Dear Editor,
Resistance of Candida species to azoles has increased in recent decades, and echinocandin resistance has emerged as a new problem in some species [1]. The global prevalence of echinocandin resistance in Candida ranges from 0 to 2.8%, but is very rare in C. albicans; moreover, fluconazole resistance was detected in only 0.4% of C. albicans samples, but in 11.9% and 11.6% of C. glabrata and C. tropicalis samples, respectively [2]. The emergence of echinocandin resistance in species with a high frequency of azole resistance raises the specter of a multidrug-resistant fungal pathogen, which appears to be the case for C. glabrata [1]. In Korea, up to 2.6% of Candida species show fluconazole resistance, with particularly high frequencies in C. glabrata and C. krusei; however, fluconazole-resistant C. albicans is rare [3].
Here, we report a case of multidrug-resistant C. albicans (resistant to fluconazole and echinocandins) isolated from the bloodstream of a 27-yr-old male patient with B cell acute lymphoblastic leukemia (B-ALL) who received allogenic stem cell transplantation (SCT). He took micafungin as a prophylactic antifungal treatment for over three weeks, followed by oral fluconazole for intermittent oral candidiasis. Six months after SCT, he was hospitalized owing to relapsed B-ALL and received re-induction chemotherapy. While on fluconazole for neutropenic fever and oral candidiasis, the antifungal agent was switched to caspofungin on hospital day 20 owing to a prolonged neutropenic fever, and was then switched to amphotericin B on day 46 after another fever developed.
Peripherally drawn blood cultures were obtained on day 74 when the patient's body temperature was 37.6℃. One of the two sets was positive for the growth of yeast, which was identified as C. albicans by the Vitek2 YST identification card system (bioMérieux, Marcy l'Etoile, France), representing the first C. albicans isolate from this patient.
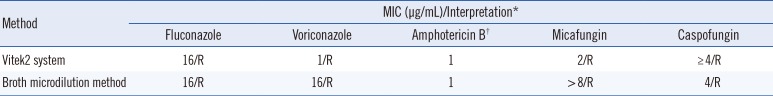
Antifungal susceptibility testing was performed by using the Vitek2 system and broth microdilution according to the CLSI guidelines [4]. The isolate was resistant to fluconazole, voriconazole, micafungin, and caspofungin (Table 1). For molecular confirmation of echinocandin resistance, the hot-spot regions of FKS1 were amplified and sequenced according to the previously outlined protocols [5]. The isolate had a homozygous T1933C mutation resulting in an S645P substitution, which was previously associated with micafungin treatment failure [5]. No specific mutation in ERG11, related to azole resistance, was detected.
Azole resistance can occur in C. albicans through diverse mechanisms such as overexpression of the multidrug transporter genes CDR1, CDR2, or MDR1, or by overexpression of ERG11, which encodes the azole target. The current patient received empirical caspofungin as of C. albicans isolation (day 76), but was then switched to amphotericin B on day 81 on the basis of the antifungal susceptibility test. Except for the initial isolation, follow-up blood cultures were all negative; however, the patient's general condition significantly worsened, and he died on day 88.
This is the first Korean case of echinocandin resistance in C. albicans, which was proven to have the FKS1 mutation. Echinocandins act by inhibiting β-1,3-D-glucan synthase, which synthesizes β-1,3-D-glucan of the fungal cell wall. Mutations of FKS genes (FKS1 and FKS2) encoding β-1,3-D-glucan synthase subunits lead to echinocandin resistance, and are detected in only 4% and <1% of C. glabrata and C. albicans isolates, respectively [6]. In Korea, Cho et al [7] reported an echinocandin-resistant C. glabrata isolate with an FKS mutation, but there has been no previous report of C. albicans with an FKS mutation.
Considering the extreme rarity of echinocandin resistance in C. albicans, our case suggests that immunocompromised patients, who are more likely to receive antifungal treatment as prophylaxis or for an invasive fungal infection, may have an increased risk of developing resistance. Recently, echinocandins have been used as first-line agents for the treatment of disseminated candidiasis and in antifungal prophylaxis [89]. Echinocandins resistance can lead to treatment failure for candidiasis, resulting in prolonged treatment periods, increased complications, and even higher mortality [16]. Although FKS mutations are uncommon among non-C. glabrata species, even with prior echinocandin exposure [6], clinicians should be aware of the potential for echinocandin resistance among patients with prior echinocandin exposure, especially those with breakthrough infections.
In conclusion, we report a case of breakthrough fungemia due to C. albicans with an FKS1 mutation in a patient with a hematologic malignancy. Clinicians should be aware of the possibility of breakthrough candidemia and echinocandin resistance in patients receiving echinocandin therapy. In such cases, an antifungal susceptibility test followed by molecular screening for FKS mutations would facilitate treatment decisions.
Acknowledgments
This research was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (NRF-2016R1A2B4008181).
References
1. Alexander BD, Johnson MD, Pfeiffer CD, Jiménez-Ortigosa C, Catania J, Booker R, et al. Increasing echinocandin resistance in Candida glabrata: clinical failure correlates with presence of FKS mutations and elevated minimum inhibitory concentrations. Clin Infect Dis. 2013; 56:1724–1732. PMID: 23487382.
2. Castanheira M, Messer SA, Rhomberg PR, Pfaller MA. Antifungal susceptibility patterns of a global collection of fungal isolates: results of the SENTRY Antifungal Surveillance Program (2013). Diagn Microbiol Infect Dis. 2016; 85:200–204. PMID: 27061369.
3. Jang MJ, Shin JH, Lee WG, Kim MN, Lee K, Lee HS, et al. In vitro fluconazole and voriconazole susceptibilities of Candida bloodstream isolates in Korea: use of the CLSI and EUCAST epidemiological cutoff values. Ann Lab Med. 2013; 33:167–173. PMID: 23667842.
4. Clinical and Laboratory Standards Institute. Reference method for broth dilution antifungal susceptibility testing of yeasts; Approved Standard. CLSI document M27-A3. Wayne, PA: Clinical and Laboratory Standards Institute 2008a;2008. 28:p. 6–12.
5. Slater JL, Howard SJ, Sharp A, Goodwin J, Gregson LM, Alastruey-Izquierdo A, et al. Disseminated Candidiasis caused by Candida albicans with amino acid substitutions in Fks1 at position Ser645 cannot be successfully treated with micafungin. Antimicrob Agents Chemother. 2011; 55:3075–3083. PMID: 21502627.
6. Shields RK, Nguyen MH, Press EG, Cumbie R, Driscoll E, Pasculle AW, et al. Rate of FKS mutations among consecutive Candida isolates causing bloodstream infection. Antimicrob Agents Chemother. 2015; 59:7465–7470. PMID: 26392494.
7. Cho EJ, Shin JH, Kim SH, Kim HK, Park JS, Sung H, et al. Emergence of multiple resistance profiles involving azoles, echinocandins and amphotericin B in Candida glabrata isolates from a neutropenia patient with prolonged fungaemia. J Antimicrob Chemother. 2015; 70:1268–1270. PMID: 25550394.
8. Pappas PG, Rex JH, Sobel JD, Filler SG, Dismukes WE, Walsh TJ, et al. Guidelines for treatment of candidiasis. Clin Infect Dis. 2004; 38:161–189. PMID: 14699449.
9. Maertens J, Marchetti O, Herbrecht R, Cornely OA, Flückiger U, Frêre P, et al. European guidelines for antifungal management in leukemia and hematopoietic stem cell transplant recipients: summary of the ECIL 3--2009 update. Bone Marrow Transplant. 2011; 46:709–718. PMID: 20661235.
10. Clinical and Laboratory Standards Institute. Reference method for broth dilution antifungal susceptibility testing of yeasts; Fourth Informational Supplement. CLSI document M27-S4. Wayne, PA: Clinical and Laboratory Standards Institute;2012.
Table 1
Drug susceptibilities of Candida albicans isolated in the present case
| Method | MIC (µg/mL)/Interpretation* | ||||
|---|---|---|---|---|---|
| Fluconazole | Voriconazole | Amphotericin B† | Micafungin | Caspofungin | |
| Vitek2 system | 16/R | 1/R | 1 | 2/R | ≥ 4/R |
| Broth microdilution method | 16/R | 16/R | 1 | > 8/R | 4/R |
*Interpretive criteria used were those published in CLSI document M27-S4 [10]; †No CLSI breakpoint is available.
Abbreviations: MIC, minimal inhibitory concentration; R, resistance.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download