B-cell lymphoma, unclassifiable, with intermediate features between those of diffuse large B-cell lymphoma (DLBCL) and Burkitt lymphoma (BL; intermediate BL/DLBCL) commonly exhibits a morphology similar to that of typical BL and an atypical immunophenotype such as diffuse and moderate-to-strong BCL2 positivity and/or a Ki67 proliferation index <90%. Alternatively, the tumor cells exhibit greater variations in nuclear size and contouring than would be considered acceptable for BL [1, 2]. Intermediate BL/DLBCL is most commonly observed in adults [3, 4, 5]. Among pediatric populations, to date, the English literature only includes reports of one case of intermediate BL/DLBCL in a 2-yr-old Korean boy and eight cases in Chinese children [6, 7]. Here, we report two additional cases that represent the first report from a western population.
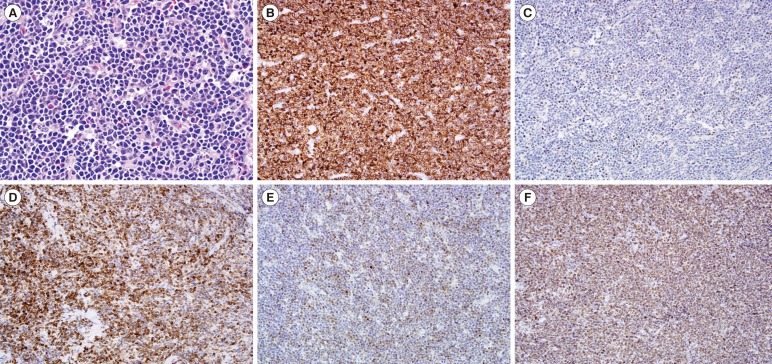
A 15-yr-old girl with sudden-onset abdominal pain and emesis was found to have a small bowel obstruction and intussusception during a computed tomography (CT) study. An urgent exploratory laparotomy revealed a mass comprising mildly to moderately pleomorphic lymphoid cells that were mostly medium-sized with rare large cells and slightly irregular nuclear contours; these cells primarily contained 2-3 inconspicuous nucleoli or, occasionally, single prominent nucleoli. Mitotic figures were frequent. Focally, tingible body macrophages imparted a "starry sky" appearance. The atypical lymphoid cells were positive for CD20, CD10, BCL-6 (focal, weak), MUM-1, and BCL-2 and negative for terminal deoxynucleotidyl transferase (TdT). The proliferative index, as indicated by Ki-67 staining, was high (>90%; Fig. 1). An Epstein-Barr virus (EBV) study with late membrane protein 1 (LMP1) immunohistochemical stain (IHC) and in situ hybridization for EBV-encoded RNAs (EBER), flow cytometric analysis, and karyotyping were not performed. FISH analysis revealed MYC rearrangement but no BCL2 or BCL6 rearrangement or copy number changes. Three of the 16 resected lymph nodes were also positive for intermediate BL/DLBCL. The patient underwent chemotherapy with cyclophosphamide, vincristine, prednisone, doxorubicin, and methotrexate. She remained in complete remission 11 months after completing chemotherapy.
A 4-yr-old boy with a 2-week history of abdominal distension and diarrhea was found to have diffuse bowel wall thickening on CT. A transrectal biopsy revealed a diffuse infiltrate of predominantly medium-sized with rare large atypical lymphoid cells; these cells had slightly irregular nuclear contours, vesicular chromatin, and mostly inconspicuous nucleoli. Apoptotic bodies and mitotic figures were frequently observed. The atypical lymphoid cells were positive for CD20, PAX-5, CD10, BCL-6, and BCL-2 and exhibited a high proliferative index, as indicated by Ki-67 staining (> 95%). MUM-1 staining was negative. The EBV study was negative according to LMP1 IHC and EBER in situ hybridization. Concurrent flow cytometric analysis revealed a monoclonal B-cell population with CD19, CD20, CD22, CD10, and surface kappa light-chain expression. The monoclonal B cells were negative for CD5, CD23, CD34, and TdT. A cytogenetic analysis (karyotyping) was not performed. FISH analysis with a MYC dual-color break apart probe revealed MYC rearrangement. There was no evidence of BCL2/IGH fusion, BCL6 rearrangement, or copy number changes in BCL2 or BCL6. The bone marrow and central nervous system were not involved (stage III). This patient received the same chemotherapy regimen as patient 1 and remained in remission for 12 months, as per the last follow-up.
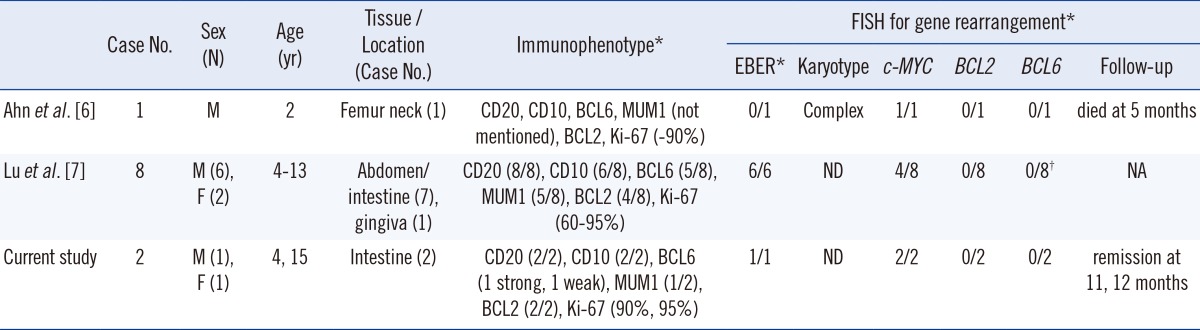
We conducted a systematic review of the pediatric high-grade mature B-cell lymphoma cases in our archives from 1988 to 2012 and identified 2 cases of intermediate BL/DLBCL. Both cases exhibited histologic morphology compatible with BL but with moderate-to-strong BCL-2 expression. Weak BCL-2 expression might be observed in BL [2]. In our experience, BCL-2 staining has yielded consistently negative or weakly positive (few cells) results in cases of BL. In addition, Case 1 exhibited focal and weak BCL6 expression and moderate-to-strong MUM-1 expression, which would be unusual for a diagnosis of BL [2]. The focal and weak BCL6 staining in Case 2 was not likely caused by poor tissue preservation and/or the stain itself, as the staining of samples from the same tissue block for other nuclear markers (MUM-1 and Ki-67) was successful. To the best of our knowledge, these two cases represent the first report of pediatric intermediate BL/DLBCL in a western population. A comparison of the current cases with previously reported pediatric intermediate BL/DLBCL cases in Asian populations is summarized in Table 1.
The current treatments for pediatric BL, DLBCL, and intermediate BL/DLBCL are similar [8]. However, treatment for patients aged 15-20 yr has been controversial because adolescent DLBCL patients fare better when treated with more aggressive regimens, compared with those who receive a cyclophosphamide, doxorubicin, vincristine, prednisone (CHOP)-like regimen [9, 10]. Both of our patients were treated with a BL chemotherapeutic regimen. It will be interesting to observe the responses of our patients, particularly the 15-yr-old female patient, during long-term follow-up. With the development of individualized targeted therapies, the recognition of pediatric intermediate BL/DLBCL might become more clinically relevant.
References
1. Carbone A, Gloghini A, Aiello A, Testi A, Cabras A. B-cell lymphomas with features intermediate between distinct pathologic entities. From pathogenesis to pathology. Hum Pathol. 2010; 41:621–631. PMID: 20398809.

2. Kluin PM, Harris NL, Stein H, Leoncini L, Raphael M, Campo E, et al. B-cell lymphoma, unclassifiable, with features intermediate between diffuse large B-cell lymphoma and Burkitt lymphoma. In : Swerdlow SH, Harris NL, Jaffe ES, Pileri SA, Stein H, Thiele J, Vardiman JW, editors. WHO classification of tumours of haematopoietic and lymphoid tissues. Lyon: IARC Press;2008. p. 265–266.
3. Liang X, Greffe B, Cook B, Giller R, Graham DK, McGranahan AN, et al. Gray zone lymphomas in pediatric patients. Pediatr Dev Pathol. 2011; 14:57–63. PMID: 20331368.

4. Lin P, Dickason TJ, Fayad LE, Lennon PA, Hu P, Garcia M, et al. Prognostic value of MYC rearrangement in cases of B-cell lymphoma, unclassifiable, with features intermediate between diffuse large B-cell lymphoma and Burkitt lymphoma. Cancer. 2012; 118:1566–1573. PMID: 21882178.

5. Salaverria I, Siebert R. The gray zone between Burkitt's lymphoma and diffuse large B-cell lymphoma from a genetics perspective. J Clin Oncol. 2011; 29:1835–1843. PMID: 21482997.

6. Ahn JY, Seo YH, Park PW, Kim KH, Park MJ, Jeong JH, et al. A case of B-cell lymphoma, unclassifiable, with features intermediate between diffuse large B-cell lymphoma and Burkitt lymphoma in a Korean child. Ann Lab Med. 2012; 32:162–166. PMID: 22389885.

7. Lu B, Zhou C, Yang W, Huang H, Gao Z, He Y, et al. Morphological, immunophenotypic and molecular characterization of mature aggressive B-cell lymphomas in Chinese pediatric patients. Leuk Lymphoma. 2011; 52:2356–2364. PMID: 21740296.

8. Reiter A, Schrappe M, Parwaresch R, Henze G, Müller-Weihrich S, Sauter S, et al. Non-Hodgkin's lymphomas of childhood and adolescence: results of a treatment stratified for biologic subtypes and stage--a report of the Berlin-Frankfurt-Münster Group. J Clin Oncol. 1995; 13:359–372. PMID: 7844597.

9. Cairo MS, Gerrard M, Sposto R, Auperin A, Pinkerton CR, Michon J, et al. Results of a randomized international study of high-risk central nervous system B non-Hodgkin lymphoma and B acute lymphoblastic leukemia in children and adolescents. Blood. 2007; 109:2736–2743. PMID: 17138821.

10. Patte C, Auperin A, Gerrad M, Michon J, Pinkerton R, Sposto R, et al. Results of the randomized international FAB/LMB96 trial for intermediate risk B-cell non-Hodgkin lymphoma in children and adolescents: it is possible to reduce treatment for the early responding patients. Blood. 2007; 109:2773–2780. PMID: 17132719.

Fig. 1
Morphologic (A, Hematoxylin and eosin staining, ×50) and immunophenotypic (B-F, ×20) features of B-cell lymphoma, unclassifiable, with intermediate features between DLBCL and Burkitt lymphoma. (B) CD20, (C) BCL-6, (D) BCL-2, (E) MUM-1, and (F) Ki-67.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download