Abstract
Background
The DEL blood type, a very weak D variant, is a major concern in the field of transfusion medicine because of its potential to cause anti-D alloimmunization. We investigated the molecular basis of serologically D-negative phenotypes, including the DEL type, and the distribution of other blood group systems in the Korean population using the recently developed multiplex ligation-dependent probe amplification (MLPA) assay.
Methods
Blood group genotyping using the MLPA assay and RhCE phenotyping were performed on randomly selected 95 D-negative red blood cell products. The MLPA results were verified by multiplex PCR for the RHD promoter, exons 4, 7, and 10 and by direct sequencing of RHD exon 9.
Results
Out of 95 cases, total deletion of the RHD was observed in 74 cases (77.9%) and four cases (4.2%) had an RHD-CE-D hybrid allele. The other 17 cases (17.9%) had an RHD(1227G>A) allele, which was further confirmed by sequencing analysis. The RhCE phenotypes of RHD(1227G>A) alleles were composed of 14 Cce and 3 CcEe, and all 60 cases of the ce phenotype were revealed to have a total deletion of the RHD. Genotyping results and allele distribution of the other 17 blood group systems were consistent with previous reports on the East Asian population.
Conclusions
MLPA assay correctly determined RHD genotype, including RHD-CE-D hybrid alleles or RHD(1227G>A) allele, and other clinically relevant blood group genotypes in D-negative Koreans. The use of MLPA assay on serologically D-negative individuals may help improve transfusion safety by preventing anti-D alloimmunization.
The Rh blood group D antigen is highly immunogenic in the human blood group system, and anti-D alloimmunization can cause severe hemolytic transfusion reactions and hemolytic disease in the fetus and newborn [1]. DEL type is a very weak D variant that cannot be detected by routine serological tests and presents as a D-negative phenotype unless adsorption and elution studies are performed [23]. In addition, DEL type can cause anti-D alloimmunization despite small amounts of D antigen on red blood cell (RBC) surfaces. Several cases of anti-D alloimmunization resulting from RBC transfusion of DEL type have been reported [4567]. Currently, about 30 RHD alleles associated with DEL type have been reported, showing differences in distribution based on ethnicity [2]. In Caucasians, the frequency of DEL type among serologically D-negative individuals is 1/1,000–1/3,000, and RHD(885G>T) and RHD(IVS3+1G>A) are the most common DEL alleles. In East Asians, 15–20% of serologically D-negative individuals are DEL type, and the RHD(1227G>A) allele is the most common [891011].
Owing to the very low frequency of the D-negative phenotype (0.15%) in Korea, ‘RhD-Negative Blood Club’ was organized to assist the supply of D-negative blood products since 1973 [812]. However, Seo et al [12] reported that 20 individuals with DEL type (n=16, 14.5%), weak D (n=2, 1.8%), and partial D (n=2, 1.8%) were classified as D-negative among 110 RhD-Negative Blood Club members. Therefore, the accurate determination of D variant (including DEL type) is important to protect D-negative individuals from inadvertent alloimmunization to the D antigen. Several RHD genotyping strategies have been proposed specifically for East Asians. The proposed methods use RHD-specific multiplex PCR for the detection of total- or partial deletion and are followed by PCR with sequence-specific priming (PCR-SSP) or exon 9 sequencing to detect DEL alleles [81213].
Recently, a multiple ligation-dependent probe amplification (MLPA) assay has been developed to detect RHD variants and zygosity, as well as the 17 other blood group systems [1415]. Compared with previously proposed strategies, the MLPA assay has more advantages, as the presence, absence, and copy number of 48 blood group alleles and 112 variant alleles can be determined simultaneously [1415]. Furthermore, unlike the most widely used comprehensive blood group genotyping platforms such as the PreciseType HEA Molecular Beadchip (Immucor, Warren, NJ, USA) and the Progenika ID CORE XT (Progenika Biopharma-Grifols, Bizkaia, Spain), the MLPA assay can detect four frequent DEL alleles [RHD(1227G>A), RHD(885G>T), RHD (3G>A), and RHD(IVS3+1G>A)] [1617].
The performance of the MLPA assay has not been validated in the East Asian population with serologically D-negative phenotype. In this study, we investigated the molecular basis of the D-negative phenotype, including the DEL type, and determined the distribution and prevalence of other blood group genotypes in the Korean population.
We investigated 95 randomly selected samples of D-negative RBC products that were supplied by the Korea Red Cross Blood Service and the Hanmaum Blood Center in Korea between August 2015 and October 2015. The D antigen status of the RBC products was confirmed by D typing using two different anti-D reagents [Bioclone (Ortho-Clinical Diagnostics, Raritan, NJ, USA) and Anti-D (RH1) IGM1 (Diagast, Loos, France) in the Korean Red Cross Blood Service; Bioclone and Bioscot (Millipore, Livingstone, UK) in the Hanmaum Blood Center], and the indirect antiglobulin technique (IAT) in each Blood Center. An adsorption-elution test was not performed routinely by blood centers.
All blood samples were serotyped for C/c and E/e antigens using monoclonal anti-C, -c, -E, and -e reagents (Ortho-Clinical Diagnostics) with the standard tube method according to the manufacturer's recommendations. This study was approved by the Institutional Review Board of Severance Hospital, Yonsei University Health System (4-2015-0882).
Genomic DNA was isolated using the QIAamp DSP DNA Blood Mini kit (Qiagen, Hilden, Germany) according to the manufacturer's
protocol, and genomic DNA concentration and purity were assessed using a spectrophotometer (NanoDrop 2000, Thermo Fischer Scientific, Waltham, MA, USA).
We used commercial SALSA MLPA Probemixes P401-A1, P402-A1, and P403-A1 Blood Group Genotyping kits (MRC-Holland, Amsterdam, the Netherlands) for the MLPA assay. The three probe mixes contained a total of 129 probes, which included 104 wild type and/or mutation probes to determine the presence, absence, and copy number of the major blood group alleles and variant alleles. The other 25 reference probes included were selected from chromosomal regions supposed to be chromosomally stable in diseases. All procedures were carried out according the manufacturer's protocol. In brief, ligation was performed using 100 ng of genomic DNA in the following steps: denaturation at 98℃ for 5 minutes, hybridization with each SALSA Probemix at 60℃ for 16 hours, ligation reaction by Ligase-65 (MRC-Holland) at 54℃ for 15 minutes, and ligase inactivation by incubation at 98℃ for 5 minutes. Finally, multiplex PCR was performed using fluorescence-labeled universal primers, dNTPs, PCR buffer, and polymerase for 35 cycles (95℃ for 30 seconds, 60℃ for 30 seconds, 72℃ for 1 minute) using a C1000 thermal Cycler (BioRad, Cressier, Switzerland). The fragments were analyzed using an ABI 3130 Genetic Analyzer (Applied Biosystems, Foster, CA, USA) and GeneMarker 2.2 software (SoftGenetics, State College, PA, USA). Zygosity was determined as the signal ratio between tested samples and control samples.
Multiplex PCR was performed to confirm the RHD genotype of MLPA results classified as total RHD gene deletion, RHD-CE-D hybrid, and DEL type. Three exons (exon 4, 7, and 10) and the promoter region were selected for amplification to detect the RHD gene (Table 1). In each multiplex PCR reaction, a 434-bp fragment of the human growth hormone gene was included as the internal control. The PCR reactions were performed with 50–100 ng of genomic DNA containing AccuPower PCR Premix (Bioneer, Daejeon, Korea) and 0.5 µM of each primer in a 20 µL total volume. PCR amplification was performed using a C1000 thermal cycler (Bio-Rad) with an initial denaturation at 95℃ for 10 minutes, followed by 35 cycles of 30 seconds at 95℃, 30 seconds at 50℃ for set A or 30 seconds at 60℃ for set B, and 30 seconds at 72℃. The presence or absence of RHD exons and the internal control were determined by electrophoresis in a 2% agarose gel.
Direct sequencing of the RHD exon 9, including the exon 9-intron 9 boundary, was performed in MLPA assay RHD(1227G>A)-positive samples to verify the results. The PCR reaction was performed in a 20 µL reaction mixture containing AccuPower PCR Premix (Bioneer), 50 ng genomic DNA, and 0.5 µM of each primer (Table 1). PCR amplification was performed at 37℃ for 2 minutes for the uracil-DNA glycosylase reaction by incubating at 95℃ for 10 minutes, followed by 35 cycles of 95℃ for 30 seconds, 60℃ for 30 seconds, and 72℃ for 60 seconds. Sequencing reactions were performed using a PRISM BigDye Terminator v3.1 cycle sequencing kit (Applied Biosystems). The DNA samples containing amplified products were added to Hi-Di formamide (Applied Biosystems), and the mixture was incubated at 95℃ for 5 minutes, cooled for 5 minutes on ice, and then analyzed using an ABI Prism 3730 DNA analyzer (Applied Biosystems).
Three RHD genotypic patterns were apparent in the MLPA analysis, and these patterns were confirmed using multiplex PCR for the promoter, and exons 4, 7, and 10 of RHD gene, as summarized in Table 2. Among the 95 cases, total deletion of the RHD gene was observed in 74 cases (77.9%) where all RHD wild-type probe combination signals were absent. Four cases (4.2%) contained the RHD-CE-D hybrid allele showing only the 5′-UTR and exon 10 of RHD gene. The remaining 17 cases (17.9%) showed positive signals at the 5′-UTR and exons 3, 4, 5, 6, 7, 9, and 10 of the RHD gene and were assumed to be the non-deletion type. For all the non-deletion types, only the RHD(1227G>A) mutation probe showed a positive signal in MLPA analysis. The RHD(1227G>A) mutation was further confirmed by sequencing analysis.
Among the 95 total cases, RHCE*C/RHCE*c heterozygotes and RHCE*c/RHCE*c homozygotes of C/c alleles comprised 26 (27.4%) and 69 (72.6%) cases, respectively, and RHCE*E/RHCE*e heterozygotes and RHCE*e/RHCE*e homozygotes of E/e alleles numbered 11 (11.6%) and 84 (88.4%), respectively. The most commonly predicted RhCE phenotype from the MLPA assay was ce (60, 63.2%), followed by Cce (24, 25.3%), cEe (9, 9.5%), and CcEe (2, 2.1%).
The prevalence of the other 16 blood group genotypes and expected phenotypes in the 95 RhD-negative donors are described in Table 3. For the MNS blood group, the numbers of cases with GYPA*01/01, GYPA*01/02, and GYPA*02/02 genotypes were 28 (29.5%), 43 (45.3%), and 24 (25.3%), respectively. The numbers of cases with GYPB*03/04 and GYPB*04/04 genotypes were 13 (13.7%) and 82 (86.3%), respectively. Variants of the MNS blood group such as Gp.Mur or Gp.Dane were not detected. The most common phenotypic combination of the MNS blood group was M+N+S-s+ (38.9%), followed by M-N+S-s+ (25.3%) and M+N-S-s+ (22.1%). In the Duffy blood group, the numbers of cases with FY*01/01, FY*01/02, and FY*02/02 genotypes were 80 (84.2%), 13 (13.7%), and 2 (2.1%), respectively. In the Kidd blood group, the numbers of cases with JK*01/01, JK*01/02, and JK*02/02 genotypes were 25 (26.3%), 48 (50.5%), and 22 (23.2%), respectively. The numbers of cases with DI*01/02 and DI*02/02 genotypes in the Diego blood group were 12 (12.6%) and 83 (87.4%), respectively. In the Dombrock blood group, the numbers of cases with DO*01/01, DO*01/02, and DO*02/02 genotypes were 4 (4.2%), 15 (15.8%), and 78 (82.1%), respectively. All 95 cases were homozygous for LU*02/02, KEL*02/02, KEL*04/04, KEL*07/07, DI*04/04, YT*01/01, SC*01/01, CO*01/01, LW*05/05, GE*01/01, CROM*01/01, KN*01/01, IN*02/02, and OK*01/01.
The frequency of the D-negative phenotype varies from 0.5% in East Asians to 3-7% in Africans and 12-18% in Caucasians [2021]. In Caucasians, the most common cause of the D-negative phenotype is a homozygous total deletion of the RHD gene, and other causes are rare [1]. In Africans, 67% of D-negative individuals have at least a single copy of RHD*ψ, inactivated by a 37-bp insertion in intron 3 and exon 4. This 37-bp duplication generates a reading frameshift and a premature stop codon [20]. Additionally, RHD-CE-D hybrid genes are relatively common in D-negative Africans. These hybrid genes consist of RHD exons 1, 2, 9, and 10 and exons 4-8 from the RHCE gene, producing no D antigen [120].
In Koreans, about 75% of D-negative individuals have a total deletion of the RHD gene, and 9-10% have RHD-CE-D hybrid genes. In addition, 13-16% of D-negative Koreans have the RHD(1227G>A) allele, which is the most common cause of the DEL type in East Asians [81213]. In this study, total deletion of the RHD gene (74/95, 77.9%) was most commonly observed using the MLPA assay. Other genotypes were RHD-CE-D hybrid gene (4/95, 4.2%) and the RHD(1227G>A) allele (17/95, 17.9%). All DEL cases with the RHD(1227G>A) allele were further confirmed by sequencing RHD exon 9. This result indicating the molecular cause of the D-negative phenotype in Koreans is consistent with previous reports [821].
The DEL type is phenotypically determined by the absence of agglutination in the indirect antiglobulin test and a positive result in the adsorption/elution technique [322]. As the sensitivity of the indirect antiglobulin test may vary across laboratories and false-positive results in adsorption/elution technique may also occur, it is difficult to accurately define the borderline between the DEL type and a true D-negative phenotype [2]. This leads to the necessity of RHD genotyping in blood donors, because it can exclude D variant (including DEL type) donors among serologically D-negative blood donors [2202324].
DEL type arises from several molecular mechanisms, including splice site mutations, missense mutations, frame shift mutations, RHD-CE-D hybrid, and partial deletion of the RHD gene [291125]. The most common DEL type in the East Asian population is caused by the RHD(1227G>A) allele. Although this substitution is a silent single nucleotide polymorphism, the substitution results in aberrant frame shift or exon deletion, and generates D protein with a weak antigen-presenting function [11]. Additionally, other alleles such as RHD(3G>A), RHD(28C>T), RHD(53T>C), RHD(251T>C), RHD(410C>A), and RHD(1222T>C) have also been identified in the East Asian population [81225]. However, the typical alleles that were identified in Caucasians, RHD(885G>T), RHD(IVS3+1G>A), RHD(1252insT), and RHD(IVS5-38del4) have not been found in East Asians [11]. In this study, all non-deletion type MLPA results were identified as the RHD(1227G>A) allele. Although the current MLPA assay can detect only four frequent DEL alleles [RHD(1227G>A), RHD(885G>T), RHD(3G>A), and RHD(IVS3+1G>A)], other mutation probes can be easily added according to the population-specific data on molecular causes of the DEL type (i.e. a probe to detect RHD(1222T>C) allele in Koreans) [8122627].
Previous reports showed that the DEL type is highly associated with the RhC+ phenotype (Cc or CC) [21219282930]. Among 126 DEL cases in Taiwan, Wang et al [28] reported that 107 (84.9%) cases were Cc and 19 (15.1%) cases were CC. Srijinda et al [29] also reported that 42 (84.0%) cases were Cc and eight (16.0%) cases were CC among 50 DEL cases in Thailand. This association between DEL type and RhC phenotype might be explained by the suppressive effect of C, where D antigen density is suppressed by the C antigen [19]. Recently published reports showed a similar distribution pattern in Korea, and the cc phenotype was exclusively found in D-negative individuals with total RHD deletion. Therefore, this study proposed the addition of RhCE phenotyping in the first step of a diagnostic approach to discriminate the D-negative phenotype from total RHD deletion inferred by ‘C-E-c+e+’ phenotype [12]. In this study, the RhC phenotype was identified as the Cc phenotype in all DEL cases, and the DEL allele with the cc phenotype was not found.
Since numerous blood group antigens can be accurately determined by a single test, several comprehensive blood group genotyping platforms have been developed and are currently used in diverse situations [31]. The most important clinical utility of this test is to identify donors lacking high-prevalence antigens or multiple common antigens like those for rare donor programs. The frequency of the D-negative phenotype is 0.15% in Koreans, about 1/100th of the frequency in the Caucasian population [8]. Considering that the DEL type is relatively common in D-negative Koreans, the true D-negative individuals fall into the rare blood donor category. Comprehensive blood group genotyping methods could be valuable tools for accurately determining the RHD genotype (including DEL type) and other blood group antigens in serologically D-negative Korean donors.
In this study, we further evaluated the performance of an MLPA assay in 17 blood group systems other than the RHD gene, and the distribution data for major alleles from 17 blood group systems were similar to the previous data in the East Asian population [2732]. In the MNS blood group system, the Ss genotype frequency showed ethnic variation. The frequencies of S/S, S/s, and s/s genotypes were 0.14, 0.40, and 0.46 among the Europeans and 0.08, 0.12, and 0.80 among the Asians, respectively [133]. Our findings showed similar results in that 0.14 of S/s genotypes, 0.86 of s/s genotypes, and no cases of SS genotype were identified in D-negative cases. In the Duffy blood group system, two Fya-negative cases were encountered, similar to previous results [33]. The frequency of the Fya-negative phenotype in the Korean population is very low compared with that in the European population, and it is extremely difficult to find Fya-negative RBCs for anti-Fya alloimmunized patients [3435]. Other relevant antigens, including Lutheran, Kell, Yt, Scianna, Colton, LW, Gerbich, Cromer, Knops, Indian, and Ok blood group systems, are not polymorphic in the Korean D-negative individuals.
In conclusion, the MLPA assay correctly determined RHD genotype including RHD-CE-D hybrid alleles or RHD(1227G>A) allele, and other clinically relevant blood group genotypes in D-negative Koreans. The use of MLPA assay in serologically D-negative individuals may help improve transfusion safety by preventing anti-D alloimmunization.
Figures and Tables
Table 1
Primers used for multiplex PCR and sequencing

| Method | Genomic target | Nucleotide sequence | Product size (bp) | References |
|---|---|---|---|---|
| Multiplex PCR (set A) | RHD exon 4 | F: CCACATGAACATGATGCACA | 127 | [18] |
| R: CAAACTGGGTATCGTTGCTG | ||||
| RHD exon 10 | F: TAAGCAAAAGCATCCAA | 186 | [6] | |
| R: ATGGTGAGATTCTCCT | ||||
| Multiplex PCR (set B) | RHD exon 7 | F: GTTGTAACCGAGTGCTGGGGATTC | 123 | [19] |
| R: TGCCGGCTCCGACGGTATC | ||||
| RHD promoter | F: TCCACTTTCCACCTCCCTGC | 256 | [19] | |
| R: GCAGCCAACTTCCCCTGTG | ||||
| Multiplex PCR (internal control) | HGH | F: TGCCTTCCCAACCATTCCCTTA | 434 | [13] |
| R: CCACTCACGGATTTCTGTTGTGTTTC | ||||
| Sequencing | RHD exon 9 | F: AGATACTGTCGTTTTGACACACAAT | 463 | In this study |
| R: GCTGAGGACTGCAGATAGGG |
Table 2
RhCE phenotype and RHD analysis using the MLPA assay
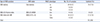
Table 3
Genotype frequency of RBC antigens in the 95 RhD-negative samples

Acknowledgements
This study was supported by a faculty research grant of Yonsei University College of Medicine for 2011 (6-2011-0089).
References
1. Daniels G. Human blood groups. Oxford: Blackwell Publishing Ltd;2013.
2. Wagner FF. RHD PCR of D-negative blood donors. Transfus Med Hemother. 2013; 40:172–181.
3. Shao CP, Maas JH, Su YQ, Kohler M, Legler TJ. Molecular background of Rh D-positive, D-negative, D(el) and weak D phenotypes in Chinese. Vox Sang. 2002; 83:156–161.

4. Wagner T, Kormoczi GF, Buchta C, Vadon M, Lanzer G, Mayr WR, et al. Anti-D immunization by DEL red blood cells. Transfusion. 2005; 45:520–526.

5. Yasuda H, Ohto H, Sakuma S, Ishikawa Y. Secondary anti-D immunization by Del red blood cells. Transfusion. 2005; 45:1581–1584.

6. Kim KH, Kim KE, Woo KS, Han JY, Kim JM, Park KU. Primary anti-D immunization by DEL red blood cells. Korean J Lab Med. 2009; 29:361–365.

7. Yang HS, Lee MY, Park TS, Cho SY, Lee HJ, Lim G, et al. Primary anti-D alloimmunization induced by “Asian type” RHD (c.1227G>A) DEL red cell transfusion. Ann Lab Med. 2015; 35:554–556.
8. Kim JY, Kim SY, Kim CA, Yon GS, Park SS. Molecular characterization of D- Korean persons: development of a diagnostic strategy. Transfusion. 2005; 45:345–352.

9. Kormoczi GF, Gassner C, Shao CP, Uchikawa M, Legler TJ. A comprehensive analysis of DEL types: partial DEL individuals are prone to antiD alloimmunization. Transfusion. 2005; 45:1561–1567.

10. Dajak S, Krstic JL, Kormoczi G, Dogic V, Burilovic V. Characteristics and frequency of DEL phenotype detected by indirect antiglobulin test in Dalmatia county of Croatia. Transfus Apher Sci. 2014; 50:210–213.

11. Chen DP, Sun CF, Ning HC, Wang WT, Tseng CP. Comprehensive analysis of RHD splicing transcripts reveals the molecular basis for the weak anti-D reactivity of Del -red blood cells. Transfus Med. 2016; 26:123–129.
12. Seo MH, Won EJ, Hong YJ, Chun S, Kwon JR, Choi YS, et al. An effective diagnostic strategy for accurate detection of RhD variants including Asian DEL type in apparently RhD-negative blood donors in Korea. Vox Sang. 2016; 111:425–430.

13. Luettringhaus TA, Cho D, Ryang DW, Flegel WA. An easy RHD genotyping strategy for D- East Asian persons applied to Korean blood donors. Transfusion. 2006; 46:2128–2137.

14. Haer-Wigman L, Veldhuisen B, Jonkers R, Loden M, Madgett TE, Avent ND, et al. RHD and RHCE variant and zygosity genotyping via multiplex ligation-dependent probe amplification. Transfusion. 2013; 53:1559–1574.
15. Haer-Wigman L, Ji Y, Loden M, de Haas M, van der Schoot CE, Veldhuisen B. Comprehensive genotyping for 18 blood group systems using a multiplex ligation-dependent probe amplification assay shows a high degree of accuracy. Transfusion. 2013; 53:2899–2909.

16. Goldman M, Nuria N, Castilho LM. An overview of the Progenika ID CORE XT: an automated genotyping platform based on a fluidic microarray system. Immunohematology. 2015; 31:62–68.

17. Paccapelo C, Truglio F, Antonietta Villa M, Revelli N, Marconi M. HEA BeadChip technology in immunohematology. Immunohematology. 2015; 31:81–90.
18. Aubin JT, Le Van Kim C, Mouro I, Colin Y, Bignozzi C, Brossard Y, et al. Specificity and sensitivity of RHD genotyping methods by PCR-based DNA amplification. Br J Haematol. 1997; 98:356–364.

19. Wagner FF, Frohmajer A, Flegel WA. RHD positive haplotypes in D negative Europeans. BMC Genet. 2001; 2:10.
20. Daniels G. Variants of RhD--current testing and clinical consequences. Br J Haematol. 2013; 161:461–470.
21. Peng CT, Shih MC, Liu TC, Lin IL, Jaung SJ, Chang JG. Molecular basis for the RhD negative phenotype in Chinese. Int J Mol Med. 2003; 11:515–521.

22. Xu W, Zhu M, Wang BL, Su H, Wang M. Prospective evaluation of a transfusion policy of RhD-positive red blood cells into DEL patients in China. Transfus Med Hemother. 2015; 42:15–21.

23. Flegel WA. Molecular genetics and clinical applications for RH. Transfus Apher Sci. 2011; 44:81–91.

24. Sandler SG, Flegel WA, Westhoff CM, Denomme GA, Delaney M, Keller MA, et al. It's time to phase in RHD genotyping for patients with a serologic weak D phenotype. College of American Pathologists Transfusion Medicine Resource Committee Work Group. Transfusion. 2015; 55:680–689.
25. Li Q, Hou L, Guo ZH, Ye LY, Yue DQ, Zhu ZY. Molecular basis of the RHD gene in blood donors with DEL phenotypes in Shanghai. Vox Sang. 2009; 97:139–146.
26. Veldhuisen B, van der Schoot CE, de Haas M. Multiplex ligation-dependent probe amplification (MLPA) assay for blood group genotyping, copy number quantification, and analysis of RH variants. Immunohematology. 2015; 31:58–61.
27. Ji Y, Wen J, Veldhuisen B, Haer-Wigman L, Wang Z, Loden-van Straaten M, et al. Validation of the multiplex ligation-dependent probe amplification assay and its application on the distribution study of the major alleles of 17 blood group systems in Chinese donors from Guangzhou. Transfusion. 2017; 57:423–432.

28. Wang YH, Chen JC, Lin KT, Lee YJ, Yang YF, Lin TM. Detection of RhD(el) in RhD-negative persons in clinical laboratory. J Lab Clin Med. 2005; 146:321–325.

29. Srijinda S, Suwanasophon C, Visawapoka U, Pongsavee M. RhC phenotyping, adsorption/elution test, and SSP-PCR: the combined test for D-elute phenotype screening in Thai RhD-negative blood donors. ISRN Hematol. 2012; 2012:358316.

30. Scott SA, Nagl L, Tilley L, Liew YW, Condon J, Flower R, et al. The RHD (1227G>A) DEL-associated allele is the most prevalent DEL allele in Australian D- blood donors with C+ and/or E+ phenotypes. Transfusion. 2014; 54:2931–2940.
31. Keller MA. The role of red cell genotyping in transfusion medicine. Immunohematology. 2015; 31:49–52.

32. Chang HE, Hong YJ, Kim H, Hwang SM, Park JS, Lee SW, et al. Genotyping of 19 red cell antigens, including RHD, using liquid bead arrays. Clin Chim Acta. 2016; 462:111–117.
33. Hong YJ, Chung Y, Hwang SM, Park JS, Kwon JR, Choi YS, et al. Genotyping of 22 blood group antigen polymorphisms and establishing a national recipient registry in the Korean population. Ann Hematol. 2016; 95:985–991.

34. Lim CS, Kim YK, Lee KN. The Duffy blood group genotypes in Asian populations. Korean J Blood Transfus. 2007; 18:145–151.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download