Abstract
Congenital syngnathia refers to the fusion of bony tissues, a rare disorder with only 41 cases reported in the international literature from 1936 to 2009. The occurrence of syngnathia without any other associated systemic disease or congenital anomaly is extremely rare. This report presents a case of congenital syngnathia with unilateral maxillomandibular bony adhesion without any other oral or maxillofacial anomaly. No recommended protocol for surgery exists due to the rarity of the disorder. There is a very low survival rate for the few patients who have forgone surgical management. This case describes a 74-year-old female patient who was suffering from limitation of mouth opening and was subsequently diagnosed with congenital syngnathia. The surgical staff performed separation surgery and reconstructed the malformed oral vestibule and cheek using the radial forearm free flap operation.
Congenital fusion of the jaws is a condition that can not open the mouth at birth and the bony fusion composed of oral mucosa or maxilla and mandible. Cases of congenital synechiae with soft tissue have been generally reported in literature, but congenital syngnathia with hard tissue is rare. It was first reported in 1936, with only 41 cases reported until 20091. In particular, congenital syngnathia that is not associated with systemic syndrome or maxillofacial defect is rarely found in literature. Since congenital syngnathia causes, dyspnea, difficulty in oral feeding, and abnormal growth of the jaws and face, early surgical treatment is necessary. However, that no standard treatment for congenital syngnathia is established because the prevalence rate is low and few patients live without surgical treatment. For the patient diagnosed with congenital syngnathia as featured in this report, we performed separative surgery and radial forearm free flap operation. We present a report on the good treatment outcome having no complication and refusion together with a review of literature.
A 74-year-old female patient with chief complaint of fusion of the left jaws came to the Department of Oral and Maxillofacial Surgery, Dankook University Hospital on 9th, March, 2011.(Fig. 1) The patient has neither opened her mouth nor chewed since birth, taking in liquid diet for 74 years. She has no family history of such fusion. The clinical findings revealed fusion in the gingiva area equivalent to the left edentulous alveolar ridge of the maxilla and mandible and no buccal vestibule as a result of perfect fusion in the buccal gingival area.(Fig. 2) There was no tooth in the oral cavity, and she had never experienced tooth extraction. There was facial asymmetry due to left mandibular deficiency caused by syngnathia. The maximum mouth opening showed 0 mm in the symphysis of the jaws, and any mandibular movement in all directions was impossible. The panoramic radiograph showed fusion of the left edentulous alveolar ridge (Fig. 3), and the facial 3 dimension image acquired through a computed tomography scan was used to observe the bony fusion of the left edentulous alveolar ridge.(Fig. 4) There was neither adhesion of both temporomandibular joints (TMJs) nor coronoid process hyperplasia.(Fig. 5) Moreover, the image from the bone scan (99mTc-MDP; Symbia E, Siemens, Germany) revealed a finding of hot spot in the affected alveolar bone.(Fig. 6)
On March 16 of the same year, since it was impossible to perform normal intubation for general anesthesia, fiber-optic intubation using endoscopy was done to perform separative surgery and reconstructed the right buccal mucosa and oral vestibule. Such reconstructive surgery included extension of lip split incision, separative surgery of the maxilla and mandible after collar incision, detachment of the affected temporalis muscle, coronoidectomy and radial forearm free flap operation to lead to mouth opening movement after the surgery.(Figs. 7-9) Before the surgery, we conducted the Allen's test for blood circulation compatibility and microvascular anastomosis to connect the radial artery and vena comitants in the radial forearm free flap to the branches of the facial artery and internal jugular vein. As a result of continuous mouth opening movement 7 days after the surgery, the maximum mouth opening was 45 mm from the symphysis of the jaws. To control the size of the transplanted flap, flap de-bulking operation was performed on 8th, July of the same year under oral intubation and general anesthesia.(Fig. 10) Now, 6 months after the surgery, the maximum opening was 45 mm from the symphysis of the jaws.
The fusion defect of the maxilla/mandible in the jawbones or oral mucosa is an extremely rare maxillofacial deformity. Such deformity is called various medical terms including congenital fusion of the jaws or gums, zygomaticomandibular fusion, intraoral band, intra-alveolar synechiae, congenital bony syngnathia, and mandibulomaxillary synostosis1. Fusion by the soft tissues of the maxilla and mandible is called synechiae, whereas fusion by osseous tissue is called syngnathia. Synechiae has been reported extensively in literatures, and its treatment is simple rather than complicated. However, syngnathia is a rarer deformity than fusion by soft tissue; unilateral bony fusion in the jaws has been reported even more rarely1. Most cases of congenital syngnathia are additionally accompanied by congenital defects such as cleft lip, cleft palate, microglossia, micrognathism, and TMJ disease1.(Table 1) In particular, cleft palate is most common. At least 41 cases of congenital syngnathia had been reported until 2009 since the first case was reported by Burket2 in 1936, whereas only 18 cases of congenital syngnathia with no additional congenital defect or syndrome had been reported until 20091. Some scholars classified the patient conditions, such as the classification of Dawson et al.3, and classification of Laster et al.4 as a modified classification.(Tables 2, 3) The patient in this case is Type 1 under the classification of Dawson et al.3 and Type 1a under the classification of Laster et al.4.
The etiologic factor of congenital bony syngnathia has yet to be revealed, but the following causes are assumed: long-term survival of buccopharyngeal membrane, amniotic band syndrome, incest, drugs during pregnancy, abnormality of fetal stapedial artery, early loss of neural crest cell, and injury5-9. According to Nanda, syngnathia occurred with cleft palate in the rabbit injected with vitamin A10. Humphrey maintained that, since the elevation of palatal shelves is delayed due to the reduced swallowing reflex of a fetus in the early stages of pregnancy, the contact of pharyngeal membrane and glossal membrane in a palate results in syngnathia together with cleft palate11. Laster maintained that such deformity is related to the time and period of external damage and that external damage occurred after week 12 of pregnancy does not cause cleft palate, micrognathism, fusion of zygomatic bone and upper jawbone or fusion of cortical bones4. In the present case, there was no ankylosis of both TMJs, but the overgrowth of left coronoid process was noted. No fusion of the left coronoid process, zygomatic bone, and upper jaw was observed, however. As a result of left mandibular deficiency due to syngnathia, the left mandibular branch was 1 cm shorter than the right branch, and facial asymmetry was observed.
The important point in treating this disease is to secure the airway and feeding through nasogastric tube insertion at birth, and then remove the fusion area by surgical procedure, administering active physical treatment to prevent recurrence in the future. If possible, early surgery is recommended to avoid the ankylosis of both TMJs and prevent secondary developmental maxillofacial deformity that may be caused by syngnathia.
In literature on the treatment of congenital syngnathia, many authors used approaches such as temporo-preauricular approach, submental approach, intraoral approach3,12, and suggested interpositional flap using temporalis muscle or buccal mucosa, insertion of an implant such as silastic sheets between separated soft tissues to prevent recurrence3, or physical treatment using oral appliance after the surgery12,13. Fusion reportedly recurred in most cases despite such efforts3,8. Recently, Choi et al.14 reported a case of using radial forearm free flap to prevent refusion and secure proper mouth opening after surgery in the acquired syngnathia. How ever, the decrease of mouth opening after surgery led to TMJ surgery and lip surgery using temporalis muscle in the secondary surgery14. In the present case, to prevent the decrease of mouth opening after the surgery, detachment of the affected temporalis muscle and coronoidectomy were additionally performed, and radial forearm free flap operation was done simultaneously with the separation of the maxilla and the mandible. Profuse bleeding occurred during the operation in the blood vessels around the base of the skull, and the cause was thought to be venous rupture due to the excessive extension of the vein connected to the base of the skull when the mouth was opened after the separation of the mandibular bone. Therefore, notifying the patient and caregiver well ahead of the surgery of the possibility of blood transfusion against excessive bleeding during the operation is recommended, including performing mouth opening carefully to prevent excessive bleeding during the operation. To avoid recurrence caused by the refusion of soft tissue, ankylosis of the TMJ, and atrophy of masticatory muscle after the surgery, mouth opening training was done 7 days after the operation. Choi et al.14 maintained in their research that, as mouth opening can be reduced due to atrophy of the masticatory muscle after the surgery despite enough buccal mucosa when using radial forearm free flap, continuous monitoring of mouth opening and physical treatment are required. In this case, the patient showed successful opening 4 months after the surgery; however, since the size of free flap was somewhat excessive, secondary flap reduction operation was performed.
In conclusion, we could secure enough mouth opening for the patient with congenital syngnathia and draw an effective result without any refusion after the surgery. However, case reports on patients undergoing the radial forearm free flap operation are rare, and there is a shortage of discussion on comparative study of cases using other operations other than the radial forearm free flap operation. Therefore, more research on the refusion pattern and maintaining mouth opening in case of the radial forearm free flap operation are deemed necessary.
To treat a patient with congenital syngnathia effectively, it is important to secure the airway of the patient, ensure proper nutrition, and secure enough mouth opening with no recurrence pattern. Therefore, it is recommended to prevent any recurrence after surgery by using the proper operation, including maintaining the mouth opening to prevent ankylosis of the TMJ through continuous physical therapy.
For a patient with congenital syngnathia, we successfully performed separative surgery and radial forearm free flap and presented a report on the satisfactory result without any complications and recurrence.
Figures and Tables
Fig. 1
74-year-old woman with facial asymmetry due to left mandibular hypoplasia resulting in the fusion of the left maxillo-mandibular alveolar ridge.

Fig. 2
Adhesion of the left commissural and retrocommissural oral cheek to the fused arches on the left side, which continued posteriorly as complete adhesion of the buccal mucosa to the slopes of the upper and lower arches, resulting in the absence of the buccal vestibule.

Fig. 3
Panoramic view showing left mandibular ramus hypoplasia resulting in the unilateral bony fusion of the left maxillary-mandibular alveolar ridges.

Fig. 4
A computerized 3 dimension reconstruction of the skull showed the bony fusion of the alveolar crest of the maxilla and mandible.

Fig. 5
Computerized 3 dimension reconstruction of the skull. A. There was neither temporomandibular joint (TMJ) ankylosis nor coronoid process hyperplasia in the right skull. B. There was no TMJ ankylosis, but coronoid process hyperplasia was noted on the left side.
Fig. 6
The bone scan (99mTc-MDP) revealed a hot spot in the left maxillo-mandibular bony fusion area.
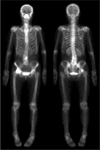
Fig. 8
The maxillo-mandibular fusion area is separated by a saw, and left coronoidectomy was done to favor mouth opening training.

References
1. Naikmasur VG, Sattur AP, Joshi SK, Rai A. Congenital syngnathia: case report and review of literature. Cleft Palate Craniofac J. 2010. 47:654–660.

2. Burket LW. Congenital bony temporomandibular ankylosis and facial hemiatrophy. JAMA. 1936. 106:1719–1722.

3. Dawson KH, Gruss JS, Myall RW. Congenital bony syngnathia: a proposed classification. Cleft Palate Craniofac J. 1997. 34:141–146.

4. Laster Z, Temkin D, Zarfin Y, Kushnir A. Complete bony fusion of the mandible to the zygomatic complex and maxillary tuberosity: case report and review. Int J Oral Maxillofac Surg. 2001. 30:75–79.

5. Poswillo D. The pathogenesis of the first and second branchial arch syndrome. Oral Surg Oral Med Oral Pathol. 1973. 35:302–328.

6. Hegtvedt AK. Peterson LJ, editor. Diagnosis and management of facial asymmetry. Principles of oral and maxillofacial surgery. 1992. Philadelphia: Lippincott;1400–1401.
7. Rao S, Oak S, Wagh M, Kulkarni B. Congenital midline palato-mandibular bony fusion with a mandibular cleft and a bifid tongue. Br J Plast Surg. 1997. 50:139–141.

8. Kamata S, Satoh K, Uemura T, Onizuka T. Congenital bilateral zygomatico-mandibular fusion with mandibular hypoplasia. Br J Plast Surg. 1996. 49:251–253.

10. Nanda R. Maxillomandibular ankylosis and cleft palate in rat embryos. J Dent Res. 1970. 49:1086–1090.

11. Humphrey T. The relation between human fetal mouth opening reflexes and closure of the palate. Am J Anat. 1969. 125:317–344.

12. Subramanian B, Agrawal K, Panda K. Congenital fusion of the jaws: a management protocol. Int J Oral Maxillofac Surg. 2010. 39:925–929.





 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download