Abstract
Objectives
This study evaluated a range of fixation methods to determine which is best for the postoperative stabilization of a mandibular osteotomy using three-dimensional finite element analysis of the stress distribution on the plate, screw and surrounding bone and displacement of the lower incisors.
Materials and Methods
The model was generated using the synthetic skull scan data, and the surface model was changed to a solid model using software. Bilateral sagittal split ramus osteotomy was performed using the program, and 8 different types of fixation methods were evaluated. A vertical load of 10 N was applied to the occlusal surface of the first molar.
Results
In the case of bicortical screws, von-Mises stress on the screws and screw hole and deflection of the lower central incisor were minimal in type 2 (inverted L pattern with 3 bicortical repositioning screws). In the case of plates, von-Mises stress was minimal in type 8 (fixation 5 mm above the inferior border of the mandible with 1 metal plate and 4 monocortical screws), and deflection of the lower central incisor was minimal in types 6 (fixation 5 mm below the superior border of the mandible with 1 metal plate and 4 monocortical screws) and 7 (fixation 12 mm below the superior border of the mandible with 1 metal plate and 4 monocortical screws).
Sagittal split ramus osteotomy (SSRO) was first reported by Trauner and Obwegeser in 1957 and modified by Dal Pont, Hunsuck, and Epker1. The SSRO technique has been modified continuously and widely used for the correction of mandibular disharmonies1,2. Nowadays, more stable results are possible thanks to the development of surgical techniques, instruments, and fixation methods. Note, however, that a number of fixation methods after osteotomy itself are currently being used. Therefore, accurate analysis of stress distribution and displacement according to the fixation methods is important. Generally, proximal and distal segments after SSRO are fixed with bicortical screws or metal plates and monocortical screws. Various studies on fixation materials and methods have been performed. Note, however, that studies on stress/strain of bone, metal plates, and screws according to number and position are rare3-5.
This study sought to evaluate the fixation methods after SSRO using three-dimensional finite element analysis (FEA) of stress distribution on the plate, screw, and surrounding bone and displacement of the lower incisors.
A mandibular surface model was created by three-dimensional (3D) scanning (Breuckmann Inc., Meersburg, Germany) of the mandible model (QS7/E, Somso modelle, Coburg, Germany). Rapidform software (INUS Technology Inc., Seoul, Korea) then converted the mandibular surface model into a 3D solid model. A commercially available computer-assisted design tool, CATIA (Dassalut System Inc., Paris, France), was used to simulate SSRO.
Group 1 was the bicortical screw-fixation group and was divided as follows (Fig. 1):
Type 1: One screw was fixed 5 mm posterior to the osteotomy line and 5 mm inferior to the superior border.
Type 2: The first screw was fixed 5 mm posterior to the osteotomy line and 5 mm inferior to the superior border. The second screw was fixed 7 mm posterior to the first screw and 5 mm inferior to the superior border. The third screw was fixed 5 mm posterior to the osteotomy line and 5 mm superior to the mandibular inferior border. Three screws were positioned in reverse L shape.
Type 3: The first screw was fixed 5 mm posterior to the osteotomy line and 5 mm inferior to the superior border. The second screw was fixed 7 mm posterior to the first screw and 5 mm inferior to the superior border. Two screws were positioned perpendicular to the vertical osteotomy line.
Type 4: The first screw was fixed 5 mm posterior to the osteotomy line and 5 mm inferior to the superior border. The second screw was fixed 5 mm posterior to the osteotomy line and 5 mm superior to the mandibular inferior border. Two screws were placed parallel to the vertical osteotomy line.
Type 5: The first screw was fixed 5 mm posterior to the osteotomy line and 5 mm inferior to the superior border. The second screw was fixed 7 mm posterior to the first screw and 5 mm inferior to the superior border. The third screw was fixed 7 mm posterior to the second screw and 5 mm inferior to the superior border. Three screws were placed perpendicular to the vertical osteotomy line.
Group 2 was the plates-fixation group using monocortical screws and was divided as follows (Fig. 1):
Type 6: A metal plate was fixed using 4 monocortical
screws. The screws were placed between the second premolar
and the first molar, between the first and second molars, and 5 mm inferior to the superior border of the mandible.
Type 7: A metal plate was fixed using 4 monocortical screws. The screws were placed between the second premolar and the first molar, between the first and second molars, and 12 mm inferior to the superior border of the mandible.
Type 8: A metal plate was fixed using 4 monocortical screws. The screws were placed between the second premolar and the first molar, between the first and second molars, and 5 mm superior to the inferior border of the mandible.
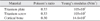
The data obtained in CATIA was imported into a commercially available FEA program, ANSYS version 12 (ANSYS Inc., Canonsburg, PA, USA). A solid element type, "SOLID 186" was chosen to model the bone segments.(Table 1)
The miniplates (Lefort system; Jeil Medical Co., Seoul, Korea) were modeled. The thickness of the actual miniplates was 0.5 mm. The diameter of the actual screws was 2 mm, and the lengths were 7 mm and 10 mm. The mechanical properties of cortical and cancellous bone were assumed to be the same.(Table 2) A load of 10 N was placed on the 90° occlusal plane of both lower first molars.(Fig. 2)
Stress on screws (group 1) and metal plates (group 2), deflection of the central incisor, and stress on bone in the vicinity of screw holes were analyzed.
Maximum von-Mises stress was measured on the screw of type 1. Minimal stress was measured on the screws of type 5.(Table 3)
Maximum deflection was measured on type 1. Types 2 and 4 showed minimal deflection because of the effective distribution of bending moments and torsional moments. (Table 4)
Maximum von-Mises stress was measured on type 1. Minimal stress was measured on type 2.(Table 4)
Stress on group 2 was concentrated on the metal plates in contrast to group 1. Type 6 showed relatively high stress concentration on the plates and screws. Type 8 exhibited minimal stress.(Table 3)
Types 6 and 7 showed minimal deflection because of the effective distribution of moments. In contrast, type 8 showed maximum deflection of the central incisor.(Table 4)
Maximum stress was measured in type 7, and minimal stress was measured in type 6.(Table 3)
SSRO is a common orthognathic surgery in the treatment of dentofacial deformities. Bony segments are stabilized by various fixation methods classified into non-rigid, semi-rigid, and rigid fixation1,6-9. Non-rigid fixation uses wires and has some disadvantages such as prolonged period of intermaxillary fixation and callus formation between both segments. On the other hand, semi-rigid and rigid fixation methods offer sufficient stability of both segments and shorter periods of intermaxillary fixation. The first report on rigid fixation using screws was published by Spiessl10. He proposed that proximal and distal segments be fixed with three compression screws with triangular configuration. There have been various suggestions on the fixation methods to reduce displacement of the condyle and to improve the stability of bony segments in SSRO10-12. Triangular configurations of screws are known to be the most stable method13,14. The semi-rigid fixation method using metal plates and screws can reduce the displacement of the condyle and nerve damage15. This method seems to be less stable than rigid fixation using bicortical screws, however16. The ideal method of fixation has not yet to be found. Furthermore, most reports were on animal studies.
In this study, five rigid fixation methods using screws and three semi-rigid fixation methods using metal plates and screws were compared. The major model of rigid fixation was Spiessl's tripod method. In this study, we found that the rigid fixation model using one screw (type 1) showed relatively high stress around the screw and more displacement on the area of incisor. On the other hand, the rigid fixation model using three screws (type 5) showed the least stress around the screws and bone in the vicinity of screw holes. Such was related to stress distribution. These results suggest that multiple screws have some mechanical advantages. This study also showed that type 4 (two screws were parallel to the vertical osteotomy line) had more mechanical advantages than type 3. This implied that complex mechanical loads from occlusal forces were transferred more effectively in the type 4 method. Type 2 may also be an effective method.
In group 2, we found that higher stress was delivered to the metal plates located on the vertical osteotomy line. Complex loading around the plates causes deflection of metal plates, inferior displacement of the anterior mandible, and relapse. Major forces delivered to the plates are bending and torsion17. Type 8 showed lower von-Mises stress than types 6 and 7, but minimal deflection of central incisors was noted on type 6. Type 6 may be a less stable method from a mechanical prospective, but a more effective method considering surgical stability.
Figures and Tables
Fig. 1
Finite element model. A. Type 1. B. Type 2. C. Type 3. D. Type 4. E. Type 5. F. Type 6. G. Type 7. H. Type 8.

Fig. 2
Boundary conditions of the finite element model of the mandible. (A: fixed, B: force, C: force)

References
1. Park JU. Orthognathic surgery. 2003. Seoul: Koonja Publishing;267–316.
2. Wolford LM. The sagittal split ramus osteotomy as the preferred treatment for mandibular prognathism. J Oral Maxillofac Surg. 2000. 58:310–312.

3. Oguz Y, Uckan S, Ozden AU, Uckan E, Eser A. Stability of locking and conventional 2.0-mm miniplate/screw systems after sagittal split ramus osteotomy: finite element analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009. 108:174–177.

4. Ueki K, Hashiba Y, Marukawa K, Alam S, Nakagawa K, Yamamoto E. Skeletal stability after mandibular setback surgery: bicortical fixation using a 2.0-mm locking plate system versus monocortical fixation using a nonlocking plate system. J Oral Maxillofac Surg. 2008. 66:900–904.

5. Brasileiro BF, Grempel RG, Ambrosano GM, Passeri LA. An in vitro evaluation of rigid internal fixation techniques for sagittal split ramus osteotomies: advancement surgery. J Oral Maxillofac Surg. 2009. 67:809–817.

6. Jafari A, Shetty KS, Kumar M. Study of stress distribution and displacement of various craniofacial structures following application of transverse orthopedic forces--a three-dimensional FEM study. Angle Orthod. 2003. 73:12–20.
7. Holberg C. Effects of rapid maxillary expansion on the cranial base--an FEM-analysis. J Orofac Orthop. 2005. 66:54–66.

8. Proffit WR, Phillips C. Adaptations in lip posture and pressure following orthognathic surgery. Am J Orthod Dentofacial Orthop. 1988. 93:294–302.
9. Nagai I, Tanaka N, Noguchi M, Suda Y, Sonoda T, Kohama G. Changes in occlusal state of patients with mandibular prognathism after orthognathic surgery: a pilot study. Br J Oral Maxillofac Surg. 2001. 39:429–433.

10. Jang HS, Kim YK. A clinical study on the relapse after bssro for the correction of mandibular prognathism. J Korean Assoc Oral Maxillofac Surg. 1996. 22:4–9.
11. Erkmen E, Simsek B, Yucel E, Kurt A. Comparison of different fixation methods following sagittal split ramus osteotomies using three-dimensional finite elements analysis. Part 1: advancement surgery-posterior loading. Int J Oral Maxillofac Surg. 2005. 34:551–558.

12. Yoon OB, Kim YG. A study of von-Mises yield strength after mandibular sagittal split ramus osteotomy. J Korean Assoc Oral Maxillofac Surg. 2002. 28:196–200.
13. Lindorf HH. Sagittal ramus osteotomy with tandem screw fixation. Technique and results. J Maxillofac Surg. 1986. 14:311–316.
14. Haug RH, Barber JE, Punjabi AP. An in vitro comparison of the effect of number and pattern of positional screws on load resistance. J Oral Maxillofac Surg. 1999. 57:300–308.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download