Abstract
Myofibroblastic sarcoma is a rare tumor that mostly develops in the soft tissues of the head and neck. Within the oral cavity, a tongue lesion is the most common. A myofibroblastic sarcoma tends to recur locally instead of metastasizing. We encountered a myofibroblastic sarcoma of the mandible of a 9-year-old male and performed mass excision and additional marginal alveolectomy. So far, there is neither recurrence nor metastasis. We report this case because of the uncommon location of this tumor type and its surgical approach compared to other forms of sarcomas.
In the head and neck, epithelial malignant tumors account for at least 80%, and mesodermal malignant tumors are relatively infrequent1. Among mesodermal malignant tumors, myofibroblastic sarcoma is a very rare disease that can occur in most organs including skin, limbs, abdominal cavity, pelvic cavity, thoracic cavity, and diaphragm but generally afflicts the head and neck such as tongue, floor of the mouth, pharynx, larynx, parapharyngeal space, salivary gland, and maxillary bones2-6. Within the oral cavity, tongue lesion is the most common. Though the treatment has yet to be established clearly due to the low incidence, treatment plans including the extent of surgical excision are determined considering the grade of malignancy, size and location of lesion, age of the patient, invasion into adjacent tissues, and metastasis after biopsy due to various grades of malignancy7. We encountered a case of myofibroblastic sarcoma of the mandible with a 9-year-old male, and we are reporting this case because of the uncommon location of this tumor type and its surgical approach compared to other forms of sarcoma.
In December 2010, a 9-year-old male patient visited us due to the painless soft tissue lesion in the right mandible, which he felt starting a month earlier when he received excisional biopsy of the lesion in the mandible by a dentist and got diagnosed with pyogenic granuloma. Two weeks after the excisional biopsy, however, it recurred; thus, the patient was referred to us after he received excision biopsy again and was finally diagnosed with myofibroblastic sarcoma.
In the clinical examination performed on the day of the first visit, a 3×2 cm reddish lesion with relatively distinct boundary evaginated to the right lingual side of the mandible was identified; the surface was covered with inflammatory granulation tissues, and it had easy bleeding tendency. An ulcer was identified on some part of the surface of lesion.(Fig. 1) #46, 84, and 85 adjacent to the lesion showed medium level of mobility laterally and vertically when the wire fixation placed by the dentist was removed. In the examination by touch, the lesion was found to extend into the mandible. Though the patient experienced inconvenience, there were no spontaneous pain and significant paresthesia in the lower teeth, lower lip, and chin. In the panoramic radiographs, on the #46, 85 apical area, osteolytic lesion with relatively distinct boundary was observed, including invasion of lesion on top of #45 tooth germs.(Fig. 2) The computed tomography (CT) and magnetic resonance imaging (MRI) revealed a lesion with relatively distinct boundary in the mandible destroying the lingual cortical bone and extending to the inside of the mandible without invading adjacent areas such as floor of the mouth, sublingual space, and tongue. There was no lymph node metastasis.(Fig. 3)
On December 31, 2010, the patient underwent mass excision including extraction of #84, 85, 44, 45, 46, and 47 and alveolectomy on the lower part of the lesion under general anesthesia.(Fig. 4) The resected soft mass measured 3×2.5 cm and was easily divided from the surrounding tissues; in the final biopsy, however, tumor cells were detected on the lower part of the lesion. Nonetheless, the tumor was deemed to have been removed completely because additional alveolectomy was performed simultaneously on the lower part of the lesion. Though the patient experienced temporary paresthesia in the right lower lip and chin after the surgery, after 3 months the patient was restored and cured without complications such as inflammation or infection.
In the histological examination, thin and spindle-shaped myofibroblasts were intersected with each other, invading the surrounding tissues locally. Most myofibroblasts had a spindle-shaped core, but some had a circle or a pleomorphic core and showed partial hyperchromatism. Though some pleomorphic cells showed high-grade dysplasia, most myofibroblasts exhibited low-grade dysplasia without tissue necrosis. Blood circulation in the surrounding area was more than sufficient, and mitotic index was relatively low at 5 mitotic figures per 10 high-power fields.(Fig. 5) Moreover, myofibroblast tested positive for immunohistochemical staining with CD34. Considering the histological, clinical, and radiological opinions, the patient was diagnosed with pT1N0M0, stage I, low-grade myofibroblastic sarcoma (LGMS) in the mandible.
The patient did not receive additional treatments including radiation and anticancer treatments; three months after the surgery, removable denture was placed in the edentulous area. Eighteen months after the surgery, there was neither recurrence nor distant metastasis.(Fig. 6) The patient has been examined regularly by the Department of Pediatrics, Oncology, Pedodontics, and Oral and Maxillofacial Surgery.
Myofibroblast is a cell in the intermediate stage of fibroblast's myogenesis process. It is located in the soft tissues of most organs6. During the treatment of wound or reaction of responsive cells, temporary fibroblasts are observed, but they die by apoptosis when the treatment is finished. If there is a problem in this process, they become tumor cells. The reason and phenomenological interpretation of the myofibroblast's differentiation into tumor cell have not been discovered despite the many research studies, and the treatment method for myofibroblastic sarcoma has yet to be established7. This is because there are not enough case reports, myofibroblast has various and complex histological differentiations and grades of malignancy, and its prognosis can change according to the location and size of lesion8. In existing research, high-grade myofibroblastic sarcoma is aggressive, showing more distant metastasis than local recurrence. LGMS, however, shows more local recurrence than distant metastasis and tends to invade into soft tissues8-10.
LGMS occurs 2.5 times more frequently in males than females, generally afflicting soft tissue, fascia, and subcutaneous tissues such as head and neck, limbs, pelvis, lung, chest, abdomen, genitals, diaphragm, thyroid, and skin. Within the head and neck, tongue lesion is the most common followed by salivary gland, floor of the mouth, parapharyngeal space, and occipital area2,3,5-7,9. Mandibular lesion is an extremely rare lesion even for LGMS. Generally occurring in the tongue, it is felt by the patient after the size of the lesion increases without clinical symptom or pain, showing distinct boundaries in radiological images and exhibiting osteoclasia and invasion on some boundaries. This case has similar aspects4.
For general sarcoma, extensive 2-5 cm excision is performed, but the range of surgical excision for LGMS is determined considering the clinical decisions and histological opinions of the operator11. Therefore, the range of excision may be determined according to the age of the patient, size and location of lesion, destruction of adjacent tissues, metastasis, and histological grade of malignancy. Generally, the diagnosis is high grade when combining size larger than 10 cm, deep location, high histological grade of malignancy (high mitotic index >10 mitotic figures per 10 high-power fields), and partial tissue necrosis12. If the diagnosis is high grade after surgical excision, radiation treatment is generally recommended, and anticancer treatment may be used in combination in case of high possibility of distant metastasis11. Fisher reported that, out of 39 LGMS cases, 13 patients (33%) experienced partial recurrence and 3 patients (8%) had distant metastasis, and that, out of 22 cases of high-grade myofibroblastic sarcoma, 7 patients (32%) experienced partial recurrence and 15 patients (68%) had distant metastasis10. According to Mentzel et al.7, out of 18 LGMS cases, 2 patients experienced recurrence, 1 patient had metastasis, 14 patients received surgical excision, and 4 other patients received surgical excision and additional treatments such as radiation and anticancer treatments.
Given the variety of existing treatments and clinical results of myofibroblastic sarcoma, histopathological evaluation and clinical/radiographic determinations are very important factors of prognosis. In particular, for children patients such as the patient in this case, deciding the proper surgical margin is critical while minimizing problems in the mandibular bone. In this case, we were able to obtain a successful treatment result by performing only alveolectomy covering the lesion while minimizing problems in the growth and development of mandible, considering the facts that the lesion had distinct boundaries, there was no invasion into the surrounding tissues except the lingual side of the mandible and #45 permanent tooth germs, the patient was young and he had low pathological grade, and the lesion tended to show more local recurrence than metastasis. Nonetheless, the most important thing is to secure a clean surgical margin, and there is a need to check for recurrence through long-term observation.
Figures and Tables
Fig. 1
Intraoral view of soft tissue mass on the lingual side of the mandible showing granulomatous tissue overgrowth.

Fig. 2
Initial panoramic view showing radiolucent lesion on #85, 46 apical area with loss of crypt wall of #45.

Fig. 3
Radiographic findings of myofibroblastic sarcoma. A. Computed tomography showing osteolytic lesion in the right mandible with cortical destruction on the lingual side. B, C. Magnetic resonance imaging showing 2.5 cm enhancing mass arising from the right mandible with extra-mandibular extension; no gross invasion in the floor of the mouth, tongue, and right sublingual space, with no pathological lymph nodes.
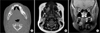
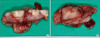
Fig. 4
Resected specimen showing well-encapsulated mass. A. Buccal side view. B. Lower part side view.
References
1. Takácsi-Nagy Z, Muraközy G, Pogány P, Fodor J, Orosz Z. Myofibroblastic sarcoma of the base of tongue. Case report and review of the literature. Strahlenther Onkol. 2009. 185:198–201.
2. Bisceglia M, Magro G. Low-grade myofibroblastic sarcoma of the salivary gland. Am J Surg Pathol. 1999. 23:1435–1436.

3. Jay A, Piper K, Farthing PM, Carter J, Diwakar A. Low-grade myofibroblastic sarcoma of the tongue. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007. 104:e52–e58.

4. Niedzielska I, Janic T, Mrowiec B. Low-grade myofibroblastic sarcoma of the mandible: a case report. J Med Case Rep. 2009. 3:8458.

5. San Miguel P, Fernández G, Ortiz-Rey JA, Larrauri P. Low-grade myofibroblastic sarcoma of the distal phalanx. J Hand Surg Am. 2004. 29:1160–1163.

6. Takahama A Jr, Nascimento AG, Brum MC, Vargas PA, Lopes MA. Low-grade myofibroblastic sarcoma of the parapharyngeal space. Int J Oral Maxillofac Surg. 2006. 35:965–968.

7. Mentzel T, Dry S, Katenkamp D, Fletcher CD. Low-grade myofibroblastic sarcoma: analysis of 18 cases in the spectrum of myofibroblastic tumors. Am J Surg Pathol. 1998. 22:1228–1238.
9. Artopoulou II, Lemon JC, Clayman GL, Chambers MS. Stent fabrication for graft immobilization following wide surgical excision of myofibroblastic sarcoma of the buccal mucosa: a clinical report. J Prosthet Dent. 2006. 95:280–285.

11. Kawaguchi N, Ahmed AR, Matsumoto S, Manabe J, Matsushita Y. The concept of curative margin in surgery for bone and soft tissue sarcoma. Clin Orthop Relat Res. 2004. (419):165–172.

12. Khoury JD, Coffin CM, Spunt SL, Anderson JR, Meyer WH, Parham DM. Grading of nonrhabdomyosarcoma soft tissue sarcoma in children and adolescents: a comparison of parameters used for the Fédération Nationale des Centers de Lutte Contre le Cancer and Pediatric Oncology Group Systems. Cancer. 2010. 116:2266–2274.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download