1. Paya CV. Prevention of cytomegalovirus disease in recipients of solid-organ transplants. Clin Infect Dis. 2001; 32:596–603. PMID:
11181123.
2. Boeckh M, Boivin G. Quantitation of cytomegalovirus: methodologic aspects and clinical applications. Clin Microbiol Rev. 1998; 11:533–554. PMID:
9665982.

3. Allice T, Cerutti F, Pittaluga F, Varetto S, Franchello A, Salizzoni M, et al. Evaluation of a novel real-time PCR system for cytomegalovirus DNA quantitation on whole blood and correlation with pp65-antigen test in guiding pre-emptive antiviral treatment. J Virol Methods. 2008; 148:9–16. PMID:
18045702.

4. Guiver M, Fox AJ, Mutton K, Mogulkoc N, Egan J. Evaluation of CMV viral load using TaqMan CMV quantitative PCR and comparison with CMV antigenemia in heart and lung transplant recipients. Transplantation. 2001; 71:1609–1615. PMID:
11435973.

5. Camargo LF, Uip DE, Simpson AA, Caballero O, Stolf NA, Vilas-Boas LS, et al. Comparison between antigenemia and a quantitative-competitive polymerase chain reaction for the diagnosis of cytomegalovirus infection after heart transplantation. Transplantation. 2001; 71:412–417. PMID:
11233903.
6. Heid CA, Stevens J, Livak KJ, Williams PM. Realtime quantitative PCR. Genome Res. 1996; 6:986–994. PMID:
8908518.
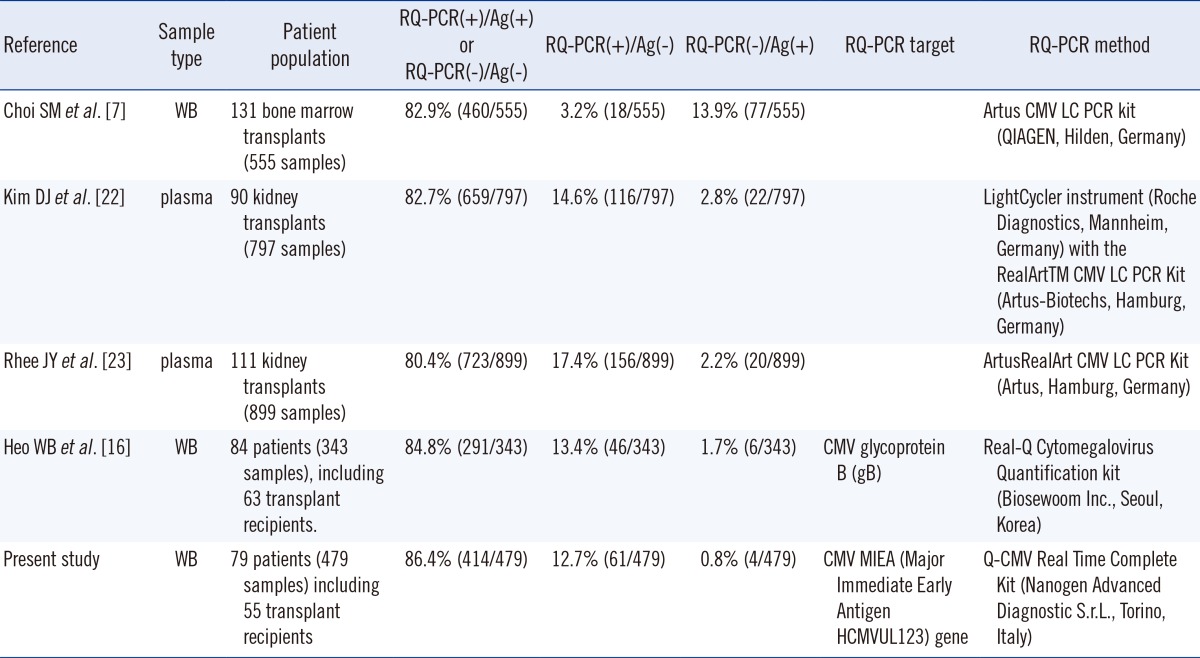
7. Choi SM, Lee DG, Lim J, Park SH, Choi JH, Yoo JH, et al. Comparison of quantitative cytomegalovirus real-time PCR in whole blood and pp65 antigenemia assay: clinical utility of CMV real-time PCR in hematopoietic stem cell transplant recipients. J Korean Med Sci. 2009; 24:571–578. PMID:
19654935.

8. Marchetti S, Santangelo R, Manzara S, D'onghia S, Fadda G, Cattani P. Comparison of real-time PCR and pp65 antigen assays for monitoring the development of Cytomegalovirus disease in recipients of solid organ and bone marrow transplants. New Microbiol. 2011; 34:157–164. PMID:
21617827.
9. Ljungman P, Griffiths P, Paya C. Definitions of cytomegalovirus infection and disease in transplant recipients. Clin Infect Dis. 2002; 34:1094–1097. PMID:
11914998.

10. Paya CV, Wilson JA, Espy MJ, Sia IG, DeBernardi MJ, Smith TF, et al. Preemptive use of oral ganciclovir to prevent cytomegalovirus infection in liver transplant patients: a randomized, placebo-controlled trial. J Infect Dis. 2002; 185:854–860. PMID:
11920308.

11. Kotton CN, Kumar D, Caliendo AM, Asberg A, Chou S, Danziger-Isakov L, et al. Updated international consensus guidelines on the management of cytomegalovirus in solid-organ transplantation. Transplantation. 2013; 96:333–360. PMID:
23896556.

12. Griffiths PD, Whitley RJ, editors. Recommendations from the International Herpes Management Forum (IHMF) Managements Strategies Workshop and 8th Annual Meeting of the IHMF. The challenge of CMV infection and disease in transplantation. UK: Cambridge Medical Publications;2000.
13. Lilleri D, Baldanti F, Gatti M, Rovida F, Dossena L, De Grazia S, et al. Clinically-based determination of safe DNAemia cutoff levels for preemptive therapy or human cytomegalovirus infections in solid organ and hematopoietic stem cell transplant recipients. J Med Virol. 2004; 73:412–418. PMID:
15170637.

14. Razonable RR, Brown RA, Wilson J, Groettum C, Kremers W, Espy M, et al. The clinical use of various blood compartments for cytomegalovirus (CMV) DNA quantitation in transplant recipients with CMV disease. Transplantation. 2002; 73:968–973. PMID:
11923702.

15. Von Müller L, Hampl W, Hinz J, Meisel H, Reip A, Engelmann E, et al. High variability between results of different in-house tests for cytomegalovirus (CMV) monitoring and a standardized quantitative plasma CMV PCR assay. J Clin Microbiol. 2002; 40:2285–2287. PMID:
12037112.

16. Heo WB, Won DI, Kim YL, Kim MH, Oh HB, Suh JS. Evaluation of Biosewoom Real-Q Cytomegalovirus Quantification kit for Cytomegalovirus viral load measure. Korean J Lab Med. 2007; 27:298–304. PMID:
18094592.
17. Li H, Dummer JS, Estes WR, Meng S, Wright PF, Tang YW. Measurement of human cytomegalovirus loads by quantitative real-time PCR for monitoring clinical intervention in transplant recipients. J Clin Microbiol. 2003; 41:187–191. PMID:
12517846.

18. Kalpoe JS, Kroes AC, de Jong MD, Schinkel J, de Brouwer CS, Beersma MF, et al. Validation of clinical application of cytomegalovirus plasma DNA load measurement and definition of treatment criteria by analysis of correlation to antigen detection. J Clin Microbiol. 2004; 42:1498–1504. PMID:
15070995.

19. Mhiri L, Kaabi B, Houimel M, Arrouji Z, Slim A. Comparison of pp65 antigenemia, quantitative PCR and DNA hybrid capture for detection of cytomegalovirus in transplant recipients and AIDS patients. J Virol Methods. 2007; 143:23–28. PMID:
17336402.

20. Ghaffari SH, Obeidi N, Dehghan M, Alimoghaddam K, Gharehbaghian A, Ghavamzadeh A. Monitoring of cytomegalovirus reactivation in bone marrow transplant recipients by real-time PCR. Pathol Oncol Res. 2008; 14:399–409. PMID:
18392952.

21. Pillet S, Roblin X, Cornillon J, Mariat C, Pozzetto B. Quantification of cytomegalovirus viral load. Expert Rev Anti Infect Ther. 2014; 12:193–210. PMID:
24341395.

22. Kim DJ, Kim SJ, Park J, Choi GS, Lee S, Kwon CD, et al. Real-time PCR assay compared with antigenemia assay for detecting cytomegalovirus infection in kidney transplant recipients. Transplant Proc. 2007; 39:1458–1460. PMID:
17580161.

23. Rhee JY, Peck KR, Lee NY, Song JH. Clinical usefulness of plasma quantitative polymerase chain reaction assay: diagnosis of cytomegalovirus infection in kidney transplant recipients. Transplant Proc. 2011; 43:2624–2629. PMID:
21911135.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download