Dear Editor,
Lipoprotein X (Lp-X) is a lamellar spherical particle rich in phospholipids and unesterified cholesterol. Although the pathogenesis of Lp-X formation is not fully understood in cholestasis, it is suggested that lipoprotein in bile refluxes into the plasma and binds to albumin forming Lp-X [1]. Lp-X is also found in familial lecithin cholesterol acyltransferase (LCAT) deficiency. Thus, it has been supposed that reduced LCAT activity, common in patients with a hepatocellular disease, contributes to Lp-X accumulation in cholestasis [2]. Serum Lp-X detection is a specific and sensitive index of cholestasis. Lp-X tests were positive in 82–100% of patients with histological evidence of cholestasis and negative in 95–98.7% of patients whose histological examination was negative [345]. Furthermore, Lp-X may play an important role in the development of hypercholesterolemia through failure to exert negative feedback on cholesterol synthesis [6]. Here, we report the first case in Korea that describes the presence of Lp-X in the serum of a patient with persistent hypercholesterolemia associated with bile obstruction.
A 71-yr-old woman, with a history of hypertension, diabetes, and Wegener's granulomatosis, was admitted to the hospital complaining of dyspnea. Approximately four months earlier, she had undergone endoscopic retrograde cholangiopancreatography for the removal of distal common bile duct stones developed owing to cholangiohepatitis.
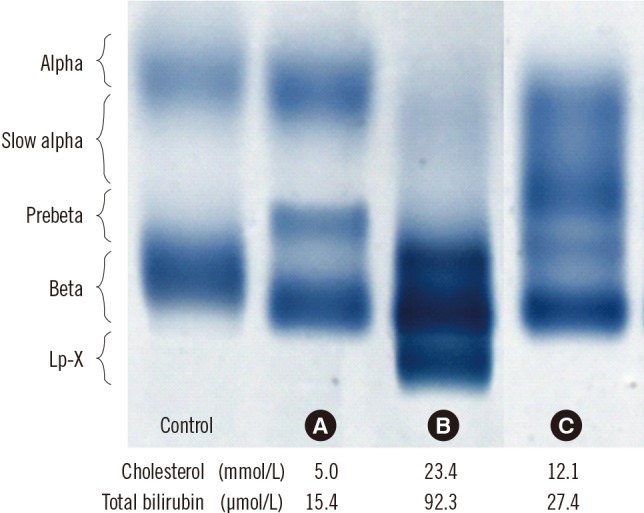
Radiological investigation showed newly developed ground glass opacity in both lungs. Initial laboratory findings suggested acute inflammation—white blood cells, 10.47×109/L; C-reactive protein, 82.8 mg/L (reference range<8.0). PCR result for Pneumocystis jirovecii using sputum sample was positive, and the patient was diagnosed as having P. jirovecii pneumonia. During antibiotic treatment, her pulmonary symptoms and elevated inflammation markers resolved gradually. However, her lipid profile and cholestatic markers were abnormal as given below: cholesterol, 13.8 mmol/L (3.7–6.2); LDL-cholesterol, 5.8 mmol/L (1.8–4.1); HDL-cholesterol, 1.5 mmol/L (1.0–1.9); triglyceride, 2.1 mmol/L (0.5–2.3); γ-glutamyltransferase 979 U/L, (7.0–35.0); total bilirubin, 80.4 µmol/L (6.8–25.7); alkaline phosphatase, 1,285 U/L (40–126). Abdominopelvic computed tomography revealed intrahepatic duct and common bile duct dilatation, suggesting unresolved cholestasis. The patient was on sulfamethoxazole/trimethoprim, teicoplanin, ranitidine hydrochloride, magnesium oxide, and calcium polycarbophil medication. Because her hypercholesterolemia was assumed to be secondary owing to cholestasis, lipoprotein was electrophoresed on agarose gel at pH 7.5 using an automated electrophoresis system Hydrasys (Sebia, Norcross, GA, USA), which showed the presence of Lp-X (Fig. 1) and indicated that the main etiology of hypercholesterolemia in this patient was cholestasis. After five months, her hypercholesterolemia was slightly improved, the total bilirubin level nearly normalized (1.6 mg/dL), the follow-up lipoprotein electrophoresis showed an absence of Lp-X, and the lipid profile was as follows: cholesterol, 12.1 mmol/L; LDL-cholesterol, 3.6 mmol/L; HDL-cholesterol, 2.2 mmol/L; triglyceride, 1.5 mmol/L. After one year, her cholesterol was further decreased to 7.2 mmol/L and other lipid profile parameters were also improved as follows: LDL-cholesterol, 3.0 mmol/L; HDL-cholesterol, 1.9 mmol/L; triglyceride, 0.7 mmol/L.
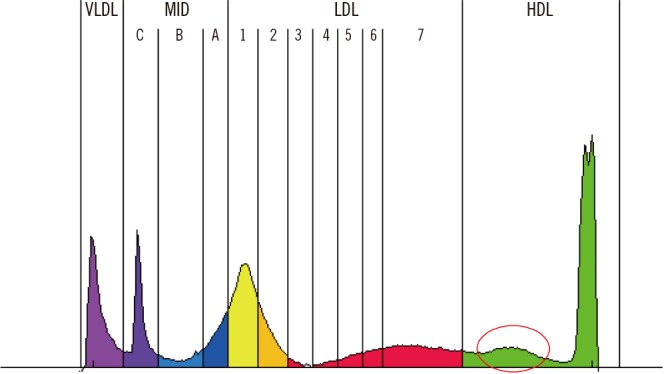
Lipoprotein electrophoresis also indicated the presence of slow alpha HDL (Fig. 1). This abnormal alpha band has been observed previously in cases of cholestasis with both increased and decreased HDL-cholesterol concentrations [78]. Slow alpha HDL has a particle size intermediate to that of normal LDL and HDL. In cholestasis, this change in HDL causes discrepancies in HDL levels measured by using various methods [9]. In this case, HDL-cholesterol level was 1.8 mmol/L at admission and gradually increased to 2.8 mmol/L at outpatient follow-up testing three months later. We performed LDL sub-fraction electrophoresis (Lipoprint LDL System; Quantimetrix, Redondo Beach, CA, USA), to identify and quantitatively score LDL components according to particle size, which showed an additional large, abnormal HDL sub-fraction that seemed to be slow alpha HDL and could be the main cause of the abnormally elevated HDL-cholesterol level in our patient (Fig. 2).
In addition, the patient was found to be hyponatremic (126 mmol/L). Pseudohyponatremia has been described in some patients with severe hypercholesterolemia secondary to increased Lp-X [10]. While severe hyperglycemia is known to also cause pseudohyponatremia, the patient's glucose level was 6.7 mmol/L (3.9–6.1). In this case, the sodium concentration was measured by an indirect ion-selective electrode method. Indirect methods may underestimate the sodium concentration because of the dilution artifacts in patients with hypercholesterolemia.
This is the first case report in Korea that describes the presence of Lp-X in the serum of a patient with persistent hypercholesterolemia associated with bile obstruction. The cholesterol level was normalized after improvement of cholestasis. Lp-X detection could be helpful in determining the cause of hypercholesterolemia in patients with cholestasis.
References
1. Manzato E, Fellin R, Baggio G, Walch S, Neubeck W, Seidel D. Formation of lipoprotein-X. Its relationship to bile compounds. J Clin Invest. 1976; 57:1248–1260. PMID: 816809.
2. Seidel D, Gjone E, Blomhoff JP, Geisen HP. Plasma lipoproteins in patients with familial plasma lecithin: cholesterol acyltransferase (LCAT) deficiency--studies on the apolipoprotein composition of isolated fractions with identification of LP-X. Horm Metab Res. 1974; (Suppl 4):6–11. PMID: 4371225.
3. Fellin R, Manzato E, Zotti S, Baggio G, Briani G, Rugge M. Lipoprotein-X and diagnosis of cholestasis: comparison with other biochemical parameters and liver biopsy. Clin Chim Acta. 1978; 85:41–47. PMID: 25728.
4. Fischer M, Falkensammer C, Barouch G, Wuketich S, Kromberger O, Schnack H. The diagnosis of cholestasis: lipoprotein X (LP-X) (author's transl). Wien Klin Wochenschr. 1975; 87:524–531. PMID: 5812.
5. Milewski B, Palynyczko Z. Significance of serum lipoproteid-X (LP-X) determination for the diagnosis of cholestasis in chronic liver diseases. Pol Med Sci Hist Bull. 1975; 15:551–555. PMID: 1228704.
6. Liersch M, Baggio G, Heuck CC, Seidel . Effect of lipoprotein-X on hepatic cholesterol synthesis. Atherosclerosis. 1977; 26:505–514. PMID: 193523.
7. Peynet J, Fénéant-Thibault M, Legrand A, Marot D, Rousselet F, Lemonnier A. Isolation and characterization of an abnormal alpha slow-moving high-density lipoprotein subfraction in serum from children with longstanding cholestasis. Clin Chem. 1986; 32:646–651. PMID: 3955813.
8. Miyahara K, Kasahara N, Kondo Y, Imai Y, Matuzaki F. Changes in plasma lipids and abnormal lipoproteins in a patient with drug-induced cholestatic hepatitis. Jpn J Med. 1991; 30:354–359. PMID: 1942649.
9. Kim S, Chun S, Lee W, Kim GS, Min WK. Cholestasis causes discrepancy in HDL-cholesterol levels measured using various methods. Lab Med Online. 2012; 2:174–178.
10. Sivakumar T, Chaidarun S, Lee HK, Cervinski M, Comi R. Multiple lipoprotein and electrolyte laboratory artifacts caused by lipoprotein X in obstructive biliary cholestasis secondary to pancreatic cancer. J Clin Lipidol. 2011; 5:324–328. PMID: 21784379.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download