive condylar resorption-the continuous excessive physical stress on the TMJ portion and the decreased adapta bility of patients. One of the contributing elements for decreased host adaptability is the age of the patient. Age groups whose environmental adaptability decrease are group of twenties to thirties presenting progressive condylar resorption due to unknown reasons and groups of fifties to sixties presenting degenerative condylar changes
11. Accordingly, this patient distribution by age was corresponded with the distribution in our study. Though both idiopathic condylar resorption and degenerative arthritis show mechanism differences, these have similar process of morphological change of condyle - if severe physical stress is applied exceeding host adaptability to TMJ portion, morphological change occurs in the condylar head and in the glenoid fossa, thereby resulting in a decrease in the posterior mandibular vertical height. This shows decreased mandibular growth in a growing child and gives rises to an anterior open bite together with progressive mandibular retrusion in an adult
11,
13. Similarly, the patient group with retrognathic profile accounted for the largest proportion at 51.9% and there was no patient group with prognathic profile in this study.
In the classification of the timing of open bite recognition, 23 patients (44.2%) showed an open bite during or after splint therapy. The splint therapy was chosen as a conservative therapy to decrease the load on TMJ and reduce the hyperactivity of tense muscles. But an anterior open bite may occur as a side effect especially in a patient wearing the splint all day long or a patient wearing a partial coverage appliance. If a splint becomes worn as a result of long-time use or if it is not checked properly, an anterior open bite may occur due to the selectively excessive eruption of molar teeth
14. In addition, several research were reported that use of splint altered the masticatory muscle activity, so occlusal force were newly set up and vertical height got changed; thus resulting the positional change of mandible itself, not the movement of teeth, which leads to the occurrence of an anterior open bite
15,
16. Based on the results of this study, 9 patients (17.3%) had a history of having undergone splint therapy, but the time of open bite recognition did not match the time of wearing a splint. We think they are patients combined with two causative factors - anterior open bite after splint therapy or splint therapy during progression of idiopathic condylar resorption which may lead to anterior open bite.
In classification of the timing of open bite recognition, 4 patients (7.7%) showed an open bite after orthognathic surgery. The positional change of bone segments, which occurs during orthognathic surgery, gives rise to a compressive force being applied to the condylar head in the glenoid fossa; if it continues, it may give rise to TMJ pain and condylar resorption, thereby causing a delayed relapse in the mandible
12,
17,
18. In their evaluation of the long-term stability after orthognathic surgery, Hoppenreijs et al.
19 reported the frequent occurrence of progressive condylar resorption, especially in the case of mandibular advancement surgery through sagittal split ramus osteotomy. Condylar resorption after orthognathic surgery is aggravated by the muscular action of the masseter muscle and the medial pterygoid muscle; thus causing the mandible to be retruded posteriorly, which gives rise to an anterior open bite
12.
The existing treatment of anterior open bite that has been suggested so far are largely divided into orthodontic treatment and surgical treatment. In the 1980s to 1990s, open bite treatment through the extrusion of anterior teeth was mainly used as a kind of orthodontic treatment. Note, however, that the extrusion of anterior teeth leads to show poor profiles resulting from the clockwise rotation of the mandible. Also in the evaluation of long-term stability for 10 years by extrusion of anterior teeth, over 35% of the patients were said to show a relapse of more than 3 mm
20. Molar intrusion provides more efficient and more stable treatment results, and attempts have been made to use bite plates, springs, high pull headgears, fixed appliances, vertical elastics, and multiloop edgewise archwire (MEAW) for this. Nonetheless, it has been difficult to attain the required amount of molar intrusion
21-
23. Surgical treatment can solve the problem of anterior open bite mainly through superior repositioning of the maxilla and counterclockwise rotation of the mandible, however the evaluation of long term stability revealed that maxilla was mainly accompanied by vertical relapse. Approximately 10% of the patients who had underwent surgery showed a significant 2-4 mm relapse of anterior open bite
24. In the evaluation of the one-year post-operative stability by Oliveira and Bloomquist
25, the average rate of skeletal relapse was found to be 33.42%. In addition, there are several factors causing relapse - condylar resorption by a compressive force due to the movement of bone segments causes delayed relapse as mentioned above, an increase in the posterior facial height occurring during the counterclockwise rotation of the mandible may result in the elongation of the pterygomasseteric sling, and the mandibular symphysis moving away from the hyoid bone cause elongation of the suprahyoid muscle
2. On the other hand, orthodontic treatment using SAS can attain relatively easily the required amount of molar intrusion, which has been difficult using the existing orthodontic treatment means and have shown comparable treatment effect with the effect of surgical treatment in the post-treatment cephalometric analysis
4. As in the case of a relatively low relapse rate of 10.36% in orthodontic treatment using SAS as reported by Lee and Park
21, orthodontic treatment using SAS has merits in terms of stability after treatment since it provides time for the slow adaptation of muscles compared with surgical treatment.
Since malocclusion is related to the malposition of the mandibular condyle in the glenoid fossa, it is an important causative factor of TMD
26,
27. As one can see in the epidemiological study conducted by Egermark et al.
28 and Henrikson et al.
29, anterior open bite is closely related to TMD among other kinds of malo cclusion. Therefore, special consideration for those patients with TMD and anterior open bite patients has become acutely required. Regarding this in the case of surgical treatment, Aghabeigi et al.
30 reported that orthognathic surgery was not effective for anterior open bite patients with TMD but was found to lead to condylar resorption. Though, orthodontic treatment using SAS makes molar intrusion effectively and has several merits - normalization of condylar position in glenoid fossa by counterclockwise rotation of mandible, having enough time for muscle adaptation to newly position
31,
32, there was also a case wherein a decrease in the posterior facial height rather increased loading on condyle; thus triggering condylar resorption.
Besides surgical treatment and orthodontic treatment of patients with anterior open bite and TMD, attempts have been made to reduce the compressive force on TMJ portion to prevent the progress of condylar resorption, which may lead to an anterior open bite. For this, intermaxillary traction by button attachment at buccal crown of premolars had been tried, but has side effects of extrusion of button attached-premolars. Intermaxillary traction by Pivot splint had also been tried, but it was hard to reduce the loading in joint space and has limitation to resolve anterior open bite
14,
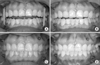
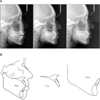
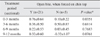
33. In this study, we applied the treatment of intermaxillary traction using SAS, and evaluated symptom changes related to TMJ and improvement amount of anterior open bite. Before starting treatment, we took an impression and made the study model of upper and lower dentition of each patient, then we investigated whether maximum intercuspitation could be induced on study model or not, and compared the occlusion between study model and actual occlusion of patients. One of the aspects differentiating treatment by intermaxillary traction from the existing orthodontic treatment methods is the fact that it has obtained treatment effects only by elastic traction after mini-screw placement instead of using bracket or wire orthodontically. The other differentiating point is the placement area of mini-screws which is placed on molar area for molar intrusion orthodontically, but placed on premolar area for intermaxillary traction used in this study. If there are some cases that obvious premature contact of premolars on study model exist, we applied intermaxillary traction using SAS first for relieve TMJ symptom and improve anterior open bite, then referred to orthodontist to eliminate premature contact ; these cases were excluded for this study. As a result of treatment, molar intrusion led to improve patient's profile of retruded chin through closure of anterior open bite. Therefore, B point (most posterior point on the bony curve between infradentale and pogonion) moved forward and the value of ANB (angle formed by A point, nasion, and B point) became improved.(
Fig. 5) There was a decrease in the mandibular plane angle and a decrease in the anterior facial height due to the counterclockwise rotation of the mandible, thereby easing the tension of muscles around the lips. An increase in the joint space may also be expected due to the counterclockwise rotation of the mandible, but it was difficult to measure joint space change in lateral cephalometrics. From the result of tracing the lateral cephalometrics, both molar intrusion and mild extrusion of anterior teeth were occurred together by existing orthodontic approach, but the treatment effect was appeared mainly by molar intrusion rather than anterior teeth extrusion by intermaxillary traction using SAS in this study. In the case of patients with a large amount of anterior open bite, the most posterior molars may play a role as lever fulcrum by condylar resorption on anterior-superior surface, thereby the most posterior molars come to be compressed by bite force continuously. If intermaxillary traction treatment applied in these patients, additional longer retention period is required after closure of anterior open bite to expect occlusal seating of the most posterior molars. (
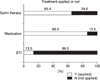
Fig. 5) As a result of treatment by intermaxillary traction, the final amount of anterior open bite improvement was found to be 1.75±1.33 mm on average, and it took 6 months of treatment period to achieve open bite improvement of about 1 mm. Adjunctive treatment for muscle relaxation was applied to patients before or during intermaxillary traction treatment. The adjunctive treatment was performed not only to relieve muscle pain and relax the tense muscles, but also to have expectation for maintaining the treatment effects after treatment finished by giving muscles enough time to adapt to changed skeletal position. In other words, repositioning of the condylar head, easing the tension of surrounding muscles, and physiological adaptation through intermaxillary traction are important elements for solving the symptoms of TMD. For this purpose, we used medication treatment, physical treatment, injection of botulinum toxin, and splint therapy
34. Muscle relaxants and non-steroidal anti-inflammatory drugs (NSAIDs) were mainly used for medication treatment. Muscle relaxants are known to control the convulsion and pain withdrawal reflex of the masticatory muscle
35. As for physical treatment, hot wet pack treatment and mandibular exercise treatment were used. Hot wet packs ease muscles and help perform exercise treatment under the condition of relieved pain. Exercise treatment was performed to build up the strength of muscles, prevent the contraction of joints, and maintain the range of functional jaw movement
36. Injection of botulinum toxin was carried out when reducing the contraction and strength of the masticatory muscle was additionally required. Splint therapy reduces the load on the TMJ and reduces the hyperactivity of muscles. In this study, anterior positioning splints were used for treatment with splint therapy. This splint make condyle to place on center or slightly anterior inferior portion of glenoid fossa, which was originally positioned at posterior superior portion of glenoid fossa by excessive action of jaw-closing muscles before treatment; so that it can reduce the load on condyle, reduce inflammation surrounding joint, increase range of mandibular movement, and relieve symptoms of TMD
37. When intermaxillary traction and splint therapy were performed in combination, in the initial stage, we had the patients wear elastics for intermaxillary traction during daytime and both elastics and anterior positioning splints when sleeping. When occlusion had become stable along with increasing overbite, and their TMJ symptoms had improved, we had them wear elastics without any splint only when sleeping.
The TMJ symptoms of the patients mostly improved after both intermaxillary traction for condylar repositioning and adjunctive treatment for muscle relaxation. In the evaluation of the treatment results, however, patients showing no change in their TMJ symptoms before and after treatment accounted for a large proportion, this can be interpreted in two ways. First, since they were anterior open bite patients accompanied with TMD, if treatment of their TMD was performed prior to treatment by intermaxillary traction, it could be written in medical record, immediately before traction treatment, that TMJ symptoms had been relieved; then there could be no change in TMJ symptoms before and after intermaxillary traction treatment. In other cases which there was no change in the TMJ symptoms, if TMD were related with sociopsychological factors or compounded with pain on other part of body, their TMD may have persisted or failed to respond to any accepted treatment.
We investigated the differences in the amount of open bite improvement according to whether or not anterior open bite was reduced by anterior superior force on chin top. If anterior open bite was not reduced by force on chin top, the causes may be considered in two ways. Firstly, in the lateral view of occlusal pattern, a wedge-shaped open bite from the incisor to the most posterior molar could be observed, just same as open bite pattern of 'reduced group' when forced on chin top. In this case, the amount of anterior open bite is not reduced by external force because of muscular factors - excessive strong strength of masticatory muscle or stiffened muscle. Second, in the view of occlusal pattern on study model, these are the cases that maximum intercuspitation had not been induced on study model. Patients who having had a bad habit such as finger sucking or tongue thrusting in their childhood or patients exhibiting stable occlusion state of anterior open bite by extruded premolar teeth were belonged to these group of occlusal pattern and excluded from the scope of this study. In the cumulative statistics by treatment period, 'reduced group' showed significantly greater amount of open bite improvement than 'not-reduced group' at periodic points of 3 months, 12 months, final treatment. In the sectional statistics by treatment period, which reflects improvement speed of anterior open bite, 'reduced group' exhibited significantly greater amount of open bite improvement than 'not reduced group' for up to 3 months from treatment initiation. In other words, 'reduced group' finally showed greater amount of open bite improvement than 'not reduced group', and about 37% of this improvement amount occurred for the first three months of intermaxillary traction treatment. The numerical figures from results above could be utilized to predict prognosis of treatment more easily for clinicians.
There were several limitations to perform this study. First, since this was a retrospective study, we had to exclude some patients, such as patients who did not have enough records to perform this study or patients who did not apply elastics regularly due to poor cooperation, therefore the number of study individuals was lower compared with the number of individuals who underwent the actual treatment. Second, we evaluated the open bites of the patients in relation to the symptoms of TMD. Since TMD were often related to the psychological factor of patients, and it was also difficult for evaluators to be objective, there were also limitations to perform study. Third, this study did not use a control patient group, such as patient group who underwent orthodontic treatment or surgical treatment; hence the difficulty in comparing the treatment results objectively. In existing literature, authors expressed difficulty in establishing a control group in the treatment of open bites. The authors who established a control group used it only to examine and ascertain the characteristics of the patients prior to treatment, but there were few cases wherein a control group was established in the true sense
21. To address this problem, we believe prospective studies need to be carried out on a great number of patients based in some objective criteria and indications to enable providing useful information for clinicians. For future research on advanced treatment by intermaxillary traction, studies should be performed with regard to the changes of the condylar position and joint space during treatment. Also, there is a need to conduct studies on long-term stability of intermaxillary traction treatment and how muscular adaptation actually has effect on treatment result.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download