Abstract
Robinsoniella peoriensis has recently been identified as a Gram-positive, spore-forming, anaerobic rod originally recovered from swine manure storage pits. To date, 6 cases of R. peoriensis infection have been reported, including 2 cases of bacteremia, 1 of abdominal fluid collection, and 3 of wound infection. In the present study, we report a 76-yr-old man with R. peoriensis bacteremia who developed aspiration pneumonia. Gram staining of a purified colony revealed Gram-positive, rod-shaped bacteria. Biochemical identification using API 20 A (bioMérieux, France) indicated presence of Clostridium spp. We performed both 500-bp and full-gene sequencing of 16S rRNA of the isolate. The sequence was analyzed with MicroSeq ID 16S rRNA Library v2.0 (Applied Biosystems, USA), GenBank Basic Local Alignment Search Tool (BLAST) (http://www.ncbi.nlm.nih.gov/genbank), and EzTaxon database v2.1 (http://www.eztaxon.org). The 500-bp 16S rRNA sequence of the blood culture isolate showed 99.16-99.79% similarity with R. peoriensis and the full-gene 16S rRNA sequence showed 98.87-99.50% similarity with R. peoriensis. The organism was confirmed as R. peoriensis by using all of the mentioned databases except for MicroSeq, which did not include the RNA sequence of this bacterium. This case suggests that identification of R. peoriensis might be challenging in clinical laboratories with no access to molecular methods, as certain commercial identification systems may not identify, or may misidentify, this organism. To the best of our knowledge, this is the first report of the isolation of R. peoriensis in Korea.
In 2009, Robinsoniella peoriensis was identified as a Gram-positive, spore-forming, anaerobic rod originally recovered from swine manure storage pits. Although anaerobic bacteria have been shown to play a role in all types of infection in humans, certain infections are notable for the prominent role played by anaerobes. These include brain abscesses, chronic sinusitis and otitis media, oral and dental infections, neck space infections, bite infections, lung abscesses, aspiration pneumonia, empyema, intra-abdominal infections of all types, abdominal surgical wound infections, female genital tract infections of all types, various superficial and deep soft tissue infections, and osteomyelitis [1]. Laboratory diagnosis of anaerobic infections is dependent on the recovery of etiological agents from clinical samples. Peptostreptococcus, Fusobacterium, Prevotella, and Bacteroides spp. are the most common anaerobes [2]. To date, 6 cases of R. peoriensis infection have been reported in Europe, United States, and China, including 2 cases of bacteremia, 1 of abdominal fluid collection, and 3 of wound infection [3-5]. R. peoriensis has not previously been reported in Korea. We describe here a case of R. peoriensis bacteremia in a 76-yr-old man with aspiration pneumonia. The identification was confirmed by both partial 500-bp and nearly complete 16S rRNA sequence.
A 76-yr-old man was admitted for the chief complaint of general weakness, cough, and sputum. He had a 7-yr history of middle cerebral artery infarct, which was first diagnosed in 2003. Initial vital signs were as follows: blood pressure, 111/69 mmHg; pulse rate, 87/min; respiratory rate, 21/min; and body temperature, 37.2℃. Initial laboratory test results were as follows: Hb, 15.0 g/dL; white blood cell count, 9.9×109/L (neutrophils, 79.1%; lymphocytes, 13.2%; monocytes, 4.5%; eosinophils, 2.9%; and basophils, 0.3%); and platelets, 180×109/L. Liver function test results and creatinine and glucose levels were within reference interval. His C-reactive protein level was elevated to 17.0 mg/dL; the culture of respiratory specimen indicated Klebsiella pneumoniae. No aerobic or anaerobic bacteria were isolated at initial blood culture. It was suspected the patient had aspiration pneumonia. Treatment with tazocin and levofloxacin was empirically initiated.
Two weeks later, bronchoscopic examination was performed and methicillin-resistant Staphylococcus aureus was isolated. The patient developed a fever and the previously administered antibiotics were replaced with vancomycin, meropenem, and sulfamethoxazole/trimethoprim. Three weeks after admission, blood culture yielded growth of Gram-positive and rod-shaped bacteria, without obvious spore formation, grown in an anaerobic bottle. The isolate was subcultured on a blood plate anaerobically and aerobically. Two days later, gray-white, smooth, and non-hemolytic colonies of unequal sizes were observed only on the anaerobic blood plate (Fig. 1). Gram staining of a purified colony indicated the presence of Gram-positive and rod-shaped bacteria with ovoid-shaped spores located sub-terminally (Fig. 1). Using API 20 A (bioMérieux, Marcy l'Etoile, France), the isolate was found to be positive for catalase and for acid production from glucose, lactose, saccharose, maltose, xylose, arabinose, and mannitol. It was negative for urease and indole formation, and for acid production from sorbitol. The isolate was identified as Clostridium beijerinckii/butyricum (91.6%). An antimicrobial susceptibility test of the isolate was not performed. Although the patient was treated with several antibiotics and no organisms were grown from follow-up blood culture, fever and respiratory failure developed. The patient died 2 months after admission.
We performed 16S rRNA sequencing. Bacterial suspension was centrifuged at 13,000 rpm for 5 min and added to 200 µL of InstaGene Matrix (Bio-Rad laboratories, Hercules, CA, USA), followed by incubation at 100℃ for 15 min. After centrifugation, the supernatant was utilized for PCR. The amplification reaction mixture consisted of 2.5 µL of 10× buffer, 2 µL of 2.5 mM dNTP, 0.6 units of Taq polymerase (Takara Bio, Shiga, Japan), 10 pmol of each primer, and 2.5 µL of template. Cycling parameters were as follows: 10 min of initial denaturation at 95℃; 35 cycles of 30 sec at 95℃ (denaturation), 30 sec at 60℃ (annealing), 45 sec at 72℃ (extension); and a final 10 min extension at 72℃. The PCR product was treated with ExoSAP-IT reagent (USB Corporation, Cleveland, OH, USA) according to the manufacturer's instructions. Sequencing reaction was performed using BigDye Terminator v3.1 Cycle Sequencing kit (Applied Biosystems, Foster City, CA, USA). The sequence was analyzed using MicroSeq ID 16S rRNA Library v2.0 (Applied Biosystems), GenBank Basic Local Alignment Search Tool (BLAST) (http://www.ncbi.nlm.nih.gov/genbank), and EzTaxon database v2.1 (http://www.eztaxon.org) [6-8].
We obtained a consensus sequence of 475 bp. Using MicroSeq ID 16S rRNA Library v2.0 (Applied Biosystems) the isolate was assigned to Clostridium coccoides (95.38%), Ruminococcusproductus (95.27%), Eubacteriumcontortum (94.89%), Clostridium saccharolyticum (93.15%), and Clostridium symbiosum (92.50%). The 16S rRNA sequence of R. peoriensis was not included in the MicroSeq ID 16S rRNA Library v2.0 (Applied Biosystems). With GenBank BLAST, the isolate showed 99.79% similarity with R. peoriensis strain 0910-06083 and 99.58% similarity with R. peoriensis strain HGUE-09/9434. Blautia producta, Eubacterium contortum, and Eubacterium fissicatena were the next closest matches with similarities of 95.20%, 94.78%, and 94.78%, respectively. When the sequence was submitted to EzTaxon database v2.1, we found the highest similarity with R. peoriensis (99.16%). Clostridium nexile, Eubacterium contortum, Blautia luti, and Clostridium oroticum were the next closest matches, with similarities of 95.72%, 95.48%, 95.39%, and 95.15%, respectively.
A phylogenetic tree based on the 16S rRNA sequences of the isolate and 31 organisms with similarity to the isolate was constructed using the neighbor-joining method (Fig. 2). Phylogenetic and molecular evolutionary analyses were conducted using Molecular Evolutionary Genetics Analysis (MEGA) software version 4.0 (http://www.megasoftware.net) [9]. It showed a subline closely related to Clostridium and Eubacterium spp.
We further amplified the nearly full 16S rRNA sequence with 3 different primer sets and obtained a consensus sequence of 1,415 bp. The 3 different primer sets used for full 16S rRNA gene sequencing were as follows: MSQ-1 (F: 5'-GAAGAGTTTGATCATGGCTCAG-3'; R: 5'-ACCGCGGCTGCTGGCAC-3'); MSQ-2 (F: 5'-GGGGAATATTGCACAATGG-3'; R: 5'-TCGCGTTGCATCGAATTAAA-3'); and MSQ-3 (F: 5'-GTAGTCCACGCCGTAAA-3'; R: 5'-TGTGTGAGCACTGCAAAGTA-3'). Using MicroSeq ID 16S rRNA Library v2.0 (Applied Biosystems) the isolate was assigned to Ruminococcus productus (94.17%) and Clostridium saccharolyticum (94.06%). The 16S rRNA sequence of R. peoriensis was not included in the MicroSeq ID 16S rRNA Library v2.0 (Applied Biosystems). With GenBank BLAST, the isolate showed 99.50% similarity with R. peoriensis and Clostridium oroticum (94.38%) was the next closest match. When the sequence was submitted to EzTaxon database v2.1, we found the highest similarity with R.peoriensis (98.87%), whilst Clostridium nexile was the next closest match with a similarity of 94.70%.
As part of a microbiological survey of swine manure, 5 unknown isolates of anaerobic, spore-forming, and Gram-positive bacilli were recovered [10]. Six years after the isolation of these unknown Gram-positive anaerobes, a representative strain was phenotypically and phylogenetically characterized [3]. Phylogenetic analysis showed that this organism was most closely related to Clostridium and Eubacterium spp. R. peoriensis was described as an oval-to-rod-shaped bacterium with sub-terminal spores that grew in 5% CO2 or under anaerobic conditions at 37℃, although the aero tolerance test was negative with our isolate. It produced small and non-hemolytic colonies 0.5-1.5 mm in diameter, and fermented glucose, lactose, and maltose. It did not reduce nitrate or produce indole [3].
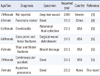
The first report of an isolate of R. peoriensis was in 2009 from the deep heel wound of a 79-yr-old woman [3]. More recently, in 2010, R. peoriensis was isolated from a blood culture of a patient with pancreatic cancer [4]. By 2011, 4 more cases of R. peoriensis isolates in human samples had been reported [5]. To date, a total of 6 cases of R. peoriensis infection have been reported in the literature (Table 1). The underlying conditions and causes included bone fracture, cerebrovascular accident, diverticulitis, and pancreatic cancer. R. peoriensis bacteremia has been previously reported in 2 cases. To our knowledge, this is the first case of infection caused by R. peoriensis in Korea, and the third case of R. peoriensis bacteremia worldwide.
The most common source of anaerobic infections is endogenous normal flora or environmental contamination of wound injuries [11, 12]. R. peoriensis usually colonizes in pig feces and produces a variety of odorous chemicals, which can contaminate local water supplies, resulting in health problems for both animals and humans [3, 10]. In the present case, our patient did not have an obvious history of exposure to pigs or pig manure. R. peoriensis was isolated from 1 anaerobic bottle of 4 blood culture bottles. The pathogenic role of this organism in this patient was unclear. No information about risk factors, infection sites, or organ tropism is currently available for this organism in relation to human infections.
In a clinical setting, this microorganism should be distinguished from closely related ovoid spore-forming organisms such as Clostridium, Ruminococcus , and Eubacterium species. We compared the biochemical characteristics of this isolate with those of the previously reported R. peoriensis (Table 2). This case showed a consistent biochemical profile with the 6 previously reported R. peoriensis organisms for urease; acid production from glucose, lactose, maltose, xylose, and arabinose; and indole formation. Among the 4 previously reported cases with an available biochemical profile for catalase, mannitol, and sorbitol, 1 was positive for catalase, whereas the other 3 were negative. The 4 cases were negative for mannitol. With regard to sorbitol, one report was negative whereas another indicated 2 out of 3 isolates were positive. Current phenotypic identification systems, including API 20 A (bioMérieux), are unable to identify R. peoriensis and may confuse it with other organisms such as Clostridium species. Clostridium beijerinckii/butyricum, the organisms which R. peoriensis was misidentified for using API 20 A (bioMérieux), has biochemical characteristics positive for glucose, lactose, maltose, xylose, and arabinose; negative for catalase and indole formation; and shows negative to weakly positive reaction to mannitol [13]. Our case was biochemically consistent with Clostridium beijerinckii/butyricum, with the exception of positive results for catalase and mannitol, which was not consistent with Clostridium beijerinckii/butyricum. Several unique phenotypic reactions should be included in the API 20 A (bioMérieux) and other commercial systems to enhance identification accuracy. Our study shows that sequencing of 16S rRNA and analysis with various databases are useful tool for the identification of unknown isolates. For R. peoriensis, EzTaxon database v2.1 and GenBank BLAST were superior to MicroSeq ID 16S rRNA Library v2.0 (Applied Biosystems) as they contained the most up-to-date sequences. Although the MicroSeq ID 16S rRNA Library v2.0 (Applied Biosystems) has been experimentally verified and been proven to be useful for routine identification in clinical laboratories [14, 15], it might be unsuitable for identification of novel sequences [16].
In summary, we report one case in which R. peoriensis was isolated from human blood. Identification of R. peoriensis might be challenging in clinical laboratories with no access to molecular methods.
Figures and Tables
Fig. 1
Colonial and microscopic morphology of Robinsoniella peoriensis. (A) Dull white and flat colonies with mixed sizes and smooth edges on an anaerobic blood plate. (B) Gram-positive and rod-shaped bacteria with ovoid-shaped spores located sub-terminally (Gram staining; ×1,000).

References
1. Finegold SM. The role of anaerobes in human infections. Scand J Infect Dis Suppl. 1981. 26:9–13.
2. Kedzia A, Kwapisz E, Wierzbowska M. Incidence of anaerobic bacteria in respiratory tract infections. Pneumonol Alergol Pol. 2003. 71:68–73.
3. Cotta MA, Whitehead TR, Falsen E, Moore E, Lawson PA. Robinsoniella peoriensis gen. nov., sp. nov., isolated from a swine-manure storage pit and a human clinical source. Int J Syst Evol Microbiol. 2009. 59:150–155.
4. Shen D, Chen R, Ye L, Luo Y, Tang YW. Robinsoniella peoriensis bacteremia in a patient with pancreatic cancer. J Clin Microbiol. 2010. 48:3448–3450.
5. Gomez E, Gustafson DR, Colgrove R, Ly T, Santana R, Rosenblatt JE, et al. Isolation of Robinsoniella peoriensis from four human specimens. J Clin Microbiol. 2011. 49:458–460.
6. Hall L, Doerr KA, Wohlfiel SL, Roberts GD. Evaluation of the MicroSeq system for identification of mycobacteria by 16S ribosomal DNA sequencing and its integration into a routine clinical mycobacteriology laboratory. J Clin Microbiol. 2003. 41:1447–1453.

7. Chun J, Lee JH, Jung Y, Kim M, Kim S, Kim BK, et al. EzTaxon: a web-based tool for the identification of prokaryotes based on 16S ribosomal RNA gene sequences. Int J Syst Evol Microbiol. 2007. 57:2259–2261.

8. Devulder G, Perrière G, Baty F, Flandrois JP. BIBI, a bioinformatics bacterial identification tool. J Clin Microbiol. 2003. 41:1785–1787.

9. Tamura K, Dudley J, Nei M, Kumar S. MEGA4: Molecular Evolutionary Genetics Analysis (MEGA) software version 4.0. Mol Biol Evol. 2007. 24:1596–1599.

10. Cotta MA, Whitehead TR, Zeltwanger RL. Isolation, characterization and comparison of bacteria from swine faeces and manure storage pits. Environ Microbiol. 2003. 5:737–745.

11. Brook I, Fraizer EH. Role of anaerobic bacteria in liver abscesses in children. Pediatr Infect Dis J. 1993. 12:743–747.

12. Edmiston CE Jr, Krepel CJ, Seabrook GR, Jochimsen WG. Anaerobic infections in the surgical patient: microbial etiology and therapy. Clin Infect Dis. 2002. 35:S112–S118.

13. Dennis LS, Amy EB, et al. Versalovic J, Carroll KC, Funke G, Jorgensen JH, Landry ML, editors. Clostridium. Manual of clinical microbiology. 2011. 10th ed. Washington, DC: ASM Press;834–857.
14. Lau SK, Ng KH, Woo PC, Yip KT, Fung AM, Woo GK, et al. Usefulness of the MicroSeq 500 16S rDNA bacterial identification system for identification of anaerobic Gram positive bacilli isolated from blood cultures. J Clin Pathol. 2006. 59:219–222.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download