Abstract
Background
We compared the LightCycler MRSA advanced test (Roche Diagnostics, Germany) with enrichment culture methods to evaluate the relative diagnostic performance of the LightCycler MRSA advanced test for active surveillance in a high-prevalence setting.
Methods
A total of 342 nasal swab specimens were obtained from patients in the intensive care unit at admission and on the seventh day for follow-up. The results of LightCycler MRSA advanced test were compared to those of the enrichment culture. For discrepant results, mecA gene PCR was performed.
Results
For the detection of methicillin-resistant Staphylococcus aureus (MRSA), the LightCycler MRSA advanced test showed 98.5% sensitivity and 78.6% specificity and had positive and negative predictive values of 75.0% and 98.8%, respectively. A total of 46 samples had discrepant results between the LightCycler MRSA advanced test and enrichment culture. Of the 44 specimens that were positive in the LightCycler MRSA advanced test but negative by enrichment culture, mecA genes were detected in 37 specimens. In addition, of the original 44 cases, 21 patients had a history of MRSA colonization or infection within the last month; of those 21 specimens, 20 were positive for mecA gene as shown by PCR. Seven mecA-negative discrepant specimens comprised 3 methicillin-sensitive S. aureus-culture positive and only 2 patients had MRSA infections.
Methicillin-resistant Staphylococcus aureus (MRSA) is one of the major nosocomial pathogens, causing a wide spectrum of infections. In the acute care hospital setting, MRSA colonization is associated with a higher risk of nosocomial infection and increased hospital costs. Reduction of MRSA colonization is the most effective measure for preventing dissemination of MRSA [1]. Therefore, a rapid and sensitive detection method to identify MRSA carriers is crucial in MRSA infection control. Active surveillance cultures for MRSA are now part of clinical practice recommendations both in Europe and the United States [2]. Studies have shown that approximately 0.2-7% of the population is colonized with MRSA [3, 4]. However, the S. aureus nasal carriage rate among healthcare workers in Korea was reported to be as high as 42.2%, and 44% of S. aureus strains was MRSA [5]. A previous study has reported that the prevalence of MRSA colonization at an intensive care unit in Korea was 36.2% [6].
The conventional culture method is time consuming for active surveillance in order to reduce MRSA colonization. Several chromogenic and differential MRSA selective agars have been shown to yield results within 18 to 24 hr [7-9]. Moreover, several real-time PCR methods have been developed and evaluated for same-day detection of MRSA directly from clinical samples [10-12]. The LightCycler MRSA advanced test (Roche Diagnostics, Mannheim, Germany) has recently been developed as a qualitative molecular diagnostic test that simultaneously detects the staphylococcal cassette chromosome mec (SCCmec) (carrying the mecA gene) and an S. aureus-specific sequence located within the orfX gene. This test is used for the direct detection of nasal colonization by MRSA. It is reported that the LightCycler MRSA advanced test had a sensitivity of 95.2% and a specificity of 96.4% [13].
The performance characteristics of the LightCycler MRSA advanced test compared with culture in a high prevalence area have not been sufficiently well studied, and as our institution has been performing active nasal surveillance of MRSA in medical and surgical patients from the intensive care unit, we aimed to compare the LightCycler MRSA advanced test with enrichment culture methods to evaluate the diagnostic performance of the LightCycler MRSA advanced test for active surveillance in high-prevalence settings.
The study was conducted prospectively in a 650-bed teaching hospital (Dongguk University Ilsan Hospital, Korea). A total of 342 nasal swab specimens were obtained from 193 patients admitted to the surgical and medical intensive care units between July 2009 and March 2010. Anterior nasal specimens were obtained from patients at admission and at the seventh day of follow-up by using BD CultureSwab Liquid Stuart (Becton Dickinson Diagnostic Systems, Sparks, MD, USA). For each patient, 2 swabs were rubbed inside the anterior nares, first on one side and then on the other, yielding a paired swab sample. The swab was transported at room temperature and stored at 2℃ until processing, which was performed within 24 hr of collection.
For enrichment culture, one of the paired swabs from each nasal specimen was inoculated in 3 mL of trypticase soy broth (Becton Dickinson Diagnostic Systems) supplemented with 6.5% NaCl. The enrichment broth was incubated for 24 hr at 35℃ and subcultured in 5% sheep blood agar plates (Becton Dickinson Diagnostic Systems) as well as mannitol salt agar and then incubated for 24 hr at 35℃. Presumptive S. aureus colonies were identified as S. aureus by a catalase test and Staphaurex Plus (Remel, Lenexa, KS, USA). Methicillin resistance was determined with an oxacillin disk (Becton Dickinson Diagnostic Systems). The BD Phoenix automated microbiology system (Becton Dickinson Diagnostic Systems) and Phoenix SMIC/ID-100 panel (Becton Dickinson Diagnostic Systems) were used to reconfirm the species identification and methicillin resistance of any specimens that showed discrepant results between the enrichment culture and the LightCycler MRSA advanced test. When all tests were completed, the isolates were frozen at -70℃ in trypticase soy broth with 10% glycerol.
The second swab was processed and tested using the LightCycler MRSA advanced test according to the manufacturer's instructions. The swab was broken off into a lysis tube, incubated in a 95℃ dry block for 2 min, subjected to a vortex in the MagNA Lyser instrument for 70 sec at a speed of 5,000 rpm, and then centrifuged at 10,000×g for 1 min. The supernatant was used directly in real-time PCR. A total of 15 µL of the reconstituted master mix and 5 µL of the lysate solution were added to the capillary. Capillaries were centrifuged briefly and transferred to the LightCycler 2.0 Instrument (Roche Diagnostics) for PCR amplification. The results were obtained in approximately 1 hr. Positive and negative controls were included in each run. After the testing, the lysis tubes were frozen and stored at -70℃.
The PCR results for the LightCycler MRSA advanced test were interpreted using the LightCycler software, which uses a decisional algorithm to interpret the assay result as negative (i.e., no MRSA DNA detected), positive (i.e., MRSA DNA detected), or invalid (i.e., no internal control detected). The LightCycler MRSA advanced test was repeated when specimens yielded invalid results.
The presence of the mecA gene was confirmed for colony and lysates with discordant results (enrichment culture, LightCycler MRSA advanced test) using the mecA gene PCR kit (Seegene, Seoul, Korea). The mecA gene PCR was performed according to the manufacturer's instructions.
The results of LightCycler MRSA advanced test were compared to those obtained using enrichment cultures. When the results of the enrichment culture and the LightCycler MRSA advanced test did not correspond, frozen isolates were thawed and recultured, and the frozen lysates were thawed. The next steps included (i) direct testing of the S. aureus colonies with the LightCycler MRSA advanced test and (ii) testing of the S. aureus colonies and lysates by using the mecA gene PCR kit.
Prevalence of the nasal colonization of MRSA in patients was calculated using results of the enrichment culture. Results of the LightCycler MRSA advanced test were compared to those of the enrichment culture results. The concordance rate, sensitivity, specificity, and negative and positive predictive values of the LightCycler MRSA advanced test were calculated.
The medical charts of patients with a negative enrichment culture but a positive LightCycler MRSA advanced test result were reviewed to collect information on MRSA colonization, MRSA infection, or use of vancomycin/teicoplanin/linezolid in the treatment of MRSA infection documented within 1 month before the study.
MRSA was recovered by culture in 39.2% (134/342) of nasal surveillance specimens in the intensive care unit. In comparison, 51.5% (176/342) of the specimens were MRSA positive as shown by the LightCycler MRSA advanced test. The MRSA prevalence at the time of admission was 27.5% by culture and 33.2% by LightCycler MRSA advanced test.
Seven of the original 342 nasal specimens (2%) showed invalid results in the initial LightCycler MRSA advanced test due to internal control failure. Five of these were correctly identified after a retest of the LightCycler MRSA advanced test, and 2 unidentified PCR specimens (0.6%) were excluded from the data analysis.
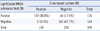
The overall agreement between the LightCycler MRSA advanced test and the enrichment culture was 86.5% (Table 1). Compared to the enrichment culture, the LightCycler MRSA advanced test had a sensitivity of 98.5% (95% confidence interval [95% CI]; 96.4-100), specificity of 78.6% (95% CI; 73.0-84.2), positive predictive value of 75.0% (95% CI; 68.6-81.4), and negative predictive value of 98.8% (95% CI; 97.1-100).
A total of 46 samples had discrepant results between the LightCycler MRSA advanced test and the enrichment culture. Among 46 specimens, 44 specimens were found to be positive by the LightCycler MRSA advanced test but negative by enrichment culture. A discrepancy analysis using the mecA gene PCR revealed the presence of the mecA gene in 37 of the 44 cases (Table 2). Among 44 specimens, methicillin-sensitive S. aureus (MSSA) was detected by culture in 6 cases. Two of the 46 discrepant specimens, which were negative for the LightCycler MRSA advanced test, were positive in the enrichment culture and had the mecA gene, as determined by mecA gene PCR of the lysates and colony. The results of these 2 specimens were considered false-negative results of the LightCycler MRSA advanced test.
The medical charts of the 44 patients that showed positive LightCycler MRSA advanced test results, but negative enrichment culture results, indicated that 21 specimens were obtained from patients with a MRSA colonization or infection history within the month before the study. Moreover, 20 of these 21 specimens were found to be positive for mecA by mecA gene PCR testing of the lysates. Vancomycin, teicoplanin, or linezolid was used in treatment of MRSA infection documented within the last month in 7 patients.
The LightCycler MRSA advanced test was developed in order to detect MRSA strains of different molecular sequences in the vicinity of the right extremity junction of the SCCmec cassette with the orfX gene. This design prevents a false-positive signal from specimens containing MSSA and methicillin-resistant coagulase-negative staphylococci mixed flora [11].
Seven of the original 342 nasal specimens (2%) had an initial invalid LightCycler MRSA advanced test. After PCR was repeated with the same lysate, 5 of these specimens were identified. There were no major changes to the procedure upon repeat PCR. The fact that there were 2 unidentified PCR specimens (internal-control failure) indicates slight PCR inhibition [14]. Therefore, initial invalid results could be attributed to technical problems or the presence of a PCR inhibitor arising from differences in collection procedures [15].
We compared the LightCycler MRSA advanced test results to enrichment cultures used to identify MRSA nasal colonization in this high-prevalence intensive care unit setting. The prevalence of MRSA among nasal isolates was 27.5%. In other intensive care units in Korea, the MRSA colonization prevalence in patients was reported to be 11.6% and 36.2% [6, 16]. Differences in the standard method for recovery of MRSA and collection time of the specimen could be the cause of diverse prevalence. Our findings demonstrate a high prevalence of MRSA colonization in patients admitted to an intensive care unit in Korea.
Compared to the enrichment culture, the sensitivity and negative predictive value of the LightCycler MRSA advanced test in our study were 98.5% and 98.8%, respectively. In 2 cases, the LightCycler MRSA advanced test yielded false-negative results. The discordant results obtained when PCR assay yielded negative results, while the cultures were actually positive, could be related to low bacterial load on the original swab or kit-related problems during extraction of DNA from some isolates [17, 18].
We found that the LightCycler MRSA advanced test had a specificity of 78.6% (162/206), which differs from the findings of Peterson et al., who studied the performance evaluation of the LightCycler MRSA advanced test in hospital non-intensive care unit settings and reported a specificity of 96.8% [13]. In our study, 44 MRSA strains were classified as MRSA by the LightCycler MRSA advanced test, but as MSSA or no growth of S. aureus by the enrichment culture. Although the interpretation of these 44 PCR results is unclear, there are a few possible explanations.
Among the 44 cases, 37 specimens contained the mecA determinant. Positivity of both the LightCycler MRSA advanced test and mecA PCR of the lysate could be false positive owing to MSSA strains harboring remnants of SCCmec plus methicillin-resistant coagulase-negative Staphylococcus (MRCNS) or dead MRSA. It is reported that phenotypic MSSA that are genotypic MRSA isolates containing mecA may require the inactivation of the mecI repressor gene before expression [19]. False positives in the MRSA gene assay are reported to be caused by the assay's potential to amplify retained segments of the right-junction sequence of the SCCmec in S. aureus strains that are missing the mecA gene [11, 20, 21]. We considered the possibility that MSSA harboring remnant SCCmec influenced the false-positive rate, but we found only 6 MSSA strains by culture. Three of them were positive for mecA gene PCR of the lysates and, possibly, the MSSA strains harboring remnant SCCmec combined with MRCNS.
Among the 21 specimens obtained from patients with MRSA colonization or a history of infection within a month prior to this study, 20 were positive for mecA as determined by mecA gene PCR of the lysates. Vancomycin, teicoplanin, or linezolid was used in treatment of MRSA infection in 7 patients. In these cases, the positivity of the LightCycler MRSA advanced test could be explained by the presence of DNA from noncultivable MRSA strains in the specimen [11, 17, 22]. Of the 37 specimens, 3 were obtained from patients with MSSA colonization or a history of infection within a month prior to this study. In these cases, the positivity of the LightCycler MRSA advanced test could be explained by the presence of DNA from noncultivable MSSA harboring remnant SCCmec combined with MRCNS. In the clinical setting of high MRSA prevalence, it is postulated that the main disadvantages of PCR assays are the possibility of the detection of residual DNA from nonviable bacteria [6]. Eleven of the 37 cases with positivity of both the LightCycler MRSA advanced test and mecA gene PCR of the lysate could not be explained by the above mentioned hypothesis. Another explanation for the discordant results could be that a molecular test has a higher sensitivity than the standard culture method used at our institution [17, 23]. Interestingly, within 14 days, 2 patients showed MRSA colonization or infection; these 2 cases could be true-positive results.
Seven of the 44 cases showed positive results for the LightCycler MRSA advanced test and negative results for mecA gene PCR of the lysate. Among 7 cases, 3 were found to be positive for MSSA colonization by enrichment culture. One patient showed a history of MRSA infection within the last month, and one had an MRSA infection within 14 days.
Given the low specificity of real-time PCR for MRSA detection, a possible scenario may be to provide an enrichment culture confirmation of positive LightCycler MRSA advanced test results. However, this adds costs and complexity to the testing algorithms [21]. A high sensitivity of any MRSA surveillance test may be desirable, since the goal of an MRSA program is to rapidly detect all patients with this potential pathogen.
In conclusion, the LightCycler MRSA advanced test was as sensitive as enrichment cultures, but positive results required confirmation with culture method because of low specificity of the MRSA method. In a setting of higher MRSA colonization rate, this drawback would constitute a bigger problem, indicating the need for further studies to definitively ascertain whether the higher costs of PCR assays and the larger number of isolated colonized patients are offset by cost savings from reduced transmission of MRSA in high-prevalence settings.
Figures and Tables
References
1. Cosgrove SE, Qi Y, Kaye KS, Harbarth S, Karchmer AW, Carmeli Y. The impact of methicillin resistance in Staphylococcus aureus bacteremia on patient outcomes: mortality, length of stay, and hospital charges. Infect Control Hosp Epidemiol. 2005. 26:166–174.
2. Muto CA, Jernigan JA, Ostrowsky BE, Richet HM, Jarvis WR, Boyce JM, et al. SHEA guideline for preventing nosocomial transmission of multidrug-resistant strains of Staphylococcus aureus and enterococcus. Infect Control Hosp Epidemiol. 2003. 24:362–386.
3. Salgado CD, Farr BM, Calfee DP. Community-acquired methicillin-resistant Staphylococcus aureus: a meta-analysis of prevalence and risk factors. Clin Infect Dis. 2003. 36:131–139.
4. Wertheim HF, Melles DC, Vos MC, van Leeuwen W, van Belkum A, Verbrugh HA, et al. The role of nasal carriage in Staphylococcus aureus infections. Lancet Infect Dis. 2005. 5:751–762.
5. Park BG, Lee MK. Nasal Carriage of Methicillin-Resistant Staphylococcus aureus among Healthcare Workers and Community Students in 1997 and 2006. Korean J Nosocomial Infect Control. 2007. 12:85–90.
6. Park SH, Jang YH, Sung H, Kim MN, Kim JS, Park YJ. Performance evaluation of BD GeneOhm MRSA PCR assay for detection of nasal colonization of methicillin-resistant Staphylococcus aureus at endemic intensive care units. Korean J Lab Med. 2009. 29:439–447.
7. Diederen B, van Duijn I, van Belkum A, Willemse P, van Keulen P, Kluytmans J. Performance of CHROMagar MRSA medium for detection of methicillin-resistant Staphylococcus aureus. J Clin Microbiol. 2005. 43:1925–1927.
8. Nahimana I, Francioli P, Blanc DS. Evaluation of three chromogenic media (MRSA-ID, MRSA-Select and CHROMagar MRSA) and ORSAB for surveillance cultures of methicillin-resistant Staphylococcus aureus. Clin Microbiol Infect. 2006. 12:1168–1174.
9. Boyce JM, Havill NL. Comparison of BD GeneOhm methicillin-resistant Staphylococcus aureus (MRSA) PCR versus the CHROMagar MRSA assay for screening patients for the presence of MRSA strains. J Clin Microbiol. 2008. 46:350–351.
10. Reischl U, Linde HJ, Metz M, Leppmeier B, Lehn N. Rapid identification of methicillin-resistant Staphylococcus aureus and simultaneous species confirmation using real-time fluorescence PCR. J Clin Microbiol. 2000. 38:2429–2433.
11. Huletsky A, Giroux R, Rossbach V, Gagnon M, Vaillancourt M, Bernier M, et al. New real-time PCR assay for rapid detection of methicillin-resistant Staphylococcus aureus directly from specimens containing a mixture of staphylococci. J Clin Microbiol. 2004. 42:1875–1884.
12. Safdar N, Narans L, Gordon B, Maki DG. Comparison of culture screening methods for detection of nasal carriage of methicillin-resistant Staphylococcus aureus: a prospective study comparing 32 methods. J Clin Microbiol. 2003. 41:3163–3166.
13. Peterson LR, Liesenfeld O, Woods CW, Allen SD, Pombo D, Patel PA, et al. Multicenter evaluation of the LightCycler methicillin-resistant Staphylococcus aureus (MRSA) advanced test as a rapid method for detection of MRSA in nasal surveillance swabs. J Clin Microbiol. 2010. 48:1661–1666.
14. Paule SM, Hacek DM, Kufner B, Truchon K, Thomson RB Jr, Kaul KL, et al. Performance of the BD GeneOhm methicillin-resistant Staphylococcus aureus test before and during high-volume clinical use. J Clin Microbiol. 2007. 45:2993–2998.
15. Bischof LJ, Lapsley L, Fontecchio K, Jacosalem D, Young C, Hankerd R, et al. Comparison of chromogenic media to BD GeneOhm methicillin-resistant Staphylococcus aureus (MRSA) PCR for detection of MRSA in nasal swabs. J Clin Microbiol. 2009. 47:2281–2283.
16. Kim OS, Yoon SW, Kang YJ, Kim YK, Lee NY, Lee JH, et al. Rate of nasal colonization of Methicillin-Resistant Staphylococcus aureus at admission to a medical intensive care unit. Korean J Nosocomial Infect Control. 2007. 12:42–49.
17. de San N, Denis O, Gasasira MF, De Mendonca R, Nonhoff C, Struelens MJ. Controlled evaluation of the IDI-MRSA assay for detection of colonization by methicillin-resistant Staphylococcus aureus in diverse mucocutaneous specimens. J Clin Microbiol. 2007. 45:1098–1101.
18. Rossney AS, Herra CM, Fitzgibbon MM, Morgan PM, Lawrence MJ, O'Connell B. Evaluation of the IDI-MRSA assay on the SmartCycler real-time PCR platform for rapid detection of MRSA from screening specimens. Eur J Clin Microbiol Infect Dis. 2007. 26:459–466.

19. Martineau F, Picard FJ, Lansac N, Ménard C, Roy PH, Ouellette M, et al. Correlation between the resistance genotype determined by multiplex PCR assays and the antibiotic susceptibility patterns of Staphylococcus aureus and Staphylococcus epidermidis. Antimicrob Agents Chemother. 2000. 44:231–238.
20. Donnio PY, Oliveira DC, Faria NA, Wilhelm N, Le Coustumier A, de Lencastre H. Partial excision of the chromosomal cassette containing the methicillin resistance determinant results in methicillin-susceptible Staphylococcus aureus. J Clin Microbiol. 2005. 43:4191–4193.
21. Farley JE, Stamper PD, Ross T, Cai M, Speser S, Carroll KC. Comparison of the BD GeneOhm methicillin-resistant Staphylococcus aureus (MRSA) PCR assay to culture by use of BBL CHROMagar MRSA for detection of MRSA in nasal surveillance cultures from an at-risk community population. J Clin Microbiol. 2008. 46:743–746.
22. Donnio PY, Fevrier F, Bifani P, Dehem M, Kervegant C, Wilhelm N, et al. Molecular and epidemiological evidence for spread of multiresistant methicillin-susceptible Staphylococcus aureus strains in hospitals. Antimicrob Agents Chemother. 2007. 51:4342–4350.
23. Drews SJ, Willey BM, Kreiswirth N, Wang M, Ianes T, Mitchell J, et al. Verification of the IDI-MRSA assay for detecting methicillin-resistant Staphylococcus aureus in diverse specimen types in a core clinical laboratory setting. J Clin Microbiol. 2006. 44:3794–3796.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download