1. Lane DA, Mannucci PM, Bauer KA, Bertina RM, Bochkov NP, Boulyjenkov V, et al. Inherited thrombophilia: Part 1. Thromb Haemost. 1996; 76:651–662. PMID:
8950768.

2. Lane DA, Mannucci PM, Bauer KA, Bertina RM, Bochkov NP, Boulyjenkov V, et al. Inherited thrombophilia: Part 2. Thromb Haemost. 1996; 76:824–834. PMID:
8971998.

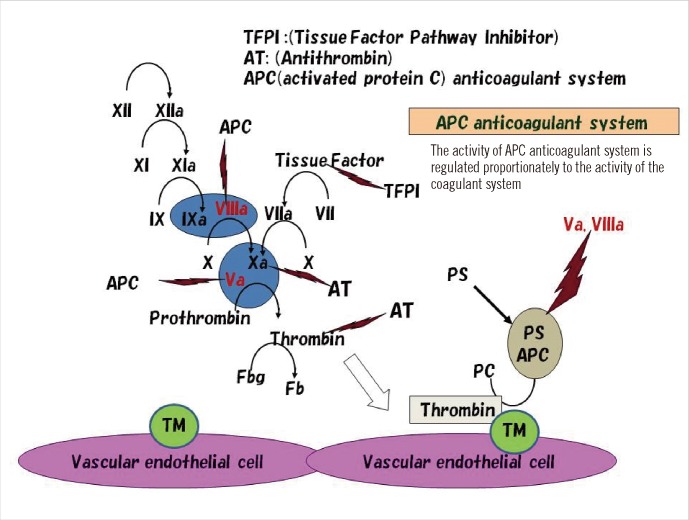
3. Dahlbäck B, Carlsson M, Svensson PJ. Familial thrombophilia due to a previously unrecognized mechanism characterized by poor anticoagulant response to activated protein C: prediction of a cofactor to activated protein C. Proc Natl Acad Sci USA. 1993; 90:1004–1008. PMID:
8430067.
4. Koster T, Rosendaal FR, de Ronde H, Briët E, Vandenbroucke JP, Bertina RM. Venous thrombosis due to poor anticoagulant response to activated protein C: Leiden Thrombophilia Study. Lancet. 1993; 342:1503–1506. PMID:
7902898.

5. Bertina RM, Koeleman BP, Koster T, Rosendaal FR, Dirven RJ, de Ronde H, et al. Mutation in blood coagulation factor V associated with resistance to activated protein C. Nature. 1994; 369:64–67. PMID:
8164741.

6. Ridker PM, Hennekens CH, Lindpaintner K, Stampfer MJ, Eisenberg PR, Miletich JP. Mutation in the gene coding for coagulation factor V and the risk of myocardial infarction, stroke, and venous thrombosis in apparently healthy men. N Engl J Med. 1995; 332:912–917. PMID:
7877648.

7. Rosendaal FR. Risk factors for venous thrombosis: prevalence, risk, and interaction. Semin Hematol. 1997; 34:171–187. PMID:
9241704.
8. Castoldi E, Rosing J. APC resistance: biological basis and acquired influences. J Thromb Haemost. 2010; 8:445–453. PMID:
20002539.

9. Poort SR, Rosendaal FR, Reitsma PH, Bertina RM. A common genetic variation in the 3'-untranslated region of the prothrombin gene is associated with elevated plasma prothrombin levels and an increase in venous thrombosis. Blood. 1996; 88:3698–3703. PMID:
8916933.

10. Franco RF, Reitsma PH. Genetic risk factors of venous thrombosis. Hum Genet. 2001; 109:369–384. PMID:
11702218.

11. Bounameaux H, Rosendaal FR. Venous thromboembolism: Why does ethnicity matter? Circulation. 2011; 123:2189–2191. PMID:
21555708.
12. Rees DC, Cox M, Clegg JB. World distribution of factor V Leiden. Lancet. 1995; 346:1133–1134. PMID:
7475606.

13. Seki T, Okayama H, Kumagai T, Kumasaka N, Sakuma M, Isoyama S, et al. Arg506Gln mutation of the coagulation factor V gene not detected in Japanese pulmonary thromboembolism. Heart Vessels. 1998; 13:195–198. PMID:
10442401.

14. Isshiki I, Murata M, Watanabe R, Matsubara Y, Kawano K, Aoki N, et al. Frequencies of prothrombin 20210 G A mutation may be different among races--studies on Japanese populations with various forms of thrombotic disorders and healthy subjects. Blood Coagul Fibrinolysis. 1998; 9:105–106. PMID:
9607126.
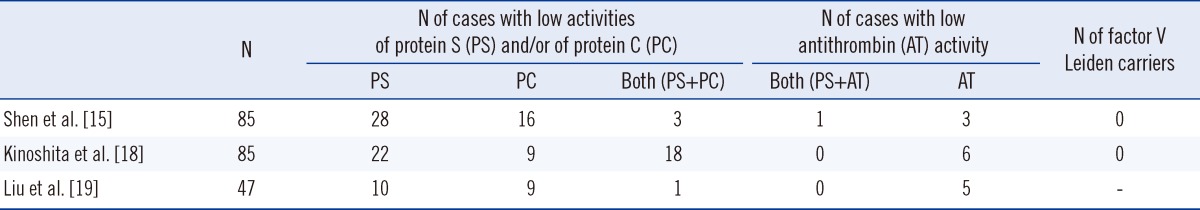
15. Shen MC, Lin JS, Tsay W. High prevalence of antithrombin III, protein C and protein S deficiency, but no factor V Leiden mutation in venous thrombophilic Chinese patients in Taiwan. Thromb Res. 1997; 87:377–385. PMID:
9271815.

16. Kim YW, Yoon KY, Park S, Shim YS, Cho HI, Park SS. Absence of factor V Leiden mutation in Koreans. Thromb Res. 1997; 86:181–182. PMID:
9175239.
17. Tang L, Guo T, Yang R, Mei H, Wang H, Lu X, et al. Genetic background analysis of protein C deficiency demonstrates a recurrent mutation associated with venous thrombosis in Chinese population. PLoS One. 2012; 7:e35773. PMID:
22545135.

18. Kinoshita S, Iida H, Inoue S, Watanabe K, Kurihara M, Wada Y, et al. Protein S and protein C gene mutations in Japanese deep vein thrombosis patients. Clin Biochem. 2005; 38:908–915. PMID:
15978566.

19. Liu HW, Kwong YL, Bourke C, Lam CK, Lie AK, Wei D, et al. High incidence of thrombophilia detected in Chinese patients with venous thrombosis. Thromb Haemost. 1994; 71:416–419. PMID:
8052955.

20. Tsuda H, Hattori S, Tanabe S, Iida H, Nakahara M, Nishioka S, et al. Screening for aetiology of thrombophilia: a high prevalence of protein S abnormality. Ann Clin Biochem. 1999; 36:423–432. PMID:
10456203.

21. Miyata T, Hamasaki N, Wada H, Kojima T. More on: racial differences in venous thromboembolism. J Thromb Haemost. 2012; 10:319–320. PMID:
22141429.

22. Trujillo-Santos AJ, Jiménez-Puente A, Perea-Milla E. Association between long travel and venous thromboembolic disease: a systematic review and meta-analysis of case-control studies. Ann Hematol. 2008; 87:79–86. PMID:
17899081.

24. Bhatia V, AroraP , Parida AK, Mittal A, Pandey AK, Kaul U. Air travel and pulmonary embolism: "economy class syndrome". J Assoc Physicians India. 2009; 57:412–414. PMID:
19634292.
25. Ueda S, Hanzawa K, Shibata M, Suzuki S. High prevalence of deep vein thrombosis in tsunami-flooded shelters established after the great East-Japan earthquake. Tohoku J Exp Med. 2012; 227:199–202. PMID:
22728376.

26. Shigekiyo T, Uno Y, Kawauchi S, Saito S, Hondo H, Nishioka J, et al. Protein S Tokushima: an abnormal protein S found in a Japanese family with thrombosis. Thromb Haemost. 1993; 70:244–246. PMID:
8236127.

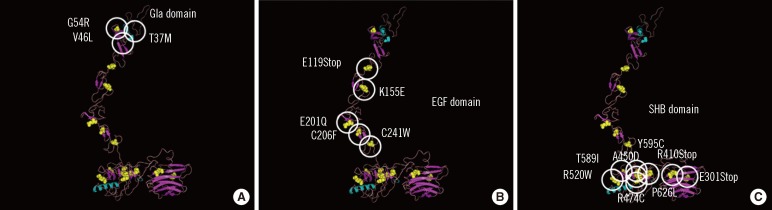
27. Yamazaki Y, Sugiura I, Matsushita T, Kojima T, Kagami K, Takamatsu J, et al. A phenotypically neutral dimorphism of protein S: the substitution of Lys155 by Glu in the second EGF domain predicted by an A to G base exchange in the gene. Thromb Res. 1993; 70:395–403. PMID:
8378895.

28. Hayashi T, Nishioka J, Shigekiyo T, Saito S, Suzuki K. Protein S Tokushima: abnormal molecule with a substitution of Glu for Lys-155 in the second epidermal growth factor-like domain of protein S. Blood. 1994; 83:683–690. PMID:
8298131.

29. Tsuda H, Urata M, Tsuda T, Wakiyama M, Iida H, Nakahara M, et al. Four missense mutations identified in the protein S gene of thrombosis patients with protein S deficiency: effects on secretion and anticoagulant activity of protein S. Thromb Res. 2002; 105:233–239. PMID:
11927129.
30. Kimura R, Honda S, Kawasaki T, Tsuji H, Madoiwa S, Sakata Y, et al. Protein S-K196E mutation as a genetic risk factor for deep vein thrombosis in Japanese patients. Blood. 2006; 107:1737–1738. PMID:
16461766.

31. Ikejiri M, Wada H, Sakamoto Y, Ito N, Nishioka J, Nakatani K, et al. The association of protein S Tokushima-K196E with a risk of deep vein thrombosis. Int J Hematol. 2010; 92:302–305. PMID:
20811787.

32. Hamasaki N. Japanese thrombophilia: Protein S/Protein C anomaly as the major risk factor for Japanese thrombophilia. Nihon Kessen Shiketsu Gakkai shi. 2006; 17:136–143. (in Japanese).
33. Tatewaki H, Iida H, Nakahara M, Tsuda H, Kinoshita S, Kanaji T, et al. A novel splice acceptor site mutation which produces multiple splicing abnormalities resulting in protein S deficiency type I. Thromb Haemost. 1999; 82:65–71. PMID:
10456456.

34. Nakahara M, Iida H, Urata M, Fujise M, Wakiyama M, Kinoshita S, et al. A novel splice acceptor site mutation of protein S gene in affected individuals with type I protein S deficiency: allelic exclusion of the mutant gene. Thromb Res. 2001; 101:387–393. PMID:
11297755.

35. Iida H, Nakahara M, Komori K, Fujise M, Wakiyama M, Urata M, et al. Failure in the detection of aberrant mRNA from the heterozygotic splice site mutant allele for protein S in a patient with protein S deficiency. Thromb Res. 2001; 102:187–196. PMID:
11369411.

36. Tsuda H, Tokunaga F, Nagamitsu H, Koide T. Characterization of endoplasmic reticulum-associated degradation of a protein S mutant identified in a family of quantitative protein S deficiency. Thromb Res. 2006; 117:323–331. PMID:
15893367.

37. Yamazaki T, Hamaguchi M, Katsumi A, Kagami K, Kojima T, Takamatsu J, et al. A quantitative protein S deficiency associated with a novel nonsense mutation and markedly reduced levels of mutated mRNA. Thromb Haemost. 1995; 74:590–595. PMID:
8584989.

38. Yamazaki T, Katsumi A, Kagami K, Okamoto Y, Sugiura I, Hamaguchi M, et al. Molecular basis of a hereditary type I protein S deficiency caused by a substitution of Cys for Arg474. Blood. 1996; 87:4643–4650. PMID:
8639833.

39. Okamoto Y, Yamazaki T, Katsumi A, Kojima T, Takamatsu J, Nishida M, et al. A novel nonsense mutation associated with an exon skipping in a patient with hereditary protein S deficiency type I. Thromb Haemost. 1996; 75:877–882. PMID:
8822579.

40. Yamazaki T, Katsumi A, Okamoto Y, Takafuta T, Tsuzuki S, Kagami K, et al. Two distinct novel splice site mutations in a compound heterozygous patient with protein S deficiency. Thromb Haemost. 1997; 77:14–20. PMID:
9031442.

41. Fujimura H, Kambayashi J, Kato H, Sakon M, Kawasaki T, Ariyoshi H, et al. Three novel missense mutations in unrelated Japanese patients with type I and type II protein S deficiency and venous thrombosis. Thromb Res. 1998; 89:151–160. PMID:
9651142.

42. Iwaki T, Mastushita T, Kobayashi T, Yamamoto Y, Nomura Y, Kagami K, et al. DNA sequence analysis of protein S deficiency--identification of four point mutations in twelve Japanese subjects. Semin Thromb Hemost. 2001; 27:155–160. PMID:
11372770.

43. Yamazaki T, Saito H, Dahlbäck B. Rapid intracellular degradation of a truncated mutant protein S (Q522X). Thromb Haemost. 2002; 87:171–172. PMID:
11848449.

44. Hirose M, Kimura F, Wang HQ, Takebayashi K, Kobayashi M, Nakanishi K, et al. Protein S gene mutation in a young woman with type III protein S deficiency and venous thrombosis during pregnancy. J Thromb Thrombolysis. 2002; 13:85–88. PMID:
12101385.
45. Okada H, Takagi A, Murate T, Adachi T, Yamamoto K, Matsushita T, et al. Identification of protein Sα gene mutations including four novel mutations in eight unrelated patients with protein S deficiency. Br J Haematol. 2004; 126:219–225. PMID:
15238143.

46. Okada H, Yamazaki T, Takagi A, Murate T, Yamamoto K, Takamatsu J, et al.
In vitro characterization of missense mutations associated with quantitative protein S deficiency. J Thromb Haemost. 2006; 4:2003–2009. PMID:
16961607.
47. Mizukami K, Nakabayashi T, Naitoh S, Takeda M, Tarumi T, Mizoguchi I, et al. One novel and one recurrent mutation in the PROS1 gene cause type I protein S deficiency in patients with pulmonary embolism associated with deep vein thrombosis. Am J Hematol. 2006; 81:787–797. PMID:
16868938.

48. Sanda N, Fujimori Y, Kashiwagi T, Takagi A, Murate T, Mizutani E, et al. An Sp1 binding site mutation of the PROS1 promoter in a patient with protein S deficiency. Br J Haematol. 2007; 138:663–665. PMID:
17596203.

49. Hamasaki N, Kanaji T. Tanaka K, Davie EW, editors. Clinical role of protein S deficiency in Asian population. Recent advances in thrombosis and hemostasis. 2008. Japan: Springer;p. 597–613.

50. Bonthron D. The human von Willebrand factor gene. Structure of the 5' region. Eur J Biochem. 1988; 171:51–57. PMID:
2828057.

51. Mancuso DJ, Tuley EA, Westfield LA, Lester-Mancuso TL, Le Beau MM, Sorace JM, et al. Human von Willebrand factor gene and pseudogene: structural analysis and differentiation by polymerase chain reaction. Biochemistry. 1991; 30:253–269. PMID:
1988024.

52. Johansson AM, Hillarp A, Säll T, Zöller B, Dahlbäck B, Halldén C. Large deletions of the PROS1 gene in a large fraction of mutation-negative patients with protein S deficiency. Thromb Haemost. 2005; 94:951–957. PMID:
16363235.

53. Lind-Halldén C, Dahlen A, Hillarp A, Zöller B, Dahlbäck B, Halldén C. Small and large
PROS1 deletions but no other types of rearrangements detected in patients with protein S deficiency. Thromb Haemost. 2012; 108:94–100. PMID:
22627709.
54. Hamasaki N. Unmasking Asian thrombophilia: is APC dysfunction the real culprit? J Thromb Haemost. 2012; 10:2016–2018. PMID:
22905992.

55. Kimura R, Sakata T, Kokubo Y, Okamoto A, Tomoike H, Miyata T. Plasma protein S activity correlates with protein S genotype but is not sensitive to identify K196E mutant carriers. J Thromb Haemost. 2006; 4:2010–2013. PMID:
16961608.

56. Tsuda T, Jin X, Tsuda H, Ieko M, Morishita E, Adachi T, et al. New quantitative total protein S-assay system for diagnosing of protein S type II deficiency: clinical application of the screening system for protein S type II deficiency. Blood Coagul Fibrinolysis. 2012; 23:56–63. PMID:
22157257.
57. Suzuki A, Sanda N, Miyawaki Y, Fujimori Y, Yamada T, Takagi A, et al. Down-regulation of
PROS1 gene expression by 17β-estradiol via estrogen receptor α (ERα)-Sp1 interaction recruiting receptor-interacting protein 140 and the corepressor-HDAC3 complex. J Biol Chem. 2010; 285:13444–13453. PMID:
20200160.
58. Drakenberg T, Ghasriani H, Thulin E, Thämlitz AM, Muranyi A, Annila A, et al. Solution structure of the Ca2+-Binding EGF3-4 pair from vitamin K-dependent protein S: identification of an unusual fold in EGF3. Biochemistry. 2005; 44:8782–8789. PMID:
15952784.

59. Schwede T, Kopp J, Guex N, Peitsch MC. SWISS-MODEL: An automated protein homology-modeling server. Nucleic Acids Res. 2003; 31:3381–3385. PMID:
12824332.

60. Huang M, Furie BC, Furie B. Crystal structure of the calcium-stabilized human factor IX Gla domain bound to a conformation-specific anti-factor IX antibody. J Biol Chem. 2004; 279:14338–14346. PMID:
14722079.

61. Groebke Zbinden K, Banner DW, Ackermann J, D'Arcy A, Kirchhofer D, Ji YH, et al. Design of selective phenylglycine amide tissue factor/factor VIIa inhibitors. Bioorg Med Chem Lett. 2005; 15:817–822. PMID:
15664864.

62. Sasaki T, Knyazev PG, Cheburkin Y, Göhring W, Tisi D, Ullrich A, et al. Crystal structure of a C-terminal fragment of growth arrest-specific protein Gas6. Receptor tyrosine kinase activation by laminin G-like domains. J Biol Chem. 2002; 277:44164–44170. PMID:
12218057.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download