Abstract
Introduction
Auto-tooth bone graft material consists of 55% inorganic hydroxyapatite (HA) and 45% organic substances. Inorganic HA possesses properties of bone in terms of the combining and dissociating of calcium and phosphate. The organic substances include bone morphogenetic protein and proteins which have osteoinduction capacity, as well as the type I collagen identical to that found in alveolar bone. Auto-tooth bone graft material is useful as it supports excellent bone regeneration capacity and minimizes the possibility of foreign body reaction,genetic diseases and disease transmission.
Materials and Methods
Implant placement combined with osteoinductive regeneration,preservation of extraction socket, maxillary sinus augmentation, and ridge augmentation using block type,powder type, and block+powder type autobone graft materialwere performed for 250 patients with alveolar bone defect and who visited the Department of Oral and Maxillofacial Surgery, College of Dentistry, Dankook University from September 2009 to August 2011.
Results
Clinical assessment: Among the 250 patients of auto-tooth bone graft, clinical assessment was performed for 133 cases of implant placement. The average initial stabilization of placed implants was 74 implant stability quotient (ISQ). Radiological assessment: The average loss of crestal bone in the mandible as measured 6 months on the average after the application of prosthesis load was 0.29 mm, ranging from 0 mm to 3.0 mm. Histological assessment: In the histological assessment, formation of new bone, densified lamellated bone, trabecular bones, osteoblast, and planting fixtures were investigated.
Nowadays, various bone graft materials are developed due to advanced biograft material development technologies; as a result, dento alveolar surgery can handle difficult osseous defects with various methods in the placement of implant, periodontal surgery, and maxillofacial surgery. The auto-tooth bone graft material is a system that treats patients by manufacturing bone graft material from their own extracted teeth. It has first been introduced by the Korea Tooth Bank R&D Center, and has satisfied many clinicians and patients for its osteoconduction as well as osteoinduction capacity.
Auto-tooth bone graft material consists of 55% inorganic and 45% organic substances. Among the inorganic substances, hydroxyapatite (HA) has the characteristics of combining and dissociating calcium and phosphate as those of bone. Organic substances include the bone morphogenetic protein (BMP) and proteins with osteoinduction capacity as well as type I collagen, which is the same as alveolar bone itself. Therefore, they have the same bone remodeling capacity with autogenous bone1.
Auto-tooth bone graft materials are divided into block and powder types. The block type has osteoinduction, capacity via blood wettability and has osteoconduction capacity via space maintaning and creeping substitution and space maintaining abilities; it is remodeled by maintaining space during a specific period. The powder type is supplied based on various sizes of particles, porosity between powders, and blood wettability, osteoconduction, osteoinduction, and creeping substitution abilities.
With above data, autotooth bone graft material is very useful in clinical situations because it supports excellent bone regeneration through osteoinduction and osteoconduction capacity and minimizes foreign body reaction due to genetic homogeneity.
This study is aimed to introduce the bone healing capacity of autotooth bone graft material based on the radiological, histological, and clinical results of implant placement, preservation of extraction socket, maxillary sinus augmentation, and ridge augmentation combined with guided bone regeneration using powder and block type performed at the Department of Oral and Maxillofacial Surgery, College of Dentistry, Dankook University.
Auto-tooth graft materials are divided into the block type and powder type. Block bone graft materials are divided into rootform and rooton types. The root form is suitable for the preservation and reconstruction of extraction socket because it resembles a dental root. The root-on type is suitable for horizontal or vertical ridge augmentation because it resembles a general block bone. In addition, both types can be used for the preservation of the extraction socket, aesthetic restoration of the alveolar bone, restoration of perforated sinus membrane, and enhancement of initial stabilization of implant. Blocktype bone graft material should be hydrated with physiological saline for 15-30 minutes before use because it is supplied after being demineralized and dried. Properly hydrated block can be controlled by operators with surgical knife or scissors and attached and fixed firmly without any additional instrument due to its excellent elasticity and flexibility.(Fig. 1) Powdertype bone graft materials are divided into crown type (Auto BT-Enamel) and root type (Auto BT-Dentin). Auto BT enamel is suitable for maintaining volume due to bone healing capacity derived from osteoconduction and late resorption because most of it consists of inorganic enamel. In contrast, Auto BT dentin is suitable for osteoinduction regeneration, ridge augmentation, and maxillary bone graft derived from osteoinduction and osteoconduction because it consists of dentin and cement containing many organic substances (type I collagen).(Fig. 2)
Implant placement combined with osteoinductive regeneration, preservation of extraction socket, maxillary sinus augmentation, and ridge augmentation using block type, powder type, and block+powder type autobone graft material were performed for 250 patients with alveolar bone defect and who visited the Department of Oral and Maxillofacial Surgery, College of Dentistry, Dankook University from September 2009 to August 2011.(Fig. 3) Surgeries were performed by professors and residents of the Department of Oral and Maxillofacial Surgery, College of Dentistry, Dankook University.
Among the 190 patients, powder type was used for 25 patients in osteoinduction regeneration, 95 patients in implant placement combined with osteoinduction regeneration, 16 patients in the preservation of extraction socket, and 15 patients in maxillary sinus augmentation. The block+powder type was used for 13 patients in osteoinduction regeneration, 38 patients in implant placement combined with osteoinduction regeneration, and 5 patients in ridge augmentation. The block type was used for 17 patients in the preservation of extraction socket. Afterward, the success of the surgery was assessed via clinical, radiological, and histological tests. (Fig. 4)
There were more male patients than female patients, and patients were mostly in their 40s and 50s. With respect to maxillary and mandibular cases, mandibular cases numbered 142, and maxillary cases, 108. Most recipient sites were extraction socket caused by periodontal disease.
Osteoinduction regeneration and implant placement combined with osteoinduction regeneration (GBR).
Auto-tooth bone graft material was placed with an implant in case of osseous defect larger than 2 mm vertically or horizontally around the placed implant. Membrane use was determined by the operator. If the amount of graft material was insufficient, it was mixed with other bone graft material.
Auto-tooth graft material was used for patients whose edentulous bone was less than 10 mm high from the sinus floor via lateral or crestal approach. Only maxillary bone graft was performed, and implant was placed after 4-6 months in cases securing the initial stabilization of the implant was difficult due to the height of the edentulous bone.
The patients' age, gender, location of placement, initial and secondary stabilization of implant, complications during and after surgery, mobility of implant at the final diagnosis, presence of exudate, edema, and bleeding after probing were investigated. Initial and secondary stabilization of implant was measured by Osstell Mentor (Integration Diagnostics Ltd., Goteborg, Sweden).
For the radiological assessment, bone height was measured right after placement and at the final diagnosis. The distance between the top of the placed implant and the top of bone in contact with the placed implant was measured as the mesial and distal surface by magnifying panoramic photos and computed tomography scan images 10 times with Marosis (Marotech, Seoul, Korea), a digital radioautograph viewer.
This assessment was conducted for 6 patients who read the purpose of the histological test and signed the consent form for biopsy. Five mm bone sample was collected from the crestal bone of 6 patients after 3.5 months on the average with 2 mm trephine bur. The samples were fixed with 10% formalin solution immediately and demineralized for 1 week with Formic AcidSodium Citrate. They were then washed, embedded in paraffin, cut in 4-5 ym, subjected to H&E staining, and examined by optical and polarizing microscope.
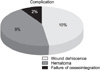
Among the 250 patients of autotooth bone graft, clinical assessment was performed for 133 cases of implant placement. Average age was 50.8, ranging from 17 to 71 years. Male patients numbered 154, and female patients, 96. A total of 93 implants were placed in the maxillary and mandibular posterior, and 40 implants, in the maxillary and mandibular anterior. Block+powdertype auto-tooth bone graft material was used for 38 patients, and powder type, for other patients. The average initial stabilization of placed implants was 74 implant stability quotient (ISQ), and average secondary stabilization was 83 ISQ. For postsurgery complications, wound dehiscence developed in 10 cases. Among them, 7 cases had no loss of crestal bone with good secondary treatment, and 3 cases had average crestal bone loss of 2 mm. In 9 cases, hematoma developed after the surgery but was treated without any serious problem. In 2 cases, osseointegration failed; the implants were removed, and new ones were placed again immediately.(Fig. 5) The average period of examination upon completion of denture was 9 months, ranging from 4 to 12 months. All cases maintained normal functions.
The average loss of crestal bone in the mandible as measured 6 months on the average after the application of prosthesis load was 0.29 mm, ranging from 0 mm to 3.0 mm. In the case of the maxilla, average loss of crestal bone after 6 months on the average was only 0.1 mm.(Fig. 6)
In the histological assessment, formation of new bone, densified lamellated bone, trabecular bones, osteoblast, and planting fixtures were investigated. Among the planting fixtures, enamel tended to be resorbed by the surrounding new bone or existed alone, whereas dentin tended to form new bones in a specific direction.(Fig. 7)
Since the first result wherein teeth generated bones2 as proven by the study of Urist2 wherein he examined the generation of bone after applying demineralized tooth in parts other than bone, the capacity of tooth to generate bones has not been investigated. Note, however, that recent research such as the study of Kim et al.1 which proved the successful use of artificially processed tooth as graft material, and the report of Murata et al.3 in Japan wherein bone was generated from demineralized tooth are based on prior research as well as the idea that the components of tooth are similar to those of bone.
No doubt, autogenous bone graft is ideal for the reconstruction of hard tissue defects. It has bone formation, osteoconduction, osteoinduction, and osseointegration capacities, and it does not trigger foreign body reaction; it also ensures fast healing. Note, however, that it is difficult to obtain a sufficient amount, and secondary defect develops in the donor site4. In the case of allograft, there is some doubt as to the amount of bone formation proteins necessary for proper osteoinduction, and contagion may develop5,6. On the other hand, xenograft is not popular among operators because of immune rejection response by heterologous proteins, possibility of contagion, and high cost7. As a result, there have been many research studies on the development, application, and effect of allograft, xenograft, and synthetic graft. The bone graft material to replace autogenous bone has been highly anticipated.
Recently, synthetic graft materials manufactured with HA, etc., have been developed and used. HA is easily combined with osseous tissues since its chemical structure is similar to that of tooth and osseous tissues, but it has only osteoconduction ability by acting as scaffold in the bone remodeling process without osteoinduction capacity8.
Autogenous bone is known to have both osteoconduction and osteoinduction capacities due to sufficient bone formation proteins in cortical bone, and it can provide bone regeneration capacity via stem cells if marrow cavity is included in the graft.
Although many research studies and application methods of graft material have been introduced, it is still difficult to obtain bone graft material that has the advantages of autogenous bone sans the disadvantages. In fact, many research studies to develop bone graft material to replace autogenous bone have been conducted. In particular, Kim et al.1 introduced a bone graft material using extracted autotooth as new bone graft material to overcome the disadvantages of allograft, xenograft, and synthetic graft.
Auto-tooth bone graft material is an innovative bone graft material with all the advantages of autogenous bone owing to its very similar components to bone and is very useful in clinical situations. It also addresses patients' repulsion to allograft and xenograft by providing excellent biocompatibility without causing immune response, foreign material reaction, or contagion. In addition, it has osteoinduction, osteoconduction, and creeping substitution capacities9-11 , and it can be manufactured in various sizes and shapes.
Tooth extracted from a person is classified as environmental waste and should be disposed of by an extracted material processor. Note, however, that the use of autotooth is not illegal if the patient agrees to process and use his/her own teeth. Unless contaminated by an infectious lesion, a tooth does not cause problems even when the root rest is in the alveolar bone. There are also surgeries wherein the root rest is left intentionally to preserve the alveolar bone12,13. In addition, Kim et al.14 reported that 90% of the tooth's organic components are type I collagen, which is very important in the calcification of bone. Ike and Urist15 proved that BMP2 included in enamel has capacity for osteoinduction, which is important in bone formation16. Gao et al.17 reported that enamel has growth factors such as insulinlike growth factor (IGF)-II, BMP-2, and transforming growth factor (TGF)-beta like bone. According to Saygin et al.18 cement and its mother cell have TGFbeta, IGFI, and plateletderived growth factor. In other words, the enamel and cement of tooth have many growth factors that help bone formation.
Based on these, the Department of Oral and Maxillofacial Surgery, College of Dentistry, Dankook University performed radiological and histological assessments of autotooth bone graft material made of extracted toothwhich is currently regarded as wasteby grafting it in human extraction socket. In this research, autotooth bone graft material showed fast bone healing capacity without inflammatory reaction in all recipient sites regardless of age and location of surgery and recorded high success rate without serious complications.
Currently, there are various bone graft materials; in particular, auto-tooth bone graft material has been studied aggressively as a material to overcome the disadvantages of allograft, xenograft, and synthetic graft without losing bone regeneration capacity like autogenous bone. The Department of Oral and Maxillofacial Surgery, Dankook University has applied it clinically since October 2008. In clinical applications, autotooth bone graft material does not have genetic and infectious risks; it is as strong as other graft materials, providing good bone generation through osteoinduction and osteoconduction as well as excellent initial bone remodeling capacity. Based on these results, we concluded that autotooth bone graft material should be researched further as a good bone graft material with osteoconduction and osteoinduction capacities to replace autogenous bone, which has many limitations.
Figures and Tables
 | Fig. 6After 6 months, computed tomography (CT) scan around buccal wall defect (arrow) showed more radio-opacity than the initial implantation with auto-tooth bone grafting. A. Initial CT view. B. CT view after 6 months. |
 | Fig. 7Resorbing enamel (yellow arrows) and dentin (blue arrows) were noted. Some enamel stayed independent (orange arrows) without surrounding bone in subject group patient I. A. Optical microscopic view (H&E stanining, ×40). B. Polarizing microscopic view (H&E staining, ×40). C, D. Optical microscopic view (H&E staining, ×100). |
References
1. Kim YK, Kim SG, Byeon JH, Lee HJ, Um IU, Lim SC. Development of a novel bone grafting material using autogenous teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010. 109:496–503.

3. Murata M, Akazawa T, Takahata M, Ito M, Tazaki J, Hino J, et al. Bone induction of human tooth and bone crushed by newly developed automatic mill. J Ceram Soc Jpn. 2010. 118:434–437.

4. Kim YK, Yun PY, Kim SG, Lim SC. Sinus bone graft using combination of autogenous bone and BioOss(R): comparison of healing according to the ratio of autogenous bone. J Korean Assoc Oral Maxillofac Surg. 2007. 33:654–659.
5. Quattlebaum JB, Mellonig JT, Hensel NF. Antigenicity of freeze-dried cortical bone allograft in human periodontal osseous defects. J Periodontol. 1988. 59:394–397.

6. Schwartz Z, Mellonig JT, Carnes DL Jr, de la Fontaine J, Cochran DL, Dean DD, et al. Ability of commercial demineralized freeze-dried bone allograft to induce new bone formation. J Periodontol. 1996. 67:918–926.

7. Sogal A, Tofe AJ. Risk assessment of bovine spongiform encephalopathy transmission through bone graft material derived from bovine bone used for dental applications. J Periodontol. 1999. 70:1053–1063.

8. Han T, Carranza FA Jr, Kenney EB. Calcium phosphate ceramics in dentistry: a review of the literature. J West Soc Periodontol Periodontal Abstr. 1984. 32:88–108.
9. Park SS, Kim SG, Lim SC, Ong JL. Osteogenic activity of the mixture of chitosan and particulate dentin. J Biomed Mater Res A. 2008. 87:618–623.

10. Gomes MF, dos Anjos MJ, Nogueira TO, Guimarães SA. Histologic evaluation of the osteoinductive property of autogenous demineralized dentin matrix on surgical bone defects in rabbit skulls using human amniotic membrane for guided bone regeneration. Int J Oral Maxillofac Implants. 2001. 16:563–571.
11. Catanzaro-Guimarães SA, Catanzaro Guimarães BP, Garcia RB, Alle N. Osteogenic potential of autogenic demineralized dentin implanted in bony defects in dogs. Int J Oral Maxillofac Surg. 1986. 15:160–169.

13. Fareed K, Khayat R, Salins P. Vital root retention: a clinical procedure. J Prosthet Dent. 1989. 62:430–434.

14. Kim SG, Kim HK, Lee SC. Combined implantation of particulate dentine, plaster of Paris, and a bone xenograft (Bio-Oss) for bone regeneration in rats. J Craniomaxillofac Surg. 2001. 29:282–288.

15. Ike M, Urist MR. Recycled dentin root matrix for a carrier of recombinant human bone morphogenetic protein. J Oral Implantol. 1998. 24:124–132.

16. Goncalves EAL. Study of the process of bone repair in surgical defects implanted with demineralized autogenous dentin matrix in radius of dog [thesis]. 1997. Bauru: University of Sao Paulo.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download