Lymphomas of different histological types can occur at the same anatomical site (composite lymphoma) or at different sites, and can arise simultaneously or sequentially [1, 2]. Reports of patients in whom histologically distinct lymphomas occur simultaneously at different sites are rare [3, 4]. Among these rare cases, the simultaneous occurrence of T- and B-cell lymphomas is extremely rare [5]. To the best of our knowledge, composite involvement of T- and B-cell lymphomas in the bone marrow (BM) have not been reported so far. We report a case of composite BM involvement by T- and B-cell lymphomas.
A 52-yr-old woman presented with abdominal discomfort. She had a history of hepatitis B-related liver cirrhosis and was taking lamivudine. She had lost 4 kg of weight in the previous 4 months. Laboratory investigation revealed pancytopenia (white blood cells, 1.7×109/L [reference range: 4-10×109/L]; hemoglobin, 11.0 g/dL [12-16 g/dL]; and platelets, 75×109/L [150-350×109/L]), elevated levels of liver enzymes (aspartate transaminase, 75 IU/L [0-40 IU/L]; alkaline phosphatase, 129 IU/L [40-120 IU/L]; γ-glutamyltransferase, 99 IU/L [8-35 IU/L]), and an increased level of lactate dehydrogenase (315 IU/L [120-250 IU/L]). Dynamic computed tomography revealed an ill-defined, 3-cm lesion in the left lateral segment of the liver and multiple abdominal and mediastinal lymphadenopathies. Esophagogastroduodenoscopy revealed a 3-cm ulcerofungating mass between the antrum and the lower body of the stomach. A liver core needle biopsy identified a peripheral T-cell lymphoma, not otherwise specified, and an endoscopic biopsy of the stomach identified a diffuse large B-cell lymphoma (DLBL). A BM biopsy revealed BM involvement by DLBL with a nodular infiltration pattern, which was corroborated by positive immunohistochemical staining for CD3 and CD20. CD20-positive lymphocytes were present in nodular aggregates. CD3-positive lymphocytes were present in small lymphocytes surrounding CD20-positive lymphocytes suggesting reactive T lymphocytes. A cytogenetic study of BM revealed an apparently normal karyotype. The patient was started on the combination chemotherapy regimen including rituximab, cyclophosphamide, doxorubicin, vincristine and prednisolone (R-CHOP).
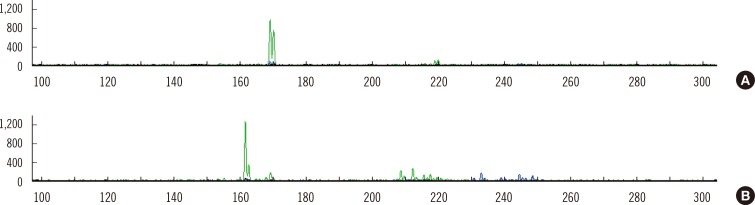
After 6 cycles of R-CHOP, the liver mass and lymphadenopathies had disappeared. However, a follow-up BM biopsy revealed BM involvement by T-cell lymphoma and DLBL. Immunohistochemical staining showed medium to large sized PAX5-positive lymphocytes with a marked interstitial infiltration pattern (Fig. 1A, B), and the cells were also CD79a-positive. Peritrabecular and interstitial infiltration of small to medium sized CD3-positive lymphocytes was also prominent (Fig. 1C, D). Rearrangements of the T-cell receptor gamma locus (TRG) and immunoglobulin heavy locus (IGH) were studied in BM (after the 6th cycle of R-CHOP), liver, and stomach (at diagnosis) specimens using the BIOMED-2 multiplex PCR protocol [6]. A 170-bp monoclonal TRG rearrangement was detected in the liver sample (Fig. 2A), while TRG in the BM had a larger 160-bp peak with a smaller 170-bp peak (Fig. 2B). IGH gene rearrangements were not detected in the stomach sample or in the BM aspirate, and the BM aspirate had a normal karyotype. After the 8th R-CHOP cycle, computed tomography and positron emission tomography findings suggested involvement of multiple lymph nodes (celiac, splenic hilar, and abdominal paraaortic lymph nodes). The patient died of pneumonia 1 yr after diagnosis.
In our TRG rearrangement study, monoclonal TRG rearrangements were detected in both liver and BM samples, but the sizes of amplicons were slightly different, that is a finding that may be explained by clonal evolution [7]. We speculate that there is BM involvement on the basis of a subclone from the hepatic T-cell lymphoma. Moreover, a small peak corresponding to a 170-bp PCR product was observed in a BM sample, which suggests that the same clone present in the liver sample was also present in the BM sample. Monoclonal IGH rearrangements were not detected in the stomach or BM sample. As monoclonal IGH rearrangements are detected in approximately 80% of DLBL cases using BIOMED-2 multiplex PCR [8], the fact that rearrangement of IGH was not detected in the stomach sample is not unusual.
T- and B-cell lymphomas simultaneously developed in this patient. Moreover, a follow-up examination suggested BM involvement by both these lymphomas. To our knowledge, this is the first report of a patient with BM involvement by both T- and B-cell lymphomas. Factors contributing to the development of synchronous primary lymphomas have not been investigated, and a case with involvement of the same site by two different lymphomas has not been reported; however, primary composite lymphomas have been reported [9]. The clinical significance of BM involvement by both T- and B-cell lymphomas is unknown, although the simultaneous development of more than one histological type of lymphoma is associated with a poor prognosis [1]. The present patient died 1 yr after her diagnosis, suggesting that composite BM involvement may also be associated with a poor prognosis.
References
1. Tucci A, Motta M, Ungari M, Ruggeri G, Crippa C, Borlenghi E, et al. The development of more than one histologic type of lymphoma in the same patient is frequent and confers a worse prognosis. Haematologica. 2005; 90:348–352. PMID: 15749667.
2. Furlan A, Pietrogrande F, Marino F, Menin C, Polato G, Vianello F. Sequential development of large B cell lymphoma in a patient with peripheral T-cell lymphoma. Haematologica. 2008; 93:e6–e8. PMID: 18166774.

3. Terada T. One patient with double lymphomas: simultaneous gastric MALT lymphoma and ileal diffuse large B-cell lymphoma. Int J Clin Exp Pathol. 2012; 5:260–263. PMID: 22558482.
4. Tang Z, Jing W, Lindeman N, Harris NL, Ferry JA. One patient, two lymphomas. Simultaneous primary gastric marginal zone lymphoma and primary duodenal follicular lymphoma. Arch Pathol Lab Med. 2004; 128:1035–1038. PMID: 15335250.
5. Cotter FE, Hall PA, Young BD, Lister TA. Simultaneous presentation of T- and B-cell malignant lymphoma with bcl-2 gene involvement. Blood. 1989; 73:1387–1388. PMID: 2649177.
6. van Dongen JJ, Langerak AW, Bruggemann M, Evans PA, Hummel M, Lavender FL, et al. Design and standardization of PCR primers and protocols for detection of clonal immunoglobulin and T-cell receptor gene recombinations in suspect lymphoproliferations: report of the BIOMED-2 Concerted Action BMH4-CT98-3936. Leukemia. 2003; 17:2257–2317. PMID: 14671650.

7. Umino A, Nakagawa M, Utsunomiya A, Tsukasaki K, Taira N, Katayama N, et al. Clonal evolution of adult T-cell leukemia/lymphoma takes place in the lymph nodes. Blood. 2011; 117:5473–5478. PMID: 21447829.

8. Evans PA, Pott Ch, Groenen PJ, Salles G, Davi F, Berger F, et al. Significantly improved PCR-based clonality testing in B-cell malignancies by use of multiple immunoglobulin gene targets. Report of the BIOMED-2 Concerted Action BHM4-CT98-3936. Leukemia. 2007; 21:207–214. PMID: 17170731.

9. Wang HW, Yang W, Wang L, Lu YL, Lu JY. Composite diffuse large B-cell lymphoma and classical Hodgkin's lymphoma of the stomach: case report and literature review. World J Gastroenterol. 2013; 19:6304–6309. PMID: 24115832.

Fig. 1
Bone marrow biopsy after 6 cycles of rituximab, cyclophosphamide, doxorubicin, vincristine and prednisolone (R-CHOP) combination chemotherapy. (A, B) Neoplastic B lymphocytes infiltrating in an interstitial pattern was immunohistochemically analyzed by anti-PAX5 antibody (A, ×100; B, ×1,000). (C, D) Neoplastic T lymphocytes infiltrating with a peritrabecular or interstitial pattern was immunohistochemically analyzed by anti-CD3 antibody (C, ×100; D, ×1,000).
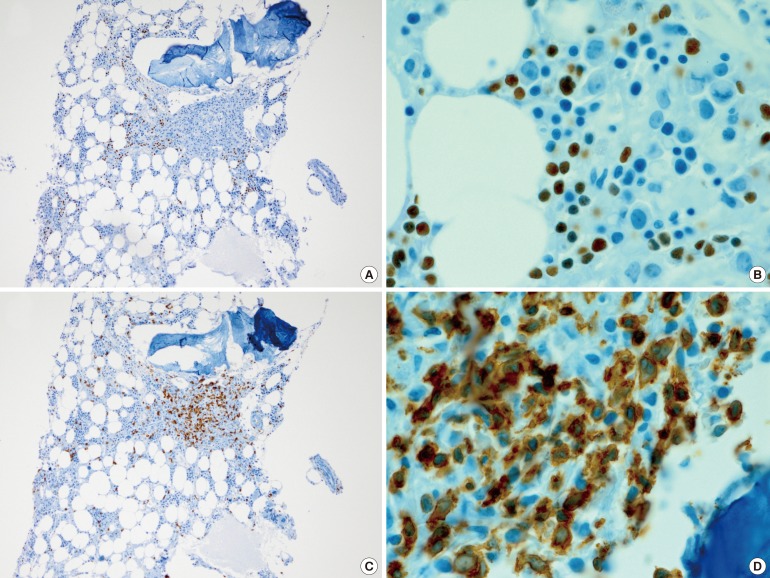
Fig. 2
T cell receptor gamma locus (TRG) rearrangement analyzed by using BIOMED-2 multiplex PCR. Horizontal axis represents amplicon size (base pairs) and vertical axis represents fluorescence intensity. (A) A monoclonal TRG rearrangement was detected at 170 bp in the liver sample. (B) Both a larger peak (160 bp) and a smaller peak (170 bp) were observed in the bone marrow aspirate sample by GeneScan analysis of the PCR results.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download