Abstract
Noroviruses are the leading cause of epidemic gastroenteritis, including foodborne outbreak, in Korea. The prevalence of human noroviruses was studied in diarrheal stool samples of patients with acute gastroenteritis by conventional duplex reverse transcription (RT)-PCR. Diarrheal stool samples were collected from 1,685 patients from the local hospitals in Seoul. The prevalence of the noroviruses was 22.8% (222/972 patients) in 2012 and 11.2% (80/713 patients) in 2013, with a total of 17.9% (302/1,685 patients). Genotyping was performed on 302 norovirus-positive stool samples to reveal 5.6% prevalence of genogroup I (GI) (17/302) and 94.4% prevalence of genogroup II (GII) (285/302). The patients with norovirus-associated acute gastroenteritis mostly showed prevalence of GII norovirus, especially GII.4 (64.6%; 195/302).
Monitoring of diarrheal patients in Korea has revealed a declining trend of bacterial infections and a rising trend of viral infections. Gastroenteritis caused by noroviruses is becoming increasingly common and, owing to its contagious nature, it is easily transmitted [1, 2, 3, 4, 5]. Hence, noroviruses have been identified as the most common causative agent [6]. In the present study, we investigated the prevalence of common human norovirus in patients with acute gastroenteritis.
Diarrheal stool samples from 1,685 patients suffering from acute gastroenteritis were collected from six local hospitals in Seoul (SW hospital, SG hospital, AM center, NP hospital, EJ hospital, and NM center) between 2012 and 2013. The samples were tested for the presence of norovirus. Briefly, 1 g of feces was mixed with 9 mL of sterile 0.1 M phosphate-buffered saline (PBS; pH 7.4; Sigma, St. Louis, MO, USA) and centrifuged at 1,660 g for 30 min at 4℃. The supernatant was collected and used for fragmentation at 4℃. At the AM center, 0.5-1 mL of the rectal swab suspensions were collected and mixed with PBS for further processing. The 1,685 diarrheal stool samples (direct rectal swabs or diarrheal feces of patients) from six hospitals were transported at 4℃ within 8 hr of collection to the Seoul Metropolitan Research Institute of Public Health and Environment, where they were stored at -70℃ until further analysis.
For the detection of noroviruses, one-step reverse transcription (RT)-PCR, followed by electrophoresis, was performed [7]. RNA was extracted by using the Viral RNA Mini Kit (QIAgen, Hilden, Germany) [8]. One-step duplex RT-PCR was performed by using the RT/PCR Diagnostic Norovirus Kit (Bioneer, Daejeon, Korea) and the GI-FIM, GI-RIM, and GI-F2 primer pairs for GI detection; the GII-FIM, GII-RIM, and GII-F3 primer pairs for GII detection; -and primers hybridized within the open reading frame 3 regions (5'-CTGCCCGAATTYGTAAATAAATGATGAT-3', 5'-CCAACCCARCCATTRTACATYTG-3', and 5'-ATGATGATGGCGTCTAAGGACGC-3' respectively) for GI detection and another 3 regions (5'-GGGAGGGCGATCGCAATCT-3', 5'-CCRCCIGCATRICCRTTRTACAT-3', and 5'-TTGTGAATGAAGATGGCGTCGART-3', respectively) for GII detection [1, 2, 3, 4, 5]. Positive results were defined as the presence of a 314-bp band for norovirus GI and a 313-bp band for norovirus GII [1, 2, 3, 4, 5].
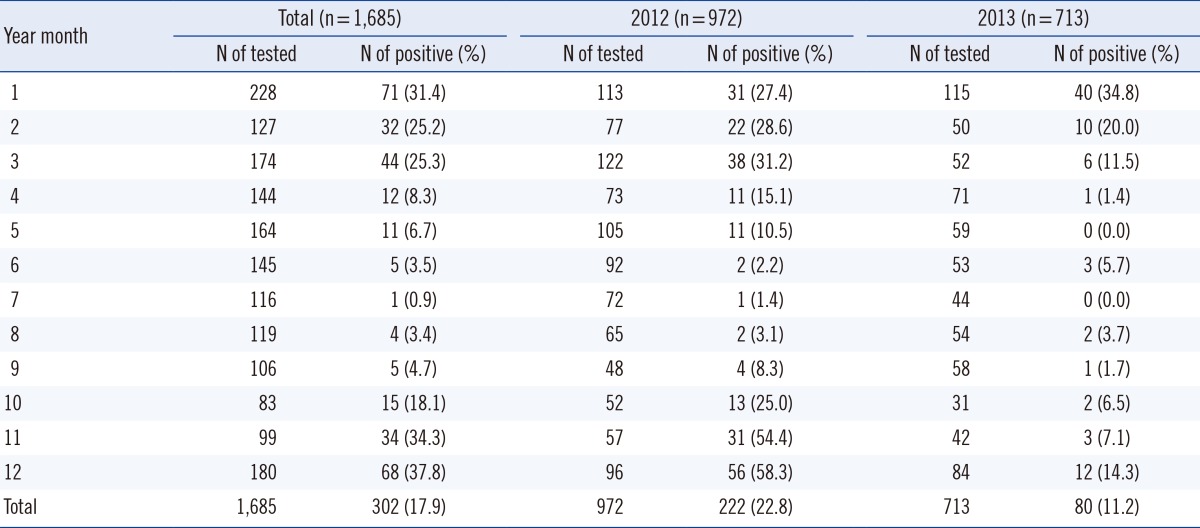
Our analysis showed that the norovirus detection rate was 22.8% (222/972 patients) in 2012 and 11.2% (80/713 patients) in 2013, with a total rate of 17.9% (302/1,685 patients) (Table 1). In subsequent studies, monthly surveillance of norovirus prevalence over a period of 2 yr (2012-2013) revealed the highest frequency between October and March.
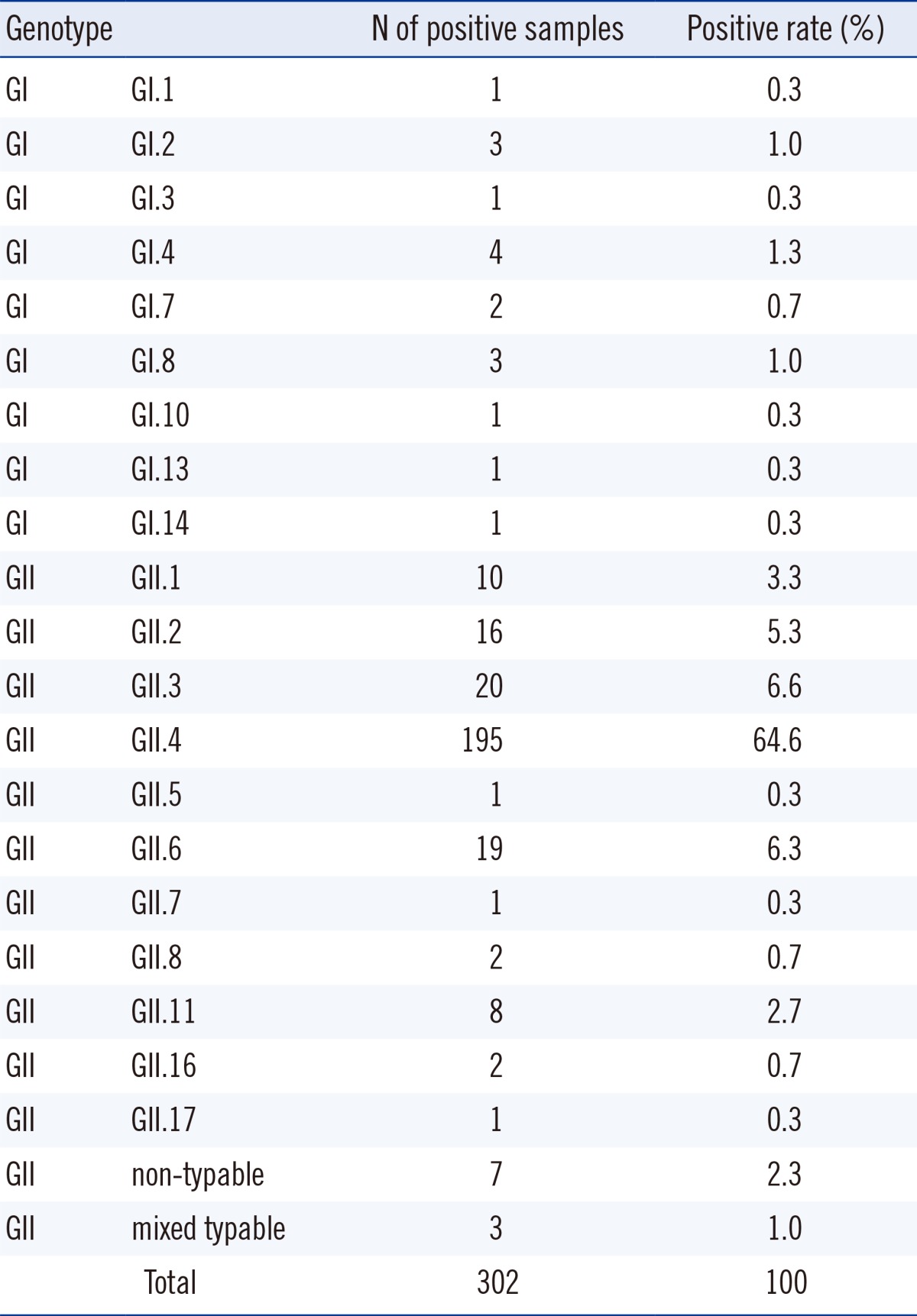
Genotyping of 302 (17.9%) norovirus-positive samples revealed 5.6% (17/302) prevalence of GI- and 94.4% (285/302) prevalence of GII. Notably, in norovirus-associated acute gastroenteritis patients, the prevalence of GII genotype norovirus was the highest, especially of GII.4 (64.6%;195/302) (Table 2).
In the Hallym University Hospital, the epidemicity of norovirus started in October 2007, peaked in November 2007, and lasted until January in 2008; again, in the same hospital, the epidemicity started in December 2009, peaked in January 2010, and lasted until February 2010 [6]. Kong et al. [8] reported the highest detection rate of norovirus in November 2005 (12.3%, 28/227) and in March 2006 (35.3%, 79/224), followed by that in March 2007 (45.9%, 62/135) in Incheon. Ham et al. [4] reported the highest peak in January (35.6%, 366/1,028), and the lowest in July (2.4%, 20/818) from 2007 to 2011, followed by that in January, February, and November from 2010 to 2013, in Seoul [5]. In addition, the Korea Centers for Disease Control and Prevention (KCDC) reported that norovirus prevalence- peaks from November to March in Korea [9]. In this study, the prevalence of noroviruses was found to be the highest between October and March in the years 2012 and 2013.
Of the 11,202 acute gastroenteritis patients whose stool samples were examined from 2007 to 2011 in Seoul, 16.6% (1,861/11,202) were found to be positive for noroviruses by RT-PCR in the Hallym University Hospital. Of the 1,861 noroviruses, 95.5% were detected as GII and 3.9% were detected as GI [4]. Approximately 6,618 acute gastroenteritis patients were recorded between 2005 and 2007 in Incheon; of the 6,618 stool samples tested, 10.7% (708/6,618) were determined to be infected with noroviruses by RT-PCR. Of the 708 noroviruses, GI constituted 0.6% and GII constituted 99.4% (69.7% GII.4 and 17.2% GII.3) [8]. Of the 1,718 acute gastroenteritis patients recorded between 2012 and 2013 in the Hallym University Hospital, 14.8% (254/1718) were positive for human norovirus as determined by using the norovirus antigen test kit. Of the 254 norovirus cases detected, 2.2% was attributable to GI and 97.8% to GII. Of the 97.8% GII noroviruses detected, 63.7% was attributable to GII.4, constituted by 60.4% GII.4 Sydney and 3.3% GII.4 Non-Sydney (Den Haag 2006b) [10]. Yu et al. [11] reported that norovirus GI accounted for 4% of the detected norovirus cases, while norovirus GII accounted for 92%, of which 70% was attributable to GII.4, between 1999 and 2011 in China. Bok et al. [12] stated that norovirus GI accounted for 3.4% of the detected noroviruses and GII accounted for 95.8%. Of the GII-positive cases, 16% of the cases were attributed to GII.4; these cases were over a 34-yr period between 1974 and 1991 in the Washington DC region in the USA.
Consequently, most of the gastroenteritis patients were related to GII norovirus infection, especially noroviruses GII.4. Our results on the prevalence of noroviruses were in accordance with previous results; for instance, the prevalence of GI (5.6%) and GII (94.4%) was similar to that in previous studies (0.6-3.9% and 92.0-99.4%, respectively) [4, 8, 10, 11, 12], while the prevalence of GII.4 (64.6%) was similar to that in other studies (63.7-70.0%) [8, 10, 11], but different from that in Bok et al. (16.0%) [12].
In addition, in Hallym University Hospital, 13.0% (1,463/11,219) of the stool samples in gastroenteritis patients were determined to be positive for noroviruses from 2007 to 2010 by using the norovirus ELISA kit [6]. The KCDC reported that, out of 18,908 diarrheal stool samples, 8.5% (1,608) were found to be positive for human norovirus in 2013 [9]. In 4,484 stool samples obtained from 461 patients of food poisoning during on outbreak from 2010 to 2013 in Seoul, 9.77% (438/4,484) were determined to be positive for noroviruses by RT-PCR; of the 438 noroviruses, 75.92% was positive for norovirus GII, and 54.05% for norovirus GII.4 [5].
All stool samples were obtained from outpatients of six hospitals, including one primary hospital (AM center), three secondary hospitals (SW hospital, NP hospital, and NM center), and two tertiary hospitals (SG and EJ hospitals). The norovirus detection rate was different among the three types of hospitals. The order of norovirus detection rate in gastroenteritis patients was primary (14.6%) < secondary (20.5%) < tertiary (26.8%) in 2012 and secondary (9.0%) < tertiary (12.0%) < primary (12.6%) in 2013. However, no differences were noted in the norovirus positive rates between stool and rectal swab samples.
In conclusion, noroviruses were found to be prevalent in patients with gastroenteritis, with a higher occurrence between October and March over the 12-month period between 2012 and 2013. Our analysis of diarrheal stool samples collected during 2012 to 2013 from local hospitals in Seoul revealed norovirus detection in 17.9% of the gastroenteritis patients (302/1,685), of whom, 5.6% (17/302) was constituted by norovirus GI and 94.4% (285/302) by norovirus GII (64.6% GII.4).
Acknowledgments
We are grateful to the EnterNet-Korea Project of the Korean CDC for supporting this study.
References
1. Lee JI. Molecular characterization of enteric viruses isolated from acute gastroenteritis patients. Chung Buk University;2008. Ph.D. Thesis.
2. Park SH, Kim EJ, Oh SA, Kim CK, Choi SS, Cho SJ, et al. Viral agents associated with acute gastroenteritis in Seoul, Korea. Clin Lab. 2011; 57:59–65. PMID: 21391466.
3. Lee JI, Park SH, Kim MS, Oh YH, Yu IS, Choi BH, et al. Surveillance of acute gastroenteritis in Seoul, Korea, during May 2004 and June 2007. J Bacteriol Virol. 2009; 39:363–371.

4. Ham HJ, Oh SA, Kim CK, Jang JI, Cho SJ, Choi SM. Molecular characteristics of human noroviruses genogroup I and genogroup II detected in acute gastroenteritis patients in Seoul. J Environ Health Sci. 2012; 38:57–65.

5. Oh SA, Park SH, Ham HJ, Seung HJ, Jang JI, Suh SW, et al. Molecular characterization of norovirus and rotavirus in outbreak of acute gastroenteritis in Seoul. J Bacteriol Virol. 2013; 43:307–316.

6. Park DJ, Kim JS, Park JY, Kim HS, Song WK, Kim HS, et al. Epidemiological analysis of norovirus infection between March 2007 and February 2010. Korean J Lab Med. 2010; 30:647–653. PMID: 21157152.

7. Korea Centers for Disease Control and Prevention (KCDC). K-Calcinet. National norovirus laboratory surveillance: 2013. http://www.google.co.kr/url?sa=t&rct=j&q=&esrc=s&frm=1&source=web&cd=1&ved=0CBwQFjAA&url=http%3A%2F%2Fwww.cdc.go.kr%2FCDC%2Fcms%2FcmsFileDownload.jsp%3Ffid%3D31%26cid%3D22015%26fieldName%3Dattach1%26index%3D1&ei=nUCKVMOWDZLz8gWdnoHwDw&usg=AFQjCNEAE32JB_qUoBija4o14zIve9jOog&bvm=bv.81828268,d.dGc&cad=rjt.
8. Gong YW, Oh BY, Kim HY, Lee MY, Kim YH, Go JM, et al. Molecular epidemiologic investigation of norovirus infections in Incheon city, Korea, from 2005 to 2007. J Bacteriol Virol. 2008; 38:249–257.

9. Korea Centers for Disease Control and Prevention (KCDC). EnterNet Korea. Laboratory surveillance of viral acute gastroenteritis in Korea;2012. Updated on Nov 2013. http://www.cdc.go.kr/CDC/notice/CdcKrInfo0301.jsp?menuIds=HOME001-MNU0004-MNU0036-MNU0037&cid=21904. Yearly Report 2013;41-52.
10. Kim HS, Hyun JW, Kim HS, Kim JS, Song WK, Lee KM. Emergence of GII.4 Sydney norovirus in South Korea during the winter of 2012-2013. J Microbiol Biotechnol. 2013; 23:1641–1643. PMID: 24043126.

11. Yu Y, Yan S, Li B, Pan Y, Wang Y. Genetic diversity distribution of human norovirus in China (1999-2011). Biomed Res Int. 2014; 2014:196169. PMID: 24672783.
12. Bok K, Abente EJ, Realpe-Quintero M, Mitra T, Sosnovtsev SV, Kapikian AZ, et al. Evolutionary dynamics of GII.4 noroviruses over a 34-year period. J Virol. 2009; 83:11890–11901. PMID: 19759138.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download