Abstract
Background
Methods
Results
Acknowledgments
References
SUPPLEMENTARY MATERIALS
Supplemental Table S2
Supplemental Table S3
Supplemental Table S4
Supplemental Table S5
Fig. 1
Thromboelastography results of (A) reaction time (R), (B) coagulation time (K), and (C) maximum amplitude (MA) and (D) thrombin generation assay results of endogenous thrombin potential (ETP) with respect to WHO bleeding grade. P values are assessed by using Kruskal-Wallis analysis for the comparison of WHO bleeding grades. * for P<0.05 and ** for P<0.005 are indicated above each box; the P values were obtained from the comparison of patients with WHO bleeding grades of 1 or ≥2 with those with WHO bleeding grade of 0 using Mann-Whitney U test with Bonferroni correction for multiple testing.
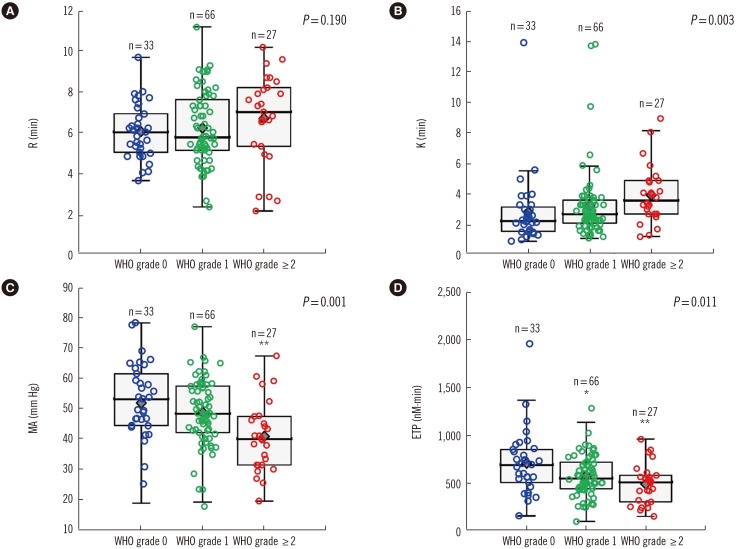
Fig. 2
ROC curve and the area under the ROC curve (AUC) for (A) maximum amplitude (MA), (B) MA based on various platelet levels, (C) endogenous thrombin potential (ETP), (D) ETP based on platelet levels, (E) MA and ETP, and (F) MA and ETP based on platelet levels used to predict high bleeding tendency (WHO bleeding grade ≥2).
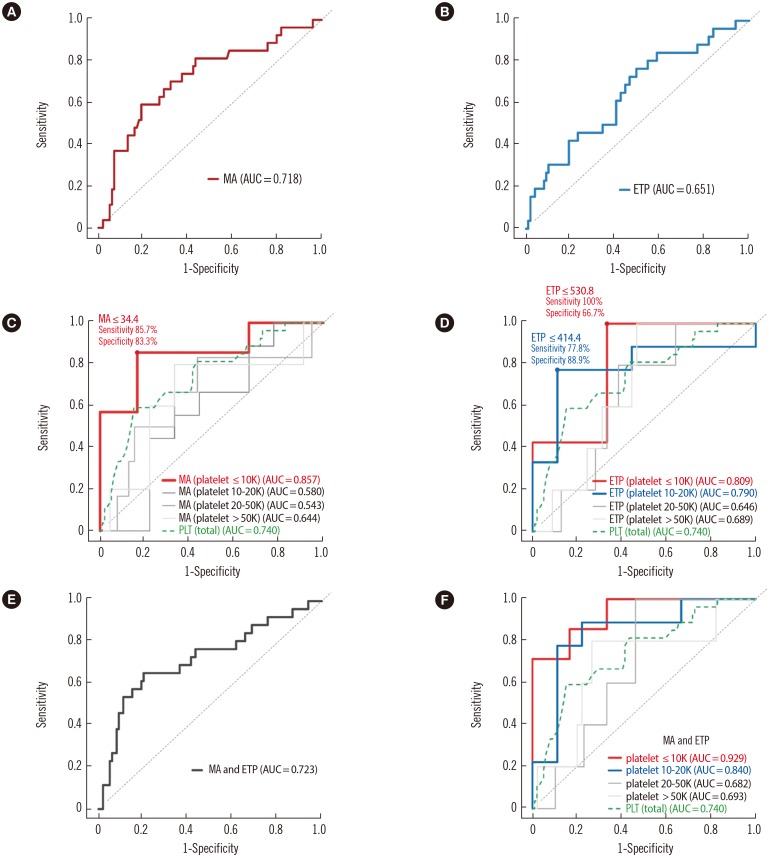
Table 1
Baseline population characteristics and laboratory results
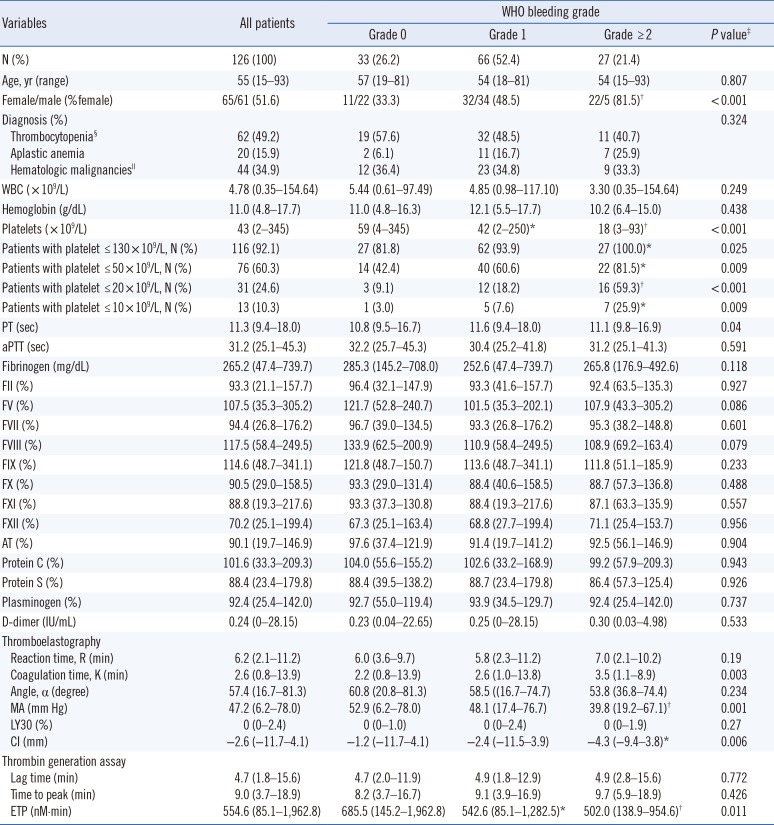
Most of the continuous variables did not show normal distributions except FX, AT and MA; therefore, continuous variables are presented as median (range) and number (percentage) for continuous and categorical variables, respectively.
*P<0.05; †P<0.005; P values were obtained from the comparison of patients with WHO bleeding grade of 1 or ≥2 with those with WHO bleeding grade of 0 by using Mann-Whitney U and χ2 test for quantitative and categorical variables, respectively, with Bonferroni correction for multiple testing; ‡P value: Kruskal-Wallis analysis for continuous variables; §Thrombocytopenia included immune thrombocytopenia (n=35) and thrombocytopenia due to peripheral consumption (n=27); ‖Hematologic malignancies included MDS (n=16), AML (n=16), ALL (n=4), and multiple myeloma (n=8).
Abbreviations: aPTT, activated partial thromboplastin time; AT, antithrombin; CI, coagulation index; ETP, endogenous thrombin potential; F, factor; MA, maximum amplitude; LY, lysis; PT, prothrombin time; WBC, white blood cell.
Table 2
Determinants of thromboelastography (TEG) and thrombin generation assay (TGA) parameters using multiple regression analysis in the total patient population (n=126)
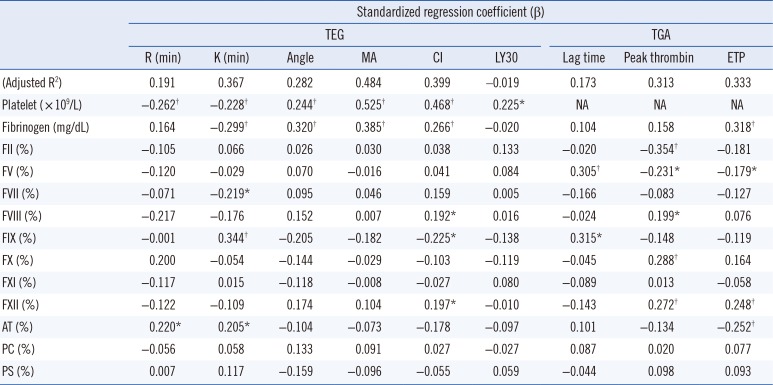
Data are presented as standardized regression coefficients (β).
*P<0.05; †P<0.01.
Abbreviations: AT, antithrombin; CI, coagulation index; ETP, endogenous thrombin potential; F, factor; K, coagulation time; Ly, lysis; MA, maximum amplitude; NA, not accessible; PC, protein C; PS, protein S; R, reaction time.
Table 3
Logistic regression analysis results of laboratory parameters for bleeding prediction
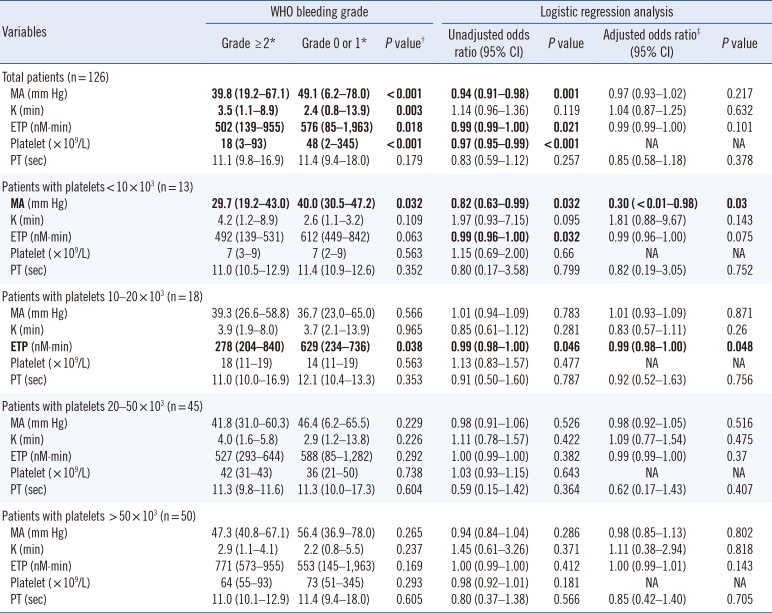
*Most of the continuous variables did not show normal distributions except MA, therefore, variables are presented as median (range); †P value: Mann-Whitney U test for results obtained from patients with WHO bleeding grade ≥2 or those with WHO bleeding grade of 0 or 1; ‡Platelet count was adjusted.
Abbreviations: CI, confidence interval; ETP, endogenous thrombin potential; MA, maximum amplitude; K, coagulation time; PT, prothrombin time.
Table 4
Diagnostic performance of laboratory parameters for the prediction of WHO bleeding grade ≥2
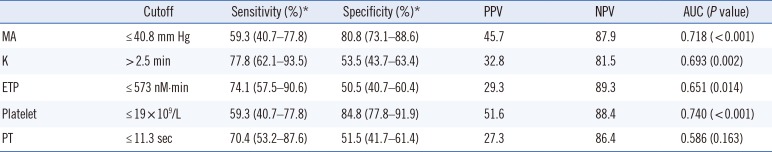
The cutoff values referred to the values producing the best diagnostic accuracy.
*Sensitivity and specificity are presented with 95% confidence intervals within the parenthesis.
Abbreviations: AUC, area under the concentration curve; ETP, endogenous thrombin potential; K, coagulation time; MA, maximum amplitude; NPV, negative predictive value; PPV, positive predictive value; PT, prothrombin time.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download