Abstract
High-resolution imaging techniques have increased the detection rate of adrenal incidentaloma. We developed a method of liquid chromatography-tandem mass spectrometry (LC-MS/MS) for detection of plasma free metanephrine (MN) and normetanephrine (NMN) and evaluated its analytical performance and clinical efficacy in differential diagnosis of adrenal incidentaloma. After solid-phase extraction, chromatographic isolation of the analytes and internal standard was achieved by column elution in the LC-MS/MS system. The analytes were detected in multiple-reaction monitoring mode by using positive electrospray ionization: MN, transition m/z 180.1→165.1; NMN, m/z 166.1→134.1. This method was validated for linearity, precision, accuracy, lower limits of quantification and detection, extraction recovery, and the matrix effect. Plasma concentrations of MN and NMN of 14 patients with pheochromocytoma were compared with those of 17 healthy volunteers, 10 patients with essential hypertension, and 60 patients with adrenal adenoma. The assay's linear range was 0.04-50.0 and 0.08-100.0 nmol/L for MN and NMN, respectively. Assay imprecision was 1.86-7.50%. The accuracy ranged from -7.50% to 2.00%, and the mean recovery of MN and NMN was within the range 71.5-95.2%. Our LC-MS/MS method is rapid, accurate, and reliable and useful for differential diagnosis of adrenal incidentaloma.
Pheochromocytoma is a rare tumor arising from chromaffin cells of the adrenal medulla or in the paraganglia that produce excessive amounts of catecholamines [12]. Because of widespread use of imaging methods, adrenal incidentalomas have become an important clinical entity where a diagnosis of pheochromocytoma must be considered [3].
Because catecholamines are metabolized within chromaffin cells to metanephrine (MN) or normetanephrine (NMN), these metabolites can be used to diagnose pheochromocytoma. Furthermore, assays of MN and NMN in plasma or urine have better diagnostic sensitivity than measurements of the parent catecholamines; therefore, determination of plasma or urine MN and NMN is recommended over other biochemical indices [34567].
MN and NMN in urine are usually measured after acid hydrolysis, which converts high concentrations of sulfate-conjugated metabolites into free MN and NMN. During this process, concentrations of MN and NMN in urine become higher than those of free MN and NMN in plasma. These higher concentrations make urinary MN and NMN easier to measure than free MN and NMN in plasma. Nonetheless, the enzyme involved in sulfate conjugation is present in gastrointestinal tissues. Thus, plasma free MN and NMN provides the most direct and accurate test for the diagnosis of pheochromocytoma [8].
The use of plasma as the specimen is convenient, comfortable for patients, and provides high sensitivity for disease detection. In addition, the influence of diet and sympathoadrenal function are easier to be controlled [3910]. However, measurement of plasma free MN and NMN is challenging from an analytical standpoint because these compounds are present at low concentrations in a complex matrix and lack unique chemical characteristics [11]. Several laboratory assays of plasma free MN and NMN have been developed. Liquid chromatography-tandem mass spectrometry (LC-MS/MS) appears superior to HPLC in terms of both sensitivity and sample throughput [1112]. We describe a LC-MS/MS method for quantification of plasma free MN and NMN for the first time in Korea. In addition, we evaluated the analytical performance and clinical utility of MN and NMN measurement.
MN and NMN were purchased from Sigma-Aldrich (St. Louis, MO, USA). d3-Metanephrine-HCl (d3-MN-HCl) and d3-normetanephrine-HCl (d3-NMN-HCl) were purchased from CDN isotopes (Pointe-Claire, Quebec, Canada). HPLC-grade acetonitrile, methanol, and distilled water (DW) were purchased from Burdick & Jackson (Muskegon, MI, USA). Formic acid and ammonium formate were purchased from Sigma-Aldrich, and Strata CW-X extraction cartridges were purchased from Phenomenex (Torrance, CA, USA).
We prepared stock solutions of 20 mmol/L MN and NMN and a stock solution of the internal standard (IS) containing 1 mg/mL each of d3-MN-HCl and d3-NMN-HCl in methanol. These solutions were stored at -70℃. We diluted the stock solutions in methanol to prepare calibrator and working IS solutions. Calibrators were prepared with five concentrations of each analyte (0.04, 0.4, 2.0, 10.0, and 50.0 nmol/L for MN and 0.08, 0.8, 4.0, 20.0, and 100.0 nmol/L for NMN) and were stored at -70℃ until use. Quality control (QC) samples were purchased from Chromsystems (Gräfelfing, Germany). All plasma samples were extracted with the solid-phase extraction (SPE) method. SPE was performed using Strata CW-X extraction cartridges, pretreated with 1 mL methanol and 1 mL DW. After transferring the mixture of 500 µL the plasma with 1 mL DW and 5 µL working IS to the cartridge, the cartridge was sequentially washed with 1 mL ammonium formate (100 mmol/L), 1 mL DW, and 1.5 mL methanol. The analytes were eluted with 5% formic acid in methanol and were evaporated and reconstituted in 100 µL of 0.1% formic acid. Three microliters of the reconstituted eluate was injected into the LC-MS/MS system.
Analyses were performed on an Agilent 6490 tandem mass spectrometer equipped with an Agilent 1260 HPLC system (Agilent Technologies, Santa Clara, CA, USA). The chromatographic separation of MN and NMN was conducted on a Unison UK C18 column (Imtackt, Portland, OR, USA; 2.0×100 mm, 3.0 µm). The mobile phase was composed of DW containing 0.1% formic acid (mobile A) and acetonitrile containing 0.1% formic acid (mobile B). The following gradients were applied to the column: 0 min, 99% A and 1% B; 0.5 min, 99% A and 1% B; 1.5 min, 20% A and 80% B; 2.5 min, 20% A and 80% B; and 2.6 min, 99% A and 1% B. The total run time was 5 min, and the flow rate was 300 µL/min. The MS/MS system was equipped with an electrospray ionization (ESI) source operated in positive-ion detection mode. Nitrogen gas was used for nebulation, desolvation, and collision. The analytes were monitored in multiple-reaction monitoring (MRM) mode. The transitions of precursor ions to product ions (m/z 180.1→165.1, m/z 166.1→134.1, m/z 183.1→168.1, and m/z 169.0→137.1) were monitored for MN, NMN, d3-MN, and d3-NMN, respectively, with dwell time of 50 msec for each. Other settings for the mass spectrometer were as follows: gas flow 12 L/min at 150℃, nebulizer pressure 413.7 kPa, sheath gas flow 12 L/min at 400℃, capillary voltage 3,000 V, and collision energy 15 V. Quantification was performed using the ratio of the integrated peak area of MN and NMN to that of IS and was calculated with MassHunter Workstation software (version B.06, Agilent Technologies).
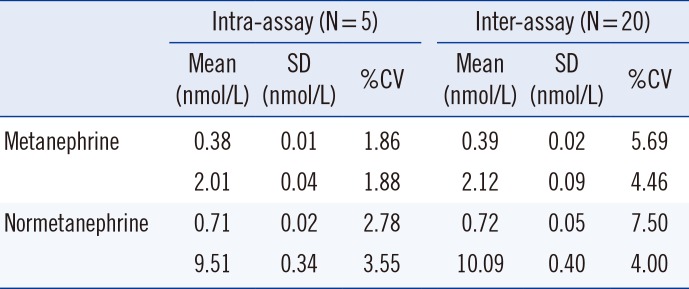
We plotted the ratios of the analyte peak area to the IS peak area at five concentrations from 0.04 to 50.0 nmol/L for MN and from 0.08 to 100.0 nmol/L for NMN. The linearity of the response was assessed by means of least-squares linear regression. Intra-assay imprecision was assessed by using five replicates in a single series, and interassay imprecision was evaluated by using 20 separate assays over 20 days, with two concentrations of QC samples. Accuracy was assessed by adding MN and NMN to charcoal-stripped serum at three concentrations (0.2, 1.0, and 10.0 nmol/L for MN and 0.4, 2.0, and 20.0 nmol/L for NMN), with five replicates. The lower limit of quantification and the lower limit of detection were tested by using bovine serum albumin spiked with MN and NMN. The extraction recovery of MN and NMN was determined at two concentrations (0.4 and 2.0 nmol/L for MN and 0.8 and 4.0 nmol/L for NMN), and the recovery of the IS was also evaluated. We assessed the matrix effect (ME) by comparing the peak area of the standards added to the mobile phase (A) with the peak area for the same amount of standards added to the preextracted samples (B): ME%=B/A×100 [13]. The validation data were analyzed in Excel 2010 (Microsoft, Redmond, WA, USA) and EP Evaluator Release 10 (Data Innovations, South Burlington, VT, USA).
Typical chromatograms of plasma MN and NMN from the LC-MS/MS analysis are shown in Fig. 1. The calibration curve yielded a linear response from 0.04 to 50.0 nmol/L for MN and from 0.08 to 100.0 nmol/L for NMN, with the corresponding correlation coefficient (r2) consistently >0.99 for both MN and NMN. Intra-assay CVs (n=5) were 1.86-1.88% for MN and 2.78-3.55% for NMN. Interassay CVs (n=20) were 4.46-5.69% for MN and 4.00-7.50% for NMN (Table 1). The method showed good accuracy with less than 10% of bias (-4.80% to 2.00% for MN and -7.50% to -2.25% for NMN). The lower limit of quantification was 0.04 nmol/L for MN and 0.08 nmol/L for NMN (n=5, CV of 5.1% and 9.0%, respectively). The lower limit of detection was 0.008 nmol/L for MN and 0.016 nmol/L for NMN. Recovery ranged from 94.6% to 95.2% for MN and from 71.5% to 80.6% for NMN at low and medium concentrations. A significant ME was not observed (mean values of ME were 89.9% and 90.1% for MN and NMN, respectively).
To evaluate clinical usefulness of the method, we retrospectively analyzed plasma MN and NMN concentrations of 14 patients with histologically proven pheochromocytoma, 60 patients with adrenal adenoma, 10 patients with essential hypertension, and 17 healthy normotensive volunteers. This study was approved by the Institutional Review Board of Samsung Medical Center, Seoul, Korea. We used upper cutoff levels for MN (0.50 nmol/L) and NMN (0.90 nmol/L) in plasma according to the data of the Mayo Clinic [512]. Fig. 2 shows the distribution of MN and NMN concentrations according to the dot-box and whisker plots constructed in MedCalc, version 12.5 (MedCalc Software, Mariakerke, Belgium). Among the patients with pheochromocytoma, plasma MN concentrations ranged from 0.04 to 10.09 nmol/L (median 0.52 nmol/L), and NMN concentrations ranged from 0.52 to 17.68 nmol/L (median 3.43 nmol/L). All patients with pheochromocytoma showed an increase above the upper cutoff level of at least one of the two analytes (100% diagnostic sensitivity). Although none of the patients with essential hypertension and none of the healthy volunteers showed elevated plasma levels of MN, one healthy volunteer and one patient with adrenal adenoma had slightly increased plasma NMN concentrations (97.7% diagnostic specificity).
In summary, we developed and validated a rapid, accurate, and reliable method for quantification of plasma MN and NMN using LC-MS/MS. With successful incorporation into routine operations in the clinical setting, this method can be useful for the initial diagnosis of pheochromocytoma.
Acknowledgments
This research was supported by a grant of Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number:HI13C2098).
References
1. Bravo EL. Evolving concepts in the pathophysiology, diagnosis, and treatment of pheochromocytoma. Endocr Rev. 1994; 15:356–368. PMID: 8076587.

2. Plouin PF, Gimenez-Roqueplo AP. Pheochromocytomas and secreting paragangliomas. Orphanet J Rare Dis. 2006; 1:49. PMID: 17156452.

3. Pacak K, Eisenhofer G, Ahlman H, Bornstein SR, Gimenez-Roqueplo AP, Grossman AB, et al. Pheochromocytoma: recommendations for clinical practice from the First International Symposium. October 2005. Nat Clin Pract Endocrinol Metab. 2007; 3:92–102. PMID: 17237836.
4. Eisenhofer G, Goldstein DS, Kopin IJ, Crout JR. Pheochromocytoma: rediscovery as a catecholamine-metabolizing tumor. Endocr Pathol. 2003; 14:193–212. PMID: 14586065.

5. Sawka AM, Jaeschke R, Singh RJ, Young WF Jr. A comparison of biochemical tests for pheochromocytoma: measurement of fractionated plasma metanephrines compared with the combination of 24-hour urinary metanephrines and catecholamines. J Clin Endocrinol Metab. 2003; 88:553–558. PMID: 12574179.

6. Peaston RT, Graham KS, Chambers E, van der Molen JC, Ball S. Performance of plasma free metanephrines measured by liquid chromatography-tandem mass spectrometry in the diagnosis of pheochromocytoma. Clin Chim Acta. 2010; 411:546–552. PMID: 20083099.

7. Grossman A, Pacak K, Sawka A, Lenders JW, Harlander D, Peaston RT, et al. Biochemical diagnosis and localization of pheochromocytoma: can we reach a consensus? Ann N Y Acad Sci. 2006; 1073:332–347. PMID: 17102103.

8. Singh RJ, Eisenhofer G. High-throughput, automated, and accurate biochemical screening for pheochromocytoma: are we there yet? Clin Chem. 2007; 53:1565–1567. PMID: 17711998.

9. Sawka AM, Gafni A, Thabane L, Young WF Jr. The economic implications of three biochemical screening algorithms for pheochromocytoma. J Clin Endocrinol Metab. 2004; 89:2859–2866. PMID: 15181069.

10. Eisenhofer G, Siegert G, Kotzerke J, Bornstein SR, Pacak K. Current progress and future challenges in the biochemical diagnosis and treatment of pheochromocytomas and paragangliomas. Horm Metab Res. 2008; 40:329–337. PMID: 18491252.

11. de Jong WH, Graham KS, van der Molen JC, Links TP, Morris MR, Ross HA, et al. Plasma free metanephrine measurement using automated online solid-phase extraction HPLC tandem mass spectrometry. Clin Chem. 2007; 53:1684–1693. PMID: 17712005.
12. Lagerstedt SA, O'Kane DJ, Singh RJ. Measurement of plasma free metanephrine and normetanephrine by liquid chromatography-tandem mass spectrometry for diagnosis of pheochromocytoma. Clin Chem. 2004; 50:603–611. PMID: 14726465.

13. Trufelli H, Palma P, Famiglini G, Cappiello A. An overview of matrix effects in liquid chromatography-mass spectrometry. Mass Spectrom Rev. 2011; 30:491–509. PMID: 21500246.

Fig. 1
Chromatograms of (A) d3-metanephrine-HCl (0.4 ng/mL), (B) metanephrine (2.0 nmol/L), (C) d3-normetanephrine-HCl (0.8 ng/mL), and (D) normetanephrine (4.0 nmol/L).
Abbreviation: MRM, multiple-reaction monitoring.
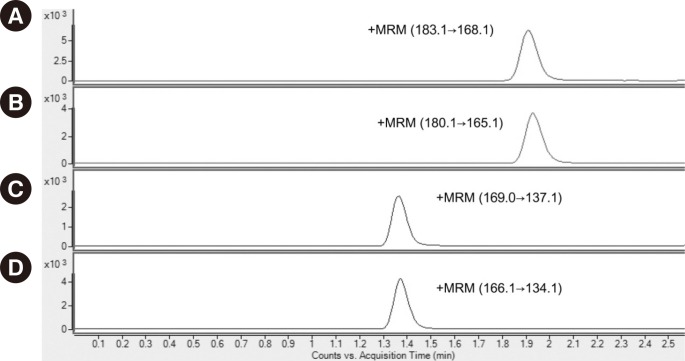
Fig. 2
Dot-box and whisker plots showing the distribution of the levels of plasma metanephrine (A) and normetanephrine (B) in healthy normotensive volunteers and in patients with essential hypertension, adrenal adenoma, or proven pheochromocytoma. The central box represents the values from the lower to upper quartiles (25th to 75th percentiles). The middle line represents the median. A line extends from the minimum to the maximum value, excluding "outside" values (greater than the upper quartile plus 1.5 times the interquartile range) and "outlying" values (greater than the upper quartile plus three times the interquartile range, marked as □), which are displayed as separate points.
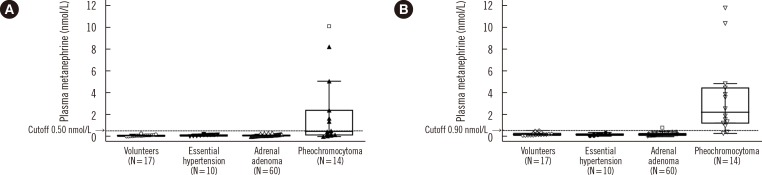
Table 1
Precision of the LC-MS/MS method for the measurement of metanephrine and normetanephrine




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download