Abstract
Calcifying epithelial odontogenic tumor (CEOT) is a rarely reported benign tumor, accounting for 0.4-3% of all odontogenic tumors. Approximately 150 cases have been reported in the literature between 1958 and 2003. The age range of CEOT varies from 8 to 92 years with mean of 36.9 years, and the occurrence of the lesion in both genders is almost equal. It has 2 clinico-topographic variants: the intraosseous (94%) and the extraosseous (6%) type. The intraosseous type has a predilection for mandible (maxilla : mandible ratio of 1 : 2). The intraosseous CEOT commonly associated with non-erupted teeth accounts for more than half (52%) of the cases and usually appears as painless swelling that causes bony expansion. The location of diffused round-shaped calcifying material is inside the connective tissue stroma and epithelial islands. The tumors tend to be located toward the tooth crown, which usually has a unilocular radiolucent region containing variant radiopaque materials radiologically. In this paper, we report a case of CEOT occurring in the left mandibular first premolar of a 23-year-old female and present a brief review of the literature.
Calcifying epithelial odontogenic tumor (CEOT) is known as a pindborg tumor and is a rarely reported tumor accounting for 0.4-3% of all odontogenic tumors1. Approximately 150 cases have been reported between 1958 and 2003, but there is insufficient evidence to indicate the long-term behavior of this tumor2. The age range of CEOT varies from 8 to 92 years with mean of 36.9 years, and the occurrence of the lesion in both genders is known to be almost equal2,3. It is largely classified as intraosseous (94%, central) and extraosseous type (6%, peripheral). The intraosseous type has a predilection for mandible (maxilla : mandible ratio of 1 : 2), with the prevalence rate of the molar region about three times higher than that of the premolar region. About 52% of intraosseous CEOT usually appears in association with non-erupted or impacted teeth and as a painless swelling mass with cortical bone expansion3. It has biological properties similar to those of intraosseous ameloblastoma and normally occurs in the reduced enamel epithelium on the dental lamina remnants and tooth crown. As for the differences between CEOT and ameloblastoma, the epithelial cells do not look like ameloblast, and the location of diffused round-shaped calcifying material is inside the connective tissue stroma and epithelial islands4. The tumors tend to be located toward the crown of non-erupted teeth, which usually has a unilocular radiolucent region containing variant radiopaque materials radiologically. CEOT contains calcifying masses or homogenous non-cellular material within the tumor epithelium and stroma5. In this paper, we report a case of CEOT occurring in the left mandibular first premolar of a 23-year-old female patient and present a brief review of the literature.
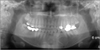
A 23-year-old female patient visited our hospital with chief complaint of discomfort from the left maxillary third molar (#28) and feeling of irritation when swallowing. The panoramic radiography showed a radiolucent image with clear boundary of radiopaque lesions around the impacted teeth and crown of the left mandibular first premolar (#34). No remarkable symptoms- such as pain, edema, bleeding, and root resorption of neighboring teeth (left mandibular canine, left mandibular second premolar)-were observed, and the roots of neighboring teeth were diverged. With no mobility and reaction to the percussion of neighboring teeth, there were no sensation of painful pressure, induration and fluctuation upon palpation in the related area.
She has no medical history of surgery related to the left mandibular premolar or significant systemic treatment record except taking preventive medicine for the slight increase of the thyroid hormone level and taking medicine for chronic rhinitis.
When she visited our hospital, there were radiolucent lesions surrounding the radiopaque lesions from #33 to #35 in the panoramic radiography, but no fistula formation in the oral cavity was observed. The mandibular canal passes under the bottom of the lesions with mental nerve through the buccal cortical bone of the crown of #34.(Fig. 1) In the dental vitality test on neighboring teeth, the cold test and electric pulpal test also showed negative reaction. The routine dental three dimensional computerized tomography scans taken before the surgery showed expansion of buccal cortical bone and mandibular canal, mental nerve slightly displaced to the bottom in #34 and clear radiopaque lesions in the radiolucent lesions with obvious boundary.
Reconstructive surgery on bone defects was performed under general anesthesia through planned mass removal and tibial bone grafting on September 16, 2010. Such operation included sulcular incision, flap elevation, detaching the mass from the neighboring tissues, extraction of the related tooth origin (#34), and mass removal. There were no findings on the mass attachment with the neighboring tissues, and the normal neighboring tissues were properly preserved. To reconstruct the defective region, particulated marrow and cancellous bone (PMCB) measuring 2×2 cm was collected from the left tibia. After the bone defects were filled with PMCB, absorbable atelo-collagen sponge (Teruplug; Termo Co., Tokyo, Japan) was used as barrier membrane on the buccal side.(Fig. 2)
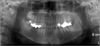
Biopsies by Hematoxylin and eosin staining, Congo red staining, and polarizing microscope were performed for the mass. A variety of acidophilic amyloid tissues and calcifying tissues could be observed from such biopsies, including the cluster of polygonal epithelial tissue strands. The amyloid tissues can be seen with red color in Congo red staining and with bright green color in polarizing microscope, which is used for analyzing amyloid material by polarization of double retraction method. Since the surgery result was favorable, she was discharged from the hospital four days after the surgery, and the stitch out was performed in the outpatient clinic. The panoramic radiography taken after the surgery on September 18, 2010 showed good healing condition after mass removal and tibial bone grafting surgery.(Fig. 3) Sensory paralysis in the left lower lip persisted, but such was probably due to the slight tension applied to the mental nerve in the retraction process during the surgery. The extraction procedure for tooth #28 as the patient's chief complaint was performed. Observations including the possibility of tumor recurrence are underway on a three-month basis in the outpatient clinic, and there are no specific complications and findings of recurrence to date.
CEOT is a relatively rarely reported tumor accounting for about 1% of all odontogenic tumors3,4. Since its histological development has yet to be revealed clearly, there are theories that it originated with the stratum intermedium of dental organ6 and with dental lamina7. CEOT occurs in all age ranges but mainly in the third to fifth decades in age groups, with no special difference by gender8. The main common location is the posterior region of mandible, and it is a clinically painless growing mass mainly. In case of occurrence in the upper jaw, however, it behaves more aggressively to include nasal cavity or maxillary sinus, and it can be accompanied by clinical symptoms such as nasal bleeding, nasal obstruction, and headache. Radiologically, it can be shown as unilocular or multilocular radiolucent image with clear boundary, containing radiopaque materials of various sizes and densities in many cases. In about 50% of the total cases of occurrence, it appears in connection with the impacted teeth or crown of non-erupted teeth9. In cases wherein no radiopaque materials are included, it may be mistaken as a dentigerous cyst. CEOT has lower tendency to penetrate into the bony trabecular space compared with ameloblastoma which is more invasive form9. Malignant change is also extremely rare5.
Histologically, it is arranged in the form of islands with polygonal epithelial cells falling, connected strands, or thin sheets its surroundings are fibrous stroma composed of atypical acidophilic amyloid tissue and calcified tissue.(Fig. 4) There is an intercellular bridge connecting the polygonal cells. Homogeneous acidophilic materials are observed between epithelial cells, and various forms of calcifying materials are found mainly in its surroundings. The histological classification can include (1) the case with small amyloid and calcifying tissues, (2) the case with full amyloid and calcifying tissues, and (3) the clear cell variant, the dominant clear cell as epithelial cell with clear cytoplasm4,9-12. CEOT's two histological characteristics-calcifying and amyloid formation-are considered destructive yet productive for self-limited growth9. This acidophilic calcification is still controversial, but there are many opinions on one amyloid type due to its positive reaction to Congo red or thioflavine T. However, there are also opinions on the kind of degenerated tissue, i.e., type IV collagen or basal lamina, enamel, or dead skin cell13.
In this case, the clear cell was not observed histologically it is regarded as the case with full amyloid and calcifying tissues based on the classification above. If the clear cell is predominant, it is called a clear cell variant, a type that is well observed in the peripheral lesion (extraosseous type)4. In addition, the destruction of cortical bone as an intraosseous lesion was not observed in this case, through which it can be inferred as a type with less aggression. However, each classification has similar recurrence rate.
The mixed tumor of CEOT and adenomatoid odontogenic tumor AOT was first reported by Damm et al.14 in 1983. In addition, Cheng et al.1 presented a report on the genuine malignant CEOT in 2002. The case presented for the first time in this paper revealed histologically strong staining, abnormal cell division, and polymorphism together with swelling in the right mandibular body1.
The treatments for CEOT are generally diverse, ranging from enucleation and curettage to mandibulectomy and maxillectomy as the more fundamental procedures3. The choice of treatment will differ depending on the radiological, histological, and clinical findings on each lesion.
The present case showed self-limited growth it was of the unilocular type, with the lesions surrounded by clear radiopaque borders. The computed tomography scans also showed slight expansion of cortical bone without any destruction of the bone. Mass removal and border grinding procedures were carried out accordingly, with the panoramic radiography taken 10 months after the surgery showing no findings of recurrence.(Fig. 5)
Given the short follow-up period, it seems premature to make a conclusion on the long-term prognosis from the present case. Nonetheless, CEOT is generally defined as an aggressive tumor with about 14% recurrence rate9. In this case, it is compared with invasive ameloblastoma, and a more invasive, aggressive treatment plan may be recommended8. However, recent studies referred to CEOT as less aggressive tumor3,4 and recommended conservative enucleation and thin border grinding in the neighboring bone as treatment plan4.
In summary, we presented a report together with a review of related literature on a case showing good progress after mass removal and tibial bone grafting procedure in CEOT, an extremely rare type among the odontogenic benign tumors. More long-term follow-up is believed to be necessary to monitor future recurrence and stability after the surgery.
Figures and Tables
Fig. 1
The radiolucent mass contains some agglomerated radiopaque materials around the impacted left mandibular first premolar (A) and Dental CT view (sagittal view) (B). The mandibular canal passes just beneath the mass.

Fig. 2
The lesion does not appear as bony perforation but slightly bony expansion (A), and the crown is exposed (B). Calcifying materials are scattered on the inner side of mass (C) and after tibial bone graft (D).

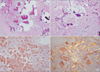
Fig. 4
Deep-stained calcifying materials and eosinophilic amyloids. The epithelial cells shaped like strands surround the calcifying materials. The amyloids show red color in Congo red staining and bright apple green color- which means bi-refringence-in polarizing microscopic view. A. Optical microscopic view (H&E staining, ×40). B. Optical microscopic view (H&E staining, ×200). C. Optical microscopic view (Congo red staining, ×200). D. Polarizing microscopic view (Congo red staining, ×200).
References
1. Cheng YS, Wright JM, Walstad WR, Finn MD. Calcifying epithelial odontogenic tumor showing microscopic features of potential malignant behavior. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002. 93:287–295.

2. Rapidis AD, Stavrianos SD, Andressakis D, Lagogiannis G, Bertin PM. Calcifying epithelial odontogenic tumor (CEOT) of the mandible: clinical therapeutic conference. J Oral Maxillofac Surg. 2005. 63:1337–1347.

3. Philipsen HP, Reichart PA. Calcifying epithelial odontogenic tumour: biological profile based on 181 cases from the literature. Oral Oncol. 2000. 36:17–26.

4. Neville BW, Damm DD, Allen CM, Bouquot JE. Oral and maxillofacial pathology. 2002. 3rd ed. Philadelphia: W. B. Saunders.
5. Deboni MC, Naclério-Homem Mda G, Pinto DS Junior, Traina AA, Cavalcanti MG. Clinical, radiological and histological features of calcifying epithelial odontogenic tumor: case report. Braz Dent J. 2006. 17:171–174.

6. Gon F. The calcifying epithelial odontogenic tumor: report of a case and a study of its histogenesis. Br J Cancer. 1965. 19:39–50.
7. Takeda Y, Suzuki A, Sekiyama S. Peripheral calcifying epithelial odontogenic tumor. Oral Surg Oral Med Oral Pathol. 1983. 56:71–75.

8. Gopalakrishnan R, Simonton S, Rohrer MD, Koutlas IG. Cystic variant of calcifying epithelial odontogenic tumor. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006. 102:773–777.

9. Franklin CD, Pindborg JJ. The calcifying epithelial odontogenic tumor. A review and analysis of 113 cases. Oral Surg Oral Med Oral Pathol. 1976. 42:753–765.
10. Anavi Y, Kaplan I, Citir M, Calderon S. Clear-cell variant of calcifying epithelial odontogenic tumor: clinical and radiographic characteristics. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003. 95:332–339.

11. Kumamoto H, Sato I, Tateno H, Yokoyama J, Takahashi T, Ooya K. Clear cell variant of calcifying epithelial odontogenic tumor (CEOT) in the maxilla: report of a case with immunohistochemical and ultrastructural investigations. J Oral Pathol Med. 1999. 28:187–191.
12. Schmidt-Westhausen A, Philipsen HP, Reichart PA. Clear cell calcifying epithelial odontogenic tumor. A case report. Int J Oral Maxillofac Surg. 1992. 21:47–49.
13. Sapp JP, Eversole LR, Wysocki GP. Contemporary oral and maxillofacial pathology. 2004. 2nd ed. New York: Elsevier.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download