Dear Editor,
Bacteria continuously develop, acquire, and spread numerous resistance patterns shortly after new antibiotics reach the market. Recently, carbapenem-resistant Enterobacteriaceae (CRE) and colistin-resistant Acinetobacter baumannii are emerging, which may lead us into the pre-antibiotic era. Pipelines of new antibiotics are becoming thinner and thinner across all therapeutic areas due to difficulties in innovation and challenges of regulatory hurdles. Under such a situation, maintaining antibiotic effectiveness in the long term requires not only innovation to develop new antibiotics, but also conservation of the effectiveness of existing antibiotics.
Antibiotic cycling or rotation consists of the sequential use of antibiotics not sharing a common mechanism of resistance, which could be considered as a strategy for conservation. Aminoglycoside consumption has continuously decreased during the recent five years [1]. The rates of amikacin or gentamicin-resistant Klebsiella pneumoniae, Pseudomonas aeruginosa, and Acinetobacter spp. also showed declining trends according to data from the Korean Nationwide Surveillance of Antimicrobial Resistance (KONSAR) program [2]. The decreasing prevalence of amikacin and tobramycin resistance in some Gram-negative bacteria was associated with decreased consumption levels of these antimicrobial agents in a single-center study [3]. Aminoglycosides, except amikacin, can be considered as old drugs; however, they remain key roles in the treatment of infections. They also possess potent bactericidal activity against some CRE [4].
We investigated the correlation of aminoglycoside consumption and its resistance in P. aeruginosa using a nationwide surveillance and antibiotic prescription database to provide background data on the effectiveness of antibiotic cycling at the national level. Data on antibiotic usage in Korea from 2002 to 2013 were acquired from the database of the National Health Insurance Service-National Sample Cohort (NHIS-NSC), a population-based cohort established to provide public health researchers and policy makers with representative information regarding the utilization of health insurance and health examinations among citizens [5]. We also included prescription data for systemic antibiotics based on the Anatomical Therapeutic Chemical Classification System in this study. Amount of use was standardized by Daily Defined Dose (DDD) and expressed as DDD per 1,000 inhabitants daily. Gentamicin and amikacin-resistance rates of P. aeruginosa isolated from Korean general hospitals were obtained from the Korean Antimicrobial Resistance Monitoring System [6]. This study was approved by the Institutional Review Board of the National Health Insurance Service Ilsan Hospital (NHIMC 2017-03-026). We analyzed the data using SAS software version 9.2 (SAS Institute, Cary, NC, USA). The relationship between antibiotic use and resistance was evaluated by simple correlation analysis. The significance level was set at P<0.05.
Despite the worsening resistance rates in other antibiotic classes in Korea [6], aminoglycosides might be the only ones showing decreasing trends of consumption and resistance rates. National gentamicin and total aminoglycoside consumption has continuously decreased and shown strong correlations with gentamicin-resistance rate of P. aeruginosa isolated from general hospitals with more than 100 beds (Fig. 1).
National amikacin consumption has continuously decreased after 2006. Amikacin-resistance rate of P. aeruginosa in the same year did not correlate with amikacin usage. However, it showed strong correlation at two-year intervals (Fig. 2).
The reason for this difference is currently unclear, but we suspected it to be due to different gentamicin- and amikacin- resistance mechanisms. Gentamicin resistance is mediated mainly by aminoglycoside modification, but 16S rRNA methyltransferase production constitutes a high level of resistance to aminoglycoside, especially to amikacin [7].
Other researchers reported that restriction of gentamicin and tobramycin decreased the resistance rate to both antimicrobials especially in P. aeruginosa in the 1980s [8 9]. The study was performed during the period of introduction of amikacin and emergence of plasmid-mediated resistance to gentamicin. In Korea, Ku et al [3] reported that decreasing prevalence of ami-kacin and tobramycin resistance in P. aeruginosa isolates were associated with decreased consumption levels of these antimicrobials; but this correlation was not observed with gentamicin. This was discordant with our study and that of Lai et al [10], which showed good correlation with gentamicin and amikacin. The study by Ku et al [3] was a single center analysis from 2001 to 2011, and could be affected by patients' characteristics, infection control policy, and microbiological factors.
The strength of this study is that it is based on nationwide surveillance and antibiotic prescription database spanning an extended period; thus the findings are representative of the population. This study suggests that less aminoglycoside consumption correlates with less resistance levels, hence the need for an antibiotic cycling strategy at the national level.
Acknowledgment
This study was supported by a grant (2016-20-001) from the National Health Insurance Service Ilsan Hospital. This study acquired permission for using NHIS-NSC (REQ0000007609).
References
1. Yoon YK, Park GC, An H, Chun BC, Sohn JW, Kim MJ. Trends of Antibiotic Consumption in Korea According to National Reimbursement Data (2008-2012): A Population-Based Epidemiologic Study. Medicine (Baltimore). 2015; 94:e2100. PMID: 26579825.
2. Yong D, Shin HB, Kim YK, Cho J, Lee WG, Ha GY, et al. Increase in the Prevalence of Carbapenem-Resistant Acinetobacter Isolates and Ampicillin-Resistant Non-Typhoidal Salmonella Species in Korea: A KONSAR Study Conducted in 2011. Infect Chemother. 2014; 46:84–93. PMID: 25024870.
3. Ku NS, Choi JY, Yong D, Kim JM, Lee K. Correlations between aminoglycoside consumption and aminoglycoside resistance in Gram-negative bacteria at a tertiary-care hospital in South Korea from 2001 to 2011. Int J Antimicrob Agents. 2013; 41:394–395. PMID: 23305659.
4. Almaghrabi R, Clancy CJ, Doi Y, Hao B, Chen L, Shields RK, et al. Carbapenem-resistant Klebsiella pneumoniae strains exhibit diversity in aminoglycoside-modifying enzymes, which exert differing effects on plazomicin and other agents. Antimicrob Agents Chemother. 2014; 58:4443–4451. PMID: 24867988.
5. Lee J, Lee JS, Park S, Shin SA, Kim KW. Cohort Profile: The National Health Insurance Service–National Sample Cohort (NHIS-NSC), South Korea. Int J Epidemiol. 2017; 46:e15. PMID: 26822938.
6. Korea Centers for Disease Control. Korean Antimicrobial Resistance Monitoring System 2013 Annual Report. last visited on 19 June 2017. http://cdc.go.kr/CDC/cms/cmsFile-Download.jsp?fid=136&cid=21224&fieldName=attachGrp&index=5.
7. Wachino J. Exogenously acquired 16S rRNA methyltransferases found in aminoglycoside-resistant pathogenic Gram-negative bacteria: an update. Drug Resist Updat. 2012; 15:133–148. PMID: 22673098.
8. Young EJ, Sewell CM, Koza MA, Clarridge JE. Antibiotic resistance patterns during aminoglycoside restriction. Am J Med Sci. 1985; 290:223–227. PMID: 3936358.
9. Gerding DN. Aminoglycoside resistance in Gram-negative bacilli during increased amikacin use. Comparison of experience in 14 United States hospitals with experience in the Minneapolis Veterans Administration Medical Center. Am J Med. 1985; 79:1–7.
10. Lai CC, Wang CY, Chu CC, Tan CK, Lu CL, Lee Y, et al. Correlation between antibiotic consumption and resistance of Gram-negative bacteria causing healthcare-associated infections at a university hospital in Taiwan from 2000 to 2009. J Antimicrob Chemother. 2011; 66:1374–1382. PMID: 21436153.
Fig. 1
Correlation of national aminoglycoside usage and gentamicin-resistance rates (%) of P. aeruginosa (GEN-R-PAE) isolated from general hospitals. Correlation of gentamicin usage and GEN-R-PAE (correlation coefficient r=0.83, P=0.0028); correlation of total aminoglycoside usage and GEN-R-PAE (r=0.92, P=0.0001).
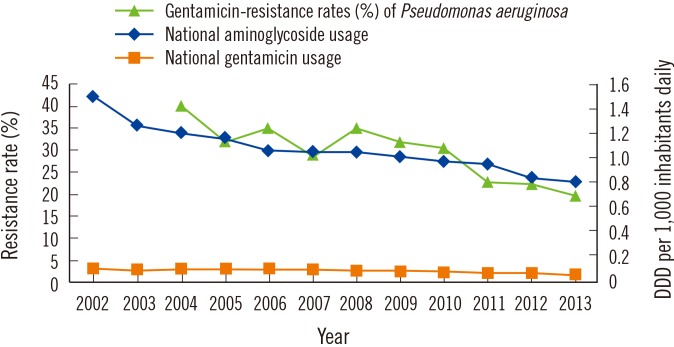
Fig. 2
Correlation of national amikacin usage and amikacin-resistance rates (%) of P. aeruginosa (AMK-R-PAE) isolated from general hospitals. Correlation of amikacin usage and AMK-R-PAE in the same year (correlation coefficient r=–0.11, P=0.8192); correlation of amikacin usage and AMK-R-PAE with 2-year interval (r=0.77, P=0.0145).





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download