1. Tzouvelekis LS, Markogiannakis A, Psichogiou M, Tassios PT, Daikos GL. Carbapenemases in
Klebsiella pneumoniae and other Enterobacteriaceae: an evolving crisis of global dimensions. Clin Microbiol Rev. 2012; 25:682–707. PMID:
23034326.
2. Queenan AM, Bush K. Carbapenemases: the versatile β-lactamases. Clin Microbiol Rev. 2007; 20:440–458. PMID:
17630334.
3. Yigit H, Queenan AM, Anderson GJ, Domenech-Sanchez A, Biddle JW, Steward CD, et al. Novel carbapenem-hydrolyzing β-lactamase, KPC-1, from a carbapenem-resistant strain of
Klebsiella pneumoniae. Antimicrob Agents Chemother. 2001; 45:1151–1161. PMID:
11257029.
4. Nordmann P, Naas T, Poirel L. Global spread of Carbapenemase-producing Enterobacteriaceae. Emerg Infect Dis. 2011; 17:1791–1798. PMID:
22000347.
5. Poirel L, Héritier C, Tolün V, Nordmann P. Emergence of oxacillinase-mediated resistance to imipenem in
Klebsiella pneumoniae. Antimicrob Agents Chemother. 2004; 48:15–22. PMID:
14693513.
6. Poirel L, Potron A, Nordmann P. OXA-48-like carbapenemases: the phantom menace. J Antimicrob Chemother. 2012; 67:1597–1606. PMID:
22499996.
7. Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing. Twenty-fourth Informational supplement, M100-S24. Wayne, PA: Clinical and Laboratory Standards Institute;2014.
8. Poirel L, Walsh TR, Cuvillier V, Nordman P. Multiplex PCR for detection of acquired carbapenemase genes. Diagn Microbiol Infect Dis. 2011; 70:119–123. PMID:
21398074.
9. Ryoo NH, Kim EC, Hong SG, Park YJ, Lee K, Bae IK, et al. Dissemination of SHV-12 and CTX-M-type extended-spectrum β-lactamases among clinical isolates of
Escherichia coli and
Klebsiella pneumoniae and emergence of GES-3 in Korea. J Antimicrob Chemother. 2005; 56:698–702. PMID:
16141280.
10. Pérez-Pérez FJ, Hanson ND. Detection of plasmid-mediated AmpC β-lactamase genes in clinical isolates by using multiplex PCR. J Clin Microbiol. 2002; 40:2153–2162. PMID:
12037080.
11. Korea Centers for Disease Control and Prevention. Korean Antimicrobial Resistance Monitoring System (KARMS) annual report, 2014. Korea Centers for Disease Control and Prevention;2015.
12. Centers for Disease Control and Prevention. Vital signs: carbapenem-resistant Enterobacteriaceae. MMWR Morb Mortal Wkly Rep. 2013; 62:165–170. PMID:
23466435.
13. Pollett S, Miller S, Hindler J, Uslan D, Carvalho M, Humphries RM. Phenotypic and molecular characteristics of carbapenem-resistant
Enterobacteriaceae in a health care system in Los Angeles, California, from 2011-2013. J Clin Microbiol. 2014; 52:4003–4009. PMID:
25210072.
14. Tseng IL, Liu YM, Wang SJ, Yeh HY, Hsieh CL, Lu HL, et al. Emergence of carbapenemase producing
Klebsiella pneumoniae and spread of KPC-2 and KPC-17 in Taiwan: a nationwide study from 2011 to 2013. PLoS One. 2015; 10:e0138471. PMID:
26384242.
15. Kim MN, Yong D, An D, Chung HS, Woo JH, Lee K, et al. Nosocomial clustering of NDM-1-producing
Klebsiella pneumoniae sequence type 340 strains in four patients at a South Korean tertiary care hospital. J Clin Microbiol. 2012; 50:1433–1436. PMID:
22259206.
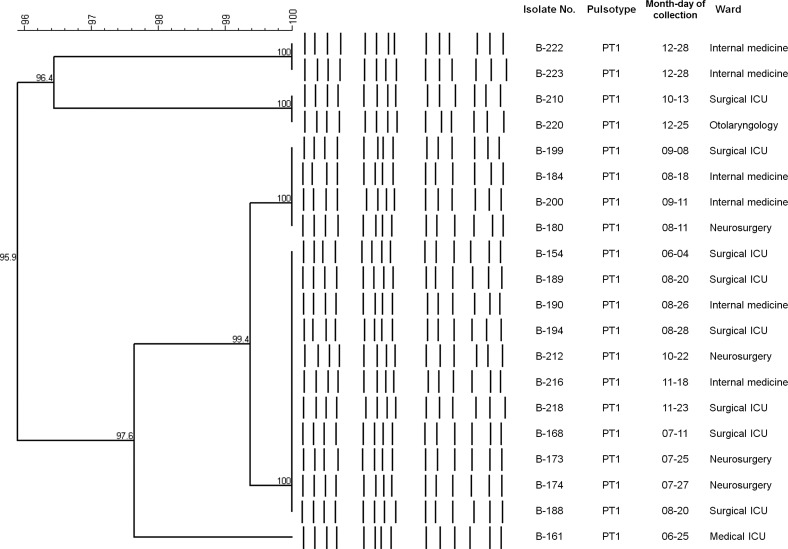
16. Hong SK, Yong D, Kim K, Hong SS, Hong SG, Khosbayar T, et al. First outbreak of KPC-2-producing
Klebsiella pneumoniae sequence type 258 in a hospital in South Korea. J Clin Microbiol. 2013; 51:3877–3879. PMID:
24006005.
17. Jeong SH, Lee KM, Lee J, Bae IK, Kim JS, Kim HS, et al. Clonal and horizontal spread of the
blaOXA-232 gene among Enterobacteriaceae in a Korean hospital. Diagn Microbiol Infect Dis. 2015; 82:70–72. PMID:
25702524.
18. Lefebvre B, Lévesque S, Bourgault AM, Mulvey MR, Mataseje L, Boyd D, et al. Carbapenem non-susceptible Enterobacteriaceae in Quebec, Canada: results of a laboratory surveillance program (2010-2012). PLoS One. 2015; 10:e0125076. PMID:
25910041.
19. Brañas P, Villa J, Viedma E, Mingorance J, Orellana MA, Chaves F. Molecular epidemiology of carbapenemase-producing
Klebsiella pneumoniae in a hospital in Madrid: Successful establishment of an OXA-48 ST11 clone. Int J Antimicrob Agents. 2015; 46:111–116. PMID:
25914088.
20. Docquier JD, Calderone V, De Luca F, Benvenuti M, Giuliani F, Bellucci L, et al. Crystal structure of the OXA-48 β-lactamase reveals mechanistic diversity among class D carbapenemases. Chem Biol. 2009; 16:540–547. PMID:
19477418.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download