Dear Editor,
Early onset neonatal infections might be due to transmission from the maternal vaginal carriage of group B streptococcus (GBS) [1]. Urinary GBS suggests a heavy load of GBS [2]. Persistence of GBS in the urogenital area is not clearly understood and may cause recurrent infections. The aim of this study was to investigate how long GBS remains in the urogenital tract.
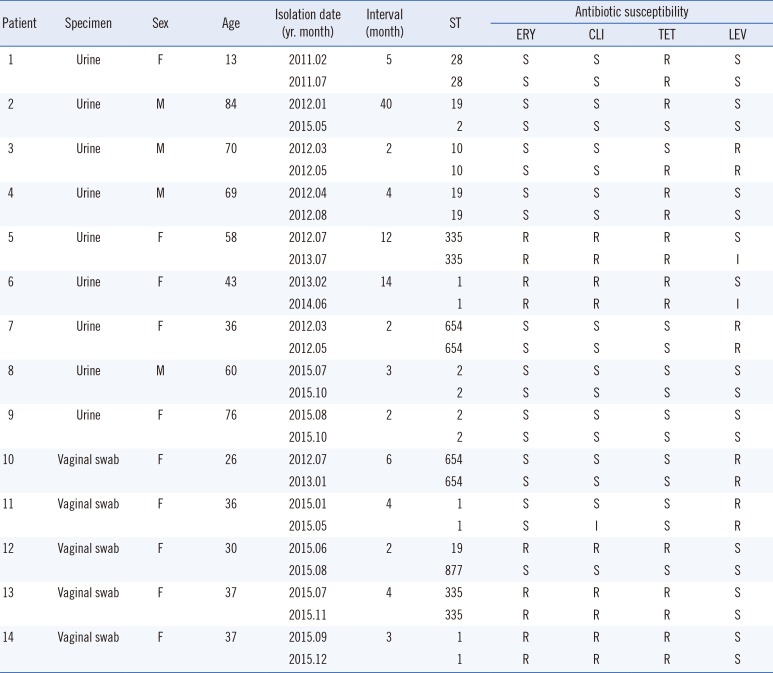
The study involved 14 patients whose urine (n=9) and vaginal swab (n=5) repeatedly tested positive for GBS throughout 2011–2015. The interval between the first and second isolation ranged from two to 40 months for urine and from two to six months for vaginal swabs. Intervals of less than two months were excluded. The vaginal swabs were taken from pregnant women for preterm screening of GBS. Bacterial identification and antimicrobial susceptibility test were performed by using the Vitek-2 system (bioMerieux Inc., Marcy l'Etoile, France).
Multilocus sequence typing (MLST) was performed according to previous reports for the collected isolates [3]. Briefly, bacterial DNA was extracted by using the GENEDIA Mycobacteria DNA Prep Kit (Green Cross Medical Science, Eumseng, Korea), and PCR was conducted for seven housekeeping genes with the AccuPower Taq PCR PreMix (Bioneer, Daejeon, Korea). DNA sequencing was performed at Macrogen Inc. (Seoul, Korea) using a dye-terminator method. Allocation of each allele and sequence type (ST) was assigned by using https://pubmlst.org/ [4]. This study was exempted from the approval by the institutional review board of Changwon Gyeongsang National University Hospital, Korea.
None of the isolates were resistant to ampicillin, penicillin-G, ceftriaxone, co-trimoxazole, linezolid, or vancomycin. Therefore, susceptibility to erythromycin, clindamycin, tetracycline, and levofloxacin was compared between the first and second isolations (Table 1). Of the isolates from the 14 patients, those of patients 2 and 3 showed a change in susceptibility to tetracycline, while those of patient 12 showed a change in susceptibility to erythromycin, clindamycin, and tetracycline.
Seven different STs were identified among the first isolates of the 14 patients. ST1 and ST19 were the most common (n=3), followed by ST2, ST335, ST654 (n=2), and ST10 and ST28 (n=1) (Table 1). Interestingly, only patients with ST19 exhibited different STs in their second specimen (patient 2, ST2 in the urine; patient 12, ST877 in the vaginal swab), whereas the other patients demonstrated the same ST. The allele combination of the seven housekeeping genes (adhP, pheS, atr, glnA, sdhA, glcK, and tkt) was 1-1-3-2-2-2-2 for ST19, 1-1-3-1-1-2-2 for ST2, and 166-1-2-1-1-2-2 for ST877. The interval of patient 2 was 40 months, and that of patient 12 was two months. The longest interval with the same ST was 14 months (patient 6) in urine and six months (patient 10) in the vaginal swab.
Recurrence of GBS colonization has been reported to be significantly higher during the subsequent pregnancies of women with prior GBS positivity (53%) than in controls (15%) [5], suggesting that GBS persists in the urogenital area for a few years. A previous study examining the dynamics of recto-vaginal GBS colonization during pregnancy by pulsed-field gel electrophoresis (PFGE) showed that genomic DNA was stable for repeated isolations from the same person throughout a 1.6-yr period; different genomic DNA was found between patients [6]. Twelve (85.7%) out of 14 patients showed the same STs in this study. This might be due to differences in study methodology: PFGE vs MLST. Another study monitoring ST genotypic diversity and serotype distribution pre- and post-delivery reported that a change of ST or serotype occurred in 18.3% (23/126) during a six-week period [6]. Although very few subjects participated in the current study, the frequency of ST change was 7.7% (1/13) within 14 months. Change of ST commonly occurred in ST1 (6/13) or ST23 (4/13) in a previous study [3], whereas in our study, it was observed in ST19. Therefore, certain STs may not be predisposed to change. As expected, different STs were identified after 40 months in urine (patient 2). In another study, 3/8 (37%) patients showed a different serotype between the urinary isolates in the first trimester and vaginal isolates in the third trimester [7].
In contrast to ST, the antibiogram did not provide complete discrimination. Although there was a change in susceptibility to tetracycline (S –> R, patient 3), the ST remained the same. Considering the difference in allocated alleles, different STs in the first and second specimens appear to be due to the acquisition of a new strain rather than the evolution of the previous type.
In conclusion, we observed that GBS may persist for at least 14 months in the urogenital tract. The frequency of change of the strain was 7.7% (1/13) during that period.
References
1. Melin P. Neonatal group B streptococcal disease: from pathogenesis to preventive strategies. Clin Microbiol Infect. 2011; 17:1294–1303. PMID: 21672083.
2. Ulett KB, Benjamin WH Jr, Zhuo F, Xiao M, Kong F, Gilbert GL, et al. Diversity of group B streptococcus serotypes causing urinary tract infection in adults. J Clin Microbiol. 2009; 47:2055–2060. PMID: 19439533.
3. Public database for molecular typing and microbial genome diversity (PubMLST), Streptococcus agalactiae (group B streptococcus, GBS) MLST databases. Updated in May 2017. http://www.pubmlst.org/sagalactiae/.
4. Turrentine MA, Ramirez MM. Recurrence of group B streptococci colonization in subsequent pregnancy. Obstet Gynecol. 2008; 112:259–264. PMID: 18669720.
5. Hansen SM, Uldbjerg N, Kilian M, Sørensen UB. Dynamics of Streptococcus agalactiae colonization in women during and after pregnancy and in their infants. J Clin Microbiol. 2004; 42:83. PMID: 14715736.
6. Manning SD, Lewis MA, Springman AC, Lehotzky E, Whittam TS, Davies HD. Genotypic diversity and serotype distribution of group B streptococcus isolated from women before and after delivery. Clin Infect Dis. 2008; 46:1829–1837. PMID: 18462173.
7. McKenna DS, Matson S, Northern I. Maternal group B streptococcal (GBS) genital tract colonization at term in women who have asymptomatic GBS bacteriuria. Infect Dis Obstet Gynecol. 2003; 11:203–207. PMID: 15108866.
Table 1
Isolation interval, sequence type (ST), and antibiogram of repeatedly isolated group B streptococci in urine and vaginal swabs




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download