This article has been
cited by other articles in ScienceCentral.
Abstract
Background
Bacterial meningitis is an infectious disease with high rates of mortality and high frequency of severe sequelae. Early identification of causative bacterial and viral pathogens is important for prompt and proper treatment of meningitis and for prevention of life-threatening clinical outcomes. In the present study, we evaluated the value of the Seeplex Meningitis ACE Detection kit (Seegene Inc., Korea), a newly developed multiplex PCR kit employing dual priming oligonucleotide methods, for diagnosing acute meningitis.
Methods
Analytical sensitivity of the kit was studied using reference strains for each pathogen targeted by the kit, while it's analytical specificity was studied using the human genome DNA and 58 clinically well-identified reference strains. For clinical validation experiment, we used 27 control cerebrospinal fluid (CSF) samples and 78 clinical CSF samples collected from patients at the time of diagnosis of acute meningitis.
Results
The lower detection limits ranged from 101 copies/µL to 5×101 copies/µL for the 12 viral and bacterial pathogens targeted. No cross-reaction was observed. In the validation study, high detection rate of 56.4% was obtained. None of the control samples tested positive, i.e., false-positive results were absent.
Conclusions
The Seeplex Meningitis ACE Detection kit showed high sensitivity, specificity, and detection rate for the identification of pathogens in clinical CSF samples. This kit may be useful for rapid identification of important acute meningitis-causing pathogens.
Keywords: Meningitis, Multiplex PCR, Dual priming oligonucleotide
INTRODUCTION
Bacterial meningitis is an infectious disease with high rates of mortality and severe sequelae. Early identification of causative bacterial and viral pathogens is important to enable prompt and appropriate treatment and thereby prevent life-threatening clinical outcomes. Patients with suspected meningitis are generally prescribed antibiotics before hospital admission or cerebrospinal fluid (CSF) collection for examination. However, the administration of antibiotics may render it difficult to culture the causative bacteria, thereby impairing microbiological diagnosis [
1,
2]. To counter this problem, alternative methods of molecular identification, including 16S/23S rRNA gene amplification followed by sequencing and real-time PCR, have been developed. However, the clinical application of such techniques is limited because of the presence of interfering bacterial or viral DNA, time-consuming nature of these assays, and small number of detection channels available on the real-time PCR platform [
3-
7].
These limitations can be overcome by the use of multiplex PCR methods, which enable the rapid and accurate identification of up to 9 bacterial and viral pathogens in clinical samples [
8-
10]. We evaluated the diagnostic value of the newly developed Seeplex Meningitis ACE Detection kit (Seegene Inc., Seoul, Korea), a multiplex PCR kit that uses dual priming oligonucleotide (DPO) methods. This kit detects the 12 most common bacterial and viral pathogens of acute meningitis, namely,
Streptococcus pneumoniae (SP),
Haemophilus influenzae (HI),
Neisseria meningitidis (NM), Group B streptococci (GBS),
Listeria monocytogenes (LM), herpes simplex virus (HSV)-1 and HSV-2, Varicella-zoster virus (VZV), Epstein-Barr virus (EBV), cytomegalovirus (CMV), human herpes virus 6 (HHV-6), and human enterovirus (HEV).
METHODS
1. Seeplex Meningitis ACE Detection kit
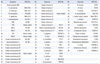
The Seeplex Meningitis ACE Detection kit has 3 components: Seeplex Meningitis-B, which detects 5 bacteria (SP, HI type b, NM, GBS, and LM); Seeplex Meningitis-V1, which detects 6 viruses (HSV-1, HSV-2, VZV, EBV, CMV, and HHV-6); and Seeplex Meningitis-V2, which detects HEV. The Seeplex Meningitis-B and V1 assays amplify DNA, whereas the Seeplex Meningitis-V2 assay amplifies cDNA reverse-transcribed from viral RNA. The target genes amplified from the 12 strains are shown in
Table 1.
2. Multiplex PCR conditions
Each PCR amplification was performed using 5 µL of isolated nucleic acid solution, 2 µL of 10×primer mixture, and 10 µL of 2×Multiplex Master Mix (Seegene Inc.) in a total volume of 20 µL. The amplification protocol was as follows: initial denaturation at 94℃ for 15 min, 40 cycles of denaturation at 94℃ for 30 sec, annealing at 63℃ for 90 sec, and extension at 72℃ for 90 sec. The amplified PCR products were electrophoresed in 2% (w/v) agarose gels and stained with ethidium bromide.
3. Analytical sensitivity and specificity of detection
PCR products were cloned into the vector pUC19 (size, 2,686 bp). The cloned plasmids were harvested, DNA concentrations were measured, and the numbers of target copies were calculated (1 µg of a 1,000-bp DNA unit equals 9.1×10
11 copies). The sensitivity of the system was evaluated by amplifying 10-fold serial dilutions of each plasmid (concentrations, 10
4 to 10
-1 copies/20 µL), with distilled water as the negative control. Samples were PCR-amplified and electrophoresed in 2% (w/v) agarose gels. Analytical sensitivity was defined as the lowest template copy number for which amplified products were consistently detected in triplicate samples. The reference strains used for the 5 bacteria and 7 viruses were as follows: SP ATCC BAA-255D, HI ATCC BAA-1416, NM ATCC 700532D, GBS ATCC BAA-611D, LM ATCC 19114D-5, CMV ATCC VR-807, EBV Korean isolate, HSV-1 ATCC VR-260, HSV-2 ATCC VR-734, VZV Korean isolate, HHV-6 Korean isolate, and HEV ATCC VR-836/VR-784. Primer specificity was assessed by evaluating cross-reactivity with human genomic DNA and 58 reference strains, including 19 HEV species (No.12-30;
Table 2).
4. Verification using clinical CSF samples
1) Specimen collection
Between June and November 2009, 196 clinical CSF samples were collected from 78 patients (27 women, 51 men) diagnosed with acute meningitis on the basis of clinical symptoms and CSF findings (WBC count, distribution of lymphocytes and neutrophils, and glucose level) [
11,
12]. Bacterial meningitis was differentiated from viral or aseptic meningitis by a WBC count of more than 100 cells/mm
3 with neutrophil dominance and a ratio of CSF glucose/serum glucose level of less than 0.4. Cases with insignificant WBC count or discrepant results in different parameters were classified into the undetermined group. The median patient age was 27 yr (range, 1 month to 72 yr). For the verification study, we tested only the 78 samples collected at the time of diagnosis, i.e., before antibiotic therapy was initiated. Another set of 118 samples was used to assess discrepancies in positive results obtained from the same patients. Samples that were blood-colored, showed leakage, were aged over 12 hr, and strongly suspected of being contaminated (with discrepancies in the pathogens detected in consecutive tests), were excluded. All samples were assessed by conventional CSF microscopic analysis, staining, and culture.
Control CSF samples were collected from 27 patients; of these 27 patients, 5 had acute cerebral bleeding; 4, primary or metastatic brain tumors; 4, tuberculous encephalitis; 2, mumps; and 1 each, Cryptococcus neoformans infection, clinically suspected meningitis due to Candida, and rickettsia. The remaining 9 patients showed normal findings.
2) DNA and RNA extraction
CSF specimens were centrifuged at 15,000×g for 5 min. DNA was extracted from both the supernatant and cell pellet by using a nucleic acid purification column according to the manufacturer's instructions (Qiagen Inc., Valencia, CA, USA) and used directly for Meningitis-V1 and Meningitis-B1 testing. RNA was also extracted from each CSF supernatant. cDNA was synthesized by reverse transcription using RevertAid™ First Strand cDNA Synthesis kits (Fermentas, Ontario, Canada) and used for Meningitis-V2 testing.
3) Sequencing
Positive results were confirmed by conventional PCR amplification by using single primer pairs and subsequent sequencing. Amplicons were purified by using a PCR purification kit (SolGent, Daejeon, Korea) and sequenced by using the BigDye Terminator Cycle Sequencing Kit (PE Applied Biosystems, Foster City, CA, USA) and an ABI PRISM 3730XL DNA analyzer (PE Applied Biosystems). Sequences were analyzed using the Basic Local Alignment Search Tool (BLAST) provided by The National Centre for Biotechnology Information (
http://www.ncbi.nlm.nih.gov/BLAST).
RESULTS
The detection sensitivity was the highest for GBS [lower limit of detection (LoD) of 5 genomes/mL] and the lowest for HI (LoD of 57 genomes/mL). The LoDs for HEV, EBV, VZV, HSV-2, HHV-6, NM, CMV, SP, HSV-1, and LM were 10, 11, 11, 12, 12, 13, 16, 19, 38, and 51 genomes/mL, respectively. The analytical sensitivities for all the 12 target pathogens were higher than the 100 copies per reaction stated by the manufacturer. No cross-reaction was evident with human genomic DNA and other reference strains. The Seeplex Meningitis-V2 ACE Detection kit successfully differentiated all the 19 HEV species from the other strains.
CSF samples were obtained from 78 patients at the time of diagnosis of active meningitis and before administration of antibiotic treatment. Among these samples, 44 (56.4%) yielded positive results with the Seeplex kit (
Table 3). Five cases (6.4%) showed positive results for HEV (4) and HSV-1 (1), which were consistent with the results of conventional studies. However, in 2 cases the results were not consistent with the results of conventional studies. One was positive for both LM and EBV in Seeplex Meningitis ACE detection kit, but positive only for LM in the conventional study; the other tested positive for HEV in Seeplex Meningitis ACE detection kit but positive for VZV in the conventional study. Each case presented a bacterial and a viral features, respectively in CSF analysis.
The Seeplex Meningitis ACE detection kit detected causative pathogens for 37 cases (47.4%) that tested negative in the conventional studies. Two patients had single bacterial infection with GBS and LM, and CSF analysis revealed bacterial and undetermined features, respectively. Single viral infections were evident in 16 patients with HEV, 9 with VZV, 3 with HSV-1, and 1 each with HSV-2 and EBV. All the cases with positive results for viruses showed viral or undetermined features in CSF analysis. Five patients showed simultaneous infection with 2 bacterial or viral pathogens: 2 tested positive for both SP and HEV and 1 each tested positive for SP and HSV-1, SP and VZV, and EBV and HSV-1. One of the cases positive for both SP and HEV had CSF findings compatible with bacterial meningitis, while the others had features consistent of viral meningitis, with lymphocyte dominance and high glucose level. Sequencing of amplicons showed no evidence of false-positive cross-reactivity; the rates of BLAST match were 98-100%.
CSF samples obtained from the remaining 34 patients did not test positive with the Seeplex kit. Sequential work-up with conventional studies showed that 1 patient each was infected with EBV, VZV, SP, HEV, and HSV-1 and had consistent CSF findings. The pathogenic agents in the other 29 patients could not be identified, although CSF analysis indicated that 6 had bacterial infection, 13 had viral infection, and the remaining 10 had indeterminate findings. None of the control cases showed false-positive results.
DISCUSSION
Acute meningitis requires prompt treatment to avoid life-threatening clinical outcomes and severe sequelae. Since various viral and bacterial pathogens can cause acute meningitis, the causative agent must be identified before treatment is initiated. Conventional diagnostic tools, including CSF staining, culture, and antigen analysis, have limited diagnostic sensitivity and specificity. This has prompted the development of several molecular methods employing conventional, real-time, or multiplex PCR. Although previously developed multiplex PCR methods can rapidly identify up to 9 bacterial and viral agents, the Seeplex Meningitis ACE detection kit, which employs a DPO method, can identify the 12 most common bacterial and viral agents that cause meningitis: SP, HI, NM, GBS, LM, CMV, HEV, EBV, HSV-1, HSV-2, HHV-6, and VZV. DPOs, which consist of 2 separate priming regions joined by a polydeoxyinosine linker, yield 2 primer segments with distinct annealing properties. The long 5'-segment initiates stable priming, whereas the short 3'-segment controls target-specific extension; the use of these 2 primer segments effectively eliminates non-specific priming and yields consistently high PCR specificity even under less-than-optimal PCR conditions [
13]. This method is highly appropriate for the identification and differentiation of viral and bacterial pathogens with very variable genetic characteristics and low availability of primer sites. Several multiplex PCR kits using the DPO technology have been developed to identify common viral and bacterial pathogens causing respiratory infections and diarrhea, and such kits are currently being used in clinical laboratories [
14-
16].
We found that the Seeplex Meningitis ACE Detection kit offered high sensitivity and specificity for identifying bacterial and viral pathogens in patients diagnosed with acute meningitis. The LoDs for the 12 pathogens ranged from 10-50 copies/µL, and no cross-reaction with human genomic DNA or reference (clinically identified) bacterial and viral pathogens was evident, indicating the high specificity of the kit.
Our validation study revealed that the kit successfully identified pathogens in the CSF samples collected from 44 of the 78 (56.4%) patients who were clinically diagnosed with acute meningitis. Only 6 of the 44 pathogens identified using the Seeplex Meningitis ACE Detection kit were also identified by other laboratory methods, with the pathogen being HEV in 4 cases and HSV-1 and LM in the remaining 2 cases. Six CSF samples were simultaneously positive for 2 pathogens, suggesting co-infection or contamination rather than false-positivity, because subsequent sequencing of PCR products yielded 98-100% matches with sequences in the BLAST database. Of the 12 pathogens assayed, HEV had the highest prevalence and was detected in 23 samples by the Seeplex Meningitis ACE Detection kit. Of the bacterial strains, SP was the most frequently detected; SP was detected in 5 samples, although it was detected along with viruses, including HEV, HSV-1, and VZV, in 4 samples.
Five of the 34 patients, whose samples were negative at the time of diagnosis were later found to have EBV, VZV, SP, HEV, and HSV-1 infection when investigated by conventional studies. These discrepancies were perhaps attributable to inter-specimen differences at varying stages of infection. Of the other 29 patients who tested negative for all pathogens, 10 had indeterminate CSF parameters, whereas 19 showed findings consistent with bacterial or viral infection. The presence of clinical features of meningitis and indeterminate CSF findings in the 10 patients may be attributed to conditions other than acute viral or bacterial meningitis. In contrast, meningitis in the 19 patients with CSF findings consistent with bacterial or viral infections may have been caused by pathogens other than the 12 assayed by the Seeplex Meningitis ACE Detection kit. Alternatively, the concentration of pathogens in the CSF may have been too low to permit detection.
In conclusion, the Seeplex Meningitis ACE Detection kit showed high sensitivity and specificity for the 12 most common bacterial and viral agents causing acute meningitis. A high detection rate was observed in the CSF samples obtained from patients clinically diagnosed with acute meningitis. This kit may enable the rapid identification of pathogens in patients with acute meningitis.






 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download