Dear Editor,
Primary bone marrow lymphoma (PBML) is a rare disease, of which diffuse large B-cell lymphoma (DLBCL) is the most common pathological subtype [123]. While T-cell lymphomas are often associated with hemophagocytic lymphohistiocytosis (HLH), non-Hodgkin B-cell lymphomas are rarely observed in patients with HLH [4]. Moreover, fibrillar projections are an uncommon feature of DLBCL [56]. Herein, we report an extremely rare case of malignancy-associated HLH in which the underlying disease was a primary bone marrow (PBM) DLBCL with fibrillar projections.
A 57-yr-old man was admitted with a history of fever and 5-kg weight loss occurring over 1-month period. His physical examination was negative for both lymphadenopathy and a notably palpable spleen. Laboratory results indicated bicytopenia (leukocytes 4.8×109/L, hemoglobin 65 g/L, and platelets 68×109/L) and increased levels of ferritin (2,575 µg/L, reference interval [RI]: 20–320 µg/L), soluble CD25 (9,670 U/mL, RI: 124–466 U/mL), lactate dehydrogenase (LD; 309 IU/L, RI: 120–250 IU/L), and β2-microglobulin (5.0 mg/L, RI: 1.0–2.4 mg/L). Chest, neck, and abdominal-pelvic computational tomography showed mild splenomegaly, but were negative for other organomegaly. Fluorodeoxyglucose whole-body positron emission tomography revealed hypermetabolic bone marrow (BM) with expansion.
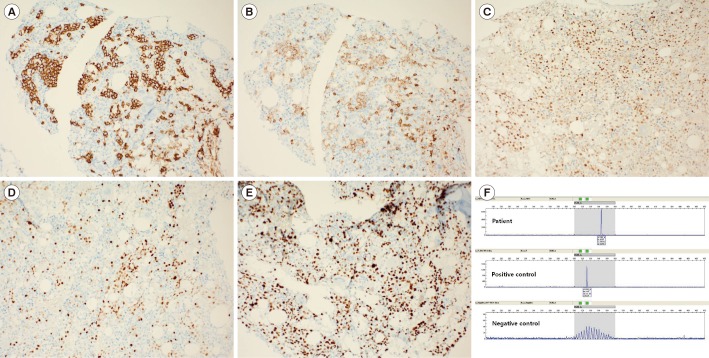
BM aspirate smears showed cells (65.4% of nucleated cells) with medium- to large-sized, round nuclei with one or more distinct nucleoli, and a moderate amount of basophilic cytoplasm. These cells had fibrillar projections and occurred in clusters; hemophagocytic histiocytes were frequently observed. A trephine biopsy showed nodular or interstitial aggregations of neoplastic cells with occasional scattered cells in small vessels and no evidence of trabecular bone destruction (Fig. 1). Karyotyping revealed hyperdiploidy and complex abnormalities; 53,XY,add(1)(p36.1),+3,add(7)(q22),+8,del(8)(p21)x2,+9,+17,der(17)del(17) (p13)add(17)(q24)x2,+18,+18,+mar[12]/45,X,-Y[4]/46,XY[4]. Flow cytometry analysis showed neoplastic cells that were CD19+, CD20+, CD22+, FMC7+, CD5+, CD2-, CD3-, CD7-, CD56-, CD10-, CD34-, and TdT-. Immunohistochemistry indicated positivity for CD20, CD5, IRF4/MUM-1, and BCL-6 and negativity for CD10, CD30, BCL-2, and cyclin D1. The Ki67 index was high (90%). In-situ hybridization for the Epstein-Barr virus did not identify infected cells. PCR assay was positive for the clonal rearrangement of the IGH gene (Fig. 2).
The patient's diagnosis was HLH associated with PBML, which was based on the criteria for defining PBML [2]. The patient's PBML had features highly suggestive of DLBCL. He was subsequently treated with four cycles of R-CHOP (cyclophosphamide, doxorubicin, vincristine, prednisone, and rituximab) chemotherapy. Following three months of chemotherapy, the patient's clinical manifestations had resolved. A follow-up BM examination showed a normal karyotype with no residual neoplastic cells or hemophagocytic histiocytes. The patient was alive at the time this letter was written on Jul 2017, 10 months post admission.
This case presents several noteworthy findings. First, the most plausible diagnosis was CD5-positive DLBCL, which is characterized by older age, elevated LD levels, occurrence at a greater number of extranodal sites, a higher frequency of B symptoms, and a more advanced stage at presentation compared with CD5-negative DLBCL. The most frequent site of extranodal involvement in CD5-positive DLBCL is the BM [7]. Although CD5 expression is observed in up to 10% of DLBCL patients [5], previous case series reported a significantly higher incidence (80%) in PBM DLBCL [1]. Indeed, CD5 positivity with accompanying hemophagocytosis is highly specific for intravascular large B-cell lymphoma (ILBCL) [5]. Although intravascular infiltration was minimal in this case, it might indicate an overlap between CD5-positive DLBCL and ILBCL. Second, the major cytogenetic abnormalities demonstrated in this case (trisomy 3, del[17p], and trisomy 18) are frequent abnormalities in DLBCL patients. Of note, two or more cytogenetic abnormalities have been associated with inferior overall survival compared with a normal karyotype or single abnormality, irrespective of histologic evidence of BM involvement [8]. Although most features of this case suggest a poor outcome, the patient showed good response to chemotherapy, at least, during the initial three months. Third, rare morphologic variants of DLBCL include the spindle cell variant, DLBCL with pseudorosettes, DLBCL with myxoid stroma, and DLBCL with fibrillar projections [5]. This case highlights neoplastic lymphocytes exhibiting fibrillar projections that can mimic some carcinomas and neurogenic tumors.
Our literature review found two recent cases of PBM DLBCL with hemophagocytosis, which are similar to the present case in that one showed CD5 positivity and minimal intravascular infiltration of neoplastic lymphocytes [9] and the other demonstrated a complex karyotype and a good initial response to chemotherapy [10]. Meticulous observation of BM aspirate smears and a detailed review, including immunophenotyping and chromosomal analysis, are essential for establishing an appropriate differential diagnosis, as well as minimizing the risk of misdiagnosis.
References
1. Chang H, Hung YS, Lin TL, Wang PN, Kuo MC, Tang TC, et al. Primary bone marrow diffuse large B cell lymphoma: a case series and review. Ann Hematol. 2011; 90:791–796. PMID: 21181164.
2. Martinez A, Ponzoni M, Agostinelli C, Hebeda KM, Matutes E, Peccatori J, et al. Primary bone marrow lymphoma: an uncommon extranodal presentation of aggressive non-hodgkin lymphomas. Am J Surg Pathol. 2012; 36:296–304. PMID: 22251943.
3. Bhagat P, Sachdeva MU, Sharma P, Naseem S, Ahluwalia J, Das R, et al. Primary bone marrow lymphoma is a rare neoplasm with poor outcome: case series from single tertiary care centre and review of literature. Hematol Oncol. 2016; 34:42–48. PMID: 25407700.
4. Rosado FG. Hemophagocytic lymphohistiocytosis: an update on diagnosis and pathogenesis. Am J Clin Pathol. 2013; 139:713–727. PMID: 23690113.
5. Gurbuxani S, Anastasi J, Hyjek E. Diffuse large B-cell lymphoma--more than a diffuse collection of large B cells: an entity in search of a meaningful classification. Arch Pathol Lab Med. 2009; 133:1121–1134. PMID: 19642739.
6. Dargent JL, Meiers I, Lespagnard L, Ma Y, Dehou MF, Verhest A. Diffuse large B-cell lymphoma with fibrillary matrix. Diagn Cytopathol. 2002; 27:223–226. PMID: 12357500.
7. Yamaguchi M, Seto M, Okamoto M, Ichinohasama R, Nakamura N, Yoshino T, et al. De novo CD5+ diffuse large B-cell lymphoma: a clinicopathologic study of 109 patients. Blood. 2002; 99:815–821. PMID: 11806981.
8. Kim S, Kim H, Kang H, Kim J, Eom H, Kim T, et al. Clinical significance of cytogenetic aberrations in bone marrow of patients with diffuse large B-cell lymphoma: prognostic significance and relevance to histologic involvement. J Hematol Oncol. 2013; 6:76. PMID: 24220305.
9. Bansal A, Mittal S, Dass J, Gupta N, Agarwal PK, Kotwal J. A case presenting with splenic infarct diagnosed as primary bone marrow CD5 positive DLBCL: a clinicopathological correlation. Indian J Hematol Blood Transfus. 2016; 32(S1):159–162. PMID: 27408381.
10. Park SH, Lee EY, Chung JS. A rare case of diffuse large B cell lymphoma-associated hemophagocytic syndrome initially present in the bone marrow with a favorable clinical course. Blood Res. 2016; 51:144–147. PMID: 27382563.
Fig. 1
Cyto- and histomorphology of bone marrow. (A) Bone marrow aspirate smear demonstrates clusters of neoplastic cells with fibrillar projections (red arrow). A histiocyte that has engulfed neutrophils and lymphocytes (green arrow) is also seen (Wright-Giemsa stain, ×1,000). (B) Bone marrow trephine biopsy specimen shows nodular infiltrates of neoplastic cells. No evidence of destruction of trabecular bone is seen (Hematoxylin & Eosin stain, ×200). A few neoplastic cells appear in a pattern of intrasinusoidal infiltration (right lower inset; immunostaining for CD34, ×400).
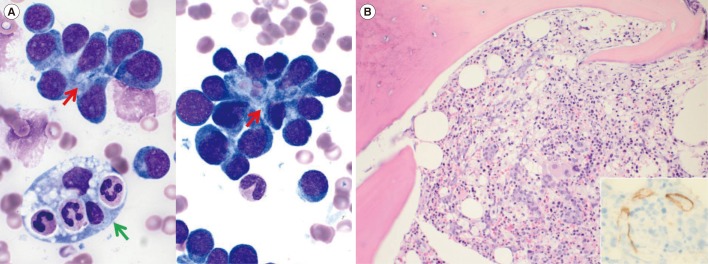
Fig. 2
Immunophenotyping and immunoglobulin heavy chain gene (IGH) clonality of the neoplastic cells. Neoplastic cells were positive for CD20 (A), CD5 (B), BCL6 (C), and IRF4/MUM1 (D) by immunostaining (×200). (E) The proliferative fraction of neoplastic cells as detected by Ki67 immunostaining was 90% (×200). (F) Neoplastic cells were positive for a clonal IGH rearrangement, which was consistent with the presence of a clonal B-cell population (IdentiClone IGH Gene Clonality Assay, Invivoscribe Technologies, Inc., San Diego, CA, USA).




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download