Abstract
Background
Hepatitis C virus (HCV) remains a worldwide health-care burden. Prevalence rates vary and the distribution of genotypes depends on geographical location. Here, the recent prevalence of HCV infections and distribution of HCV genotypes among Korean blood donors were studied.
Methods
Between February 2005 and December 2009, a total of 11,064,532 donors were screened for anti-HCV and 11,412,690 donors were screened for HCV RNA. HCV genotyping was conducted for 748 blood donors with HCV RNA by using the line probe assay (VERSANT HCV Genotype 2.0 Assay, Bayer Healthcare, USA) after amplification of the 5'-untranslated and core regions of the genome.
Results
The anti-HCV prevalence was 0.16% (17,250/11,064,532). HCV RNA was detected in 959 out of the 11,412,690 donors (8.4/100,000). HCV RNA was more prevalent among women, donors who resided at harbor sites, and first-time donors. In addition, the prevalence of HCV RNA increased with age. The genotypes of 740 out of the 748 tested donors (98.9%) were identified. HCV genotype 1b (47.7%) and 2a/2c (35.0%) were dominant. Genotypes 2 (7.6%), 2b (2.3%), 3a (1.6%), 1a (1.3%), 1 (0.9%), 2v (0.5%), 1v (0.1%), and 3 (0.1%) were also identified. Genotype 4a/4c/4d (0.1%) was detected for the first time in one Korean blood donor.
Hepatitis C is a major public health problem in numerous countries [1]. Chronic hepatitis C is the third most common cause of chronic liver disease and hepatocellular carcinoma in Korea, following hepatitis B viral infections and alcohol-induced hepatitis [2]. Blood transfusions have been a leading cause of hepatitis C virus (HCV) transmission. Since 2005, blood donors in Korea have been tested not only for anti-HCV but also for HCV RNA, and an eligible donor selection strategy has been enforced. Since this enforcement, HCV transmission through transfusion has not yet been reported in the Korean population.
The prevalence of anti-HCV antibodies among Koreans older than 40 yr was approximately 1.29% (95% confidence interval, 1.12-1.48%) [3-7]. The latest reported prevalence of anti-HCV in Korean blood donors was 0.1% (Korean Red Cross (KRC), 2010, unpublished data). However, this rate may underestimate the actual prevalence of HCV infections in the general population because donors are generally highly selected [8].
The prevalence of HCV infections confirmed by HCV nucleic acid amplification testing (HCV NAT) was only approximately 0.006% (KRC, 2010, unpublished data), which was much lower than the prevalence reported using anti-HCV testing.
HCV is a single-stranded RNA virus of the Flaviviridae family [9]. HCV is divided into 6 genotypes and numerous sub-genotypes [10]. Striking nucleotide sequence diversity has been reported for HCVs isolated from different geographical areas [11, 12]. The genotypes can have up to 30% nucleotide sequence difference [10, 13]. Different genotypes may respond differently to antiviral treatment [14].
HCV genotypes 1 and 2 (sub-genotype 1b and 2a) are the most dominant genotypes in Korean patients and health examinees [2, 3, 15-21]. Most Korean studies have been performed using small number of samples from a selected population. The purpose of this study was to determine the recent prevalence of HCV infections and the distribution of HCV genotypes among a large number of Korean blood donors.
The study was conducted at the KRC Central Blood Laboratory Center, Seoul. A total of 11,064,532 blood donors were tested for anti-HCV antibodies. HCV NAT was conducted for 11,412,690 donors (including hospital blood centers) between February 2005 and December 2009. Samples with reactive results in the HCV NAT were collected from 3 KRC laboratories (Central, Jung-Bu, Nam-Bu) and stored at -80℃. Of the 959 samples with plasma HCV RNA, only 748 samples could be genotyped in this study (for various reasons). With approval from the KRC Institutional Review Board (4th, 2010), demographics of the HCV infected donors at the KRC (959 HCV RNA reactive donors), including gender, age, and residence site, were reviewed through the Blood Information Management System (BIMS) of the KRC.
All samples were tested for anti-HCV antibodies using the third generation enzyme immunoassay (LG HCD 3.0 TMB, LG Chemical Ltd., Seoul, Korea). Positive hits using this immunoassay were confirmed using the recombinant immunoblot assay (RIBA) (LG HCD confirm, LG Chemical Ltd.).
Two HCV NAT formats were used: Procleix HIV-1/HCV enhanced Semi-Automation System (eSAS, Novartis/Gen Probe, Emeryville, CA, USA) and Ampliscreen bioMerieux combination system using COBAS AmpliScreen HCV Test (Roche Diagnostics, Branchburg, NJ, USA) and NucliSens EasyMag (bioMerieux, Boxtel, The Netherlands).
HCV-RNA was extracted from 200 µL of plasma using the QIAamp MinElute Virus Spin Kit (Qiagen, Hilden, Germany) following the manufacturer's instructions. cDNA was synthesized immediately after RNA extraction. Reverse transcription PCR (RT-PCR) was conducted using the VERSANT HCV Amplification 2.0 Kit (Bayer Healthcare, Tarrytown, NY, USA) and performed using a PTC-100 Thermal Cycler (MJ Research, Waltham, MA, USA). Reverse hybridization (using line probe assay [LiPA] for genotyping of HCV) was performed using the VERSANT HCV Genotype 2.0 assay (INNO-LiPA HCV 2.0, Bayer Healthcare). Before probe hybridization, we evaluated the degree of gene expression using agarose gel electrophoresis of the PCR products (2% agarose, SeaKem LE, Cambrex, Rockland, ME, USA) by comparing the PCR product band with a 100-bp DNA ladder (Promega, Madison, WI, USA). The genotypes (and sub-genotypes) of HCV were identified by comparing the expressed genes on assay strips to a Reading Card, and the results were interpreted according to the guidelines of the manufacturer. The genotypes and sub-genotypes, which can be discriminated by VERSANT HCV Genotype 2.0 assay kit are 1, 1a, 1b, 1a/1b, 2, 2a/2c, 2b, 3, 3a, 3b, 3c, 3k, 4, 4a/4c/4d, 4b, 4e, 4f, 4h, 5a, and 6a/6b.
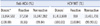
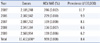
The Anti-HCV repeated reactive rate for blood donors was 0.16% (17,250/11,064,532), and HCV RNA was detected in 959 out of the 11,412,690 (8.4/100,000) blood donors (Table 1). Eighteen of these 959 donors donated blood during the window period. The prevalence (number/100,000) of HCV-infected blood donations decreased from 11.7 in 2005 to 6.2 in 2009 (Table 2). Of the HCV NAT reactive donors, 98.7% (881/893) were also RIBA positive.
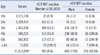
The prevalence of HCV RNA was higher in females than males (10.16/100,000 vs. 7.85/100,000; P=0.0003) and increased with age (P=0.0011) (Table 3).
The prevalence of HCV RNA was higher in donors residing near harbor sites such as Busan and Incheon than in those residing at other sites (15.7/100,000 vs. 7.2/100,000; P<0.0001) (Table 4). First-time blood donors were more likely to test positive for HCV RNA than repeat donors (31.3/100,000 vs. 1.3/100,000; P<0.0001).
The proportion of individuals showing ALT abnormalities (≥65 IU/L) was higher in HCV RNA reactive donors than in the control group (30.2% vs. 1.6%).
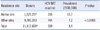
HCV genotypes were determined for 740 of the 748 blood donors (98.9%) (Table 5). The dominant HCV genotypes of Korean blood donors were 1b (357/748, 47.7%) and 2a/2c (262/748, 35.0%); genotype 1 (7/748), 1b, 1a (10/748), and 1v (1/748) constituted 50.1% of the blood donors (375/748); genotype 2 (57/748), 2a/2c, 2b (17/748), and 2v (4/748) constituted 45.5% (340/748). Genotype 3 (1/748) and 3a (12/748) were also observed. Genotype 4a/4c/4d (1/748) was identified in one donor. Eleven donors were co-infected with different subtypes, e.g., 1b+2a/2c (3/748), 1b+1a (2/748), 1b+2 (2/748), 1b+3 (1/748), and 1b+2a/2c+3a (1/748).
The gender, age, and residence site of the donors were not significantly different in donors infected with HCV genotypes 1b and 2a/2c: P=0.106 (gender); P=0.961 (age); P=0.931 (residence site) (Table 6).
Infections in 18 donors, who donated during the window period from 2005 to 2009 could be detected by HCV NAT. The prevalence of anti-HCV (0.16%) and HCV RNA (8.4/100,000) in blood donors did not appear to reflect the true prevalence of HCV infections in the Korean population. According to monthly reports in 2011 (KRC, 2011; unpublished data), the anti-HCV prevalence in a military recruit training center was 0.29%, which was higher than that observed for blood donors (0.16%).
Anti-HCV repeated reactive donors were confirmed by using RIBA supplementary test and HCV NAT screening. Only 5-10% of the anti-HCV repeated reactive donors were estimated to be RIBA positive, and 60-70% of the RIBA-positive donors contained HCV RNA. The true prevalence of HCV infections is thus better defined as the prevalence of HCV NAT-reactive donors. The true prevalence of HCV infections among Korean donors, confirmed by RIBA and HCV NAT is approximately 0.006% (KRC, 2010; unpublished data), which is much lower than the prevalence of anti-HCV.
We evaluated demographics such as the gender, age, residence site, and donation time of the HCV RNA reactive donors at the KRC. We only used donor information provided by the BIMS and did not perform any epidemiologic studies. Elderly donors showed a higher frequency of HCV infection compared with young donors. Exposure to acupuncture has been reported as a significant risk factor for the elderly in rural areas [2]. The reason for the high frequency of HCV RNA in females is unclear. The high frequency of HCV RNA in donors who lived around harbor sites appeared to be associated with environmental factors.
KRC has implemented a healthy donor registry program since 2000 and the program is important for decreasing the prevalence of HCV infections of donors.
HCV is single-stranded RNA virus of approximately 9.4 kb; its gene structure was identified in 1989 by Choo et al. [9, 22]. The classification of HCV into 6 genotypes and approximately 80 sub-genotypes (proposed by Simmonds et al.) is widely used and is based on the nucleotide sequence of NS5 [10]. Methods for HCV genotyping include direct analysis of nucleotide sequences, LiPA, restriction fragment length polymorphism, and restriction fragment mass polymorphism. We used LiPA, a genotyping kit, which is technically simple, cost-effective, and simplifies the interpretation of most HCV genotypes. However, LiPA cannot distinguish between genotype 1b and 1a, between 2c and 2a, and between 4a, 4c, and 4d because of the high homogeneity in the 5'-untranslated regions (UTRs) of different subtypes. Recently, the performance of LiPA reagents for 5'-UTRs was improved by simultaneous amplification of the genomic core region. Thus, the reagents have been upgraded in accordance with the newly classified nomenclature (developed in 2005), thereby mitigating this weakness to some extent [23].
HCV genotypes 1, 2, and 3 are distributed throughout the world. Genotype 4 is mainly found in the Middle East and Africa, and it has recently been identified among European immigrants that moved from Africa or the Middle East; this indicates that the distribution of these viral genotypes is changing because of population redistribution. Genotypes 5 and 6 are found in southern Africa and in Asia, respectively. Genotypes 1b and 2 are dominant in Japan and Taiwan. Genotype 6 is commonly found in Hong Kong, Vietnam, and Laos [1, 12, 24-26]. HCV genotypes 1b and 2a are dominant in Korea. The distribution of HCV genotypes in this study confirmed the results reported previously [2, 3, 15-19]. Although the test kit did not discriminate between 2a and 2c, HCV genotypes 1b (47.7%) and 2a/2c (35.0%) were dominant. Various genotypes such as 1, 1a, 2b, 2, and 2v were also identified. The frequency of genotypes 3 and 3a is still low among Korean blood donors. However, identification of the 4a/4c/4d genotype in one blood donor is intriguing. This donor was a 40-yr-old male with moderately elevated ALT activity (57 IU/L) and with a viral load of 1.2×106 IU/mL. An epidemiological study for investigating the route of HCV infection could not be performed. This case may be the first HCV infection with a 4a/4c/4d genotype in Korean blood donors. Genotype 3 is the dominant genotype among young people; in comparison, genotypes 1 or 2 predominate in USA [27]. Genotypes 1b and 2a/2c are predominant in the elderly [25]. However, other researchers have reported that the age of the donors does not affect the HCV frequency [26]. In this study, genotypes 1b and 2a/2c are less frequent in teenagers compared with the elderly (64.0% vs. 81.5-86.7%); however, this difference is not statistically significant. Fortunately, dominant HCV genotypes among Koreans, including genotypes 1 and 2, respond well to antiviral therapy [2].
In conclusion, periodic studies to determine the prevalence of HCV infections and HCV genotypes in blood donors should be performed to monitor the emergence of new genotypes such as genotype 4a/4c/4d found in this study.
Figures and Tables
References
2. Lim YS. Current status of liver disease in Korea: Hepatitis C. Korean J Hepatol. 2009. 15(Suppl 6):S25–S28.

4. Jeong TH, Jeon TH. PCR prevalence and risk factors of hepatitis C virus infection in the adult population of Ulsan. J Korean Acad Fam Med. 1998. 19:364–373.
5. Seo WT, Lee SS. A study on positive rate of HBsAg, HBsAb and anti-HCV in Korean adults. Korean J Blood Transfus. 1998. 9:259–272.
6. Na HY, Park MH, Park KS, Sohn YH, Joo YE, Kim SJ. Geographic characteristics of positivity of anti-HCV and hepatitis B surface antigen in Kwangju and Chonnam Province: Survey data of 6,790 health screenees. Korean J Gastroenterol. 2001. 38:177–184.
7. Park KS, Lee YS, Lee SG, Hwang JY, Chung WJ, Cho KB, et al. A study on markers of viral hepatitis in adults living in Daegu and Gyungbuk area. Korean J Gastroenterol. 2003. 41:473–479.
8. Alter MJ, Kruszon-Moran D, Nainan OV, McQuillan GM, Gao F, Moyer LA, et al. The prevalence of hepatitis C virus infection in the United States, 1988 through 1994. N Engl J Med. 1999. 341:556–562.

9. Simmonds P. Genetic diversity and evolution of hepatitis C virus -15 yr on. J Gen Virol. 2004. 85:3173–3188.
10. Simmonds P, Bukh J, Combet C, Deléage G, Enomoto N, Feinstone S, et al. Consensus proposals for a unified system of nomenclature of hepatitis C virus genotypes. Hepatology. 2005. 42:962–973.

11. Zein NN. Clinical significance of hepatitis C virus genotypes. Clin Microbiol Rev. 2000. 13:223–235.

12. McOmish F, Yap PL, Dow BC, Follett EA, Seed C, Keller AJ, et al. Geographical distribution of hepatitis C virus genotypes in blood donors: an international collaborative survey. J Clin Microbiol. 1994. 32:884–892.

13. Okamoto H, Kurai K, Okada S, Yamamoto K, Lizuka H, Tanaka T, et al. Full-length sequence of a hepatitis C virus genome having poor homology to reported isolates: comparative study of four distinct genotypes. Virology. 1992. 188:331–341.

14. Mita E, Hayashi N, Hagiwara H, Ueda K, Kanazawa Y, Kasahara A, et al. Predicting interferon therapy efficacy from hepatitis C virus genotype and RNA titer. Dig Dis Sci. 1994. 39:977–982.

15. Suh DJ, Jeong SH. Current status of hepatitis C virus infection in Korea. Intervirology. 2006. 49:70–75.

16. Kwon JH, Bae SH. Current status and clinical course of hepatitis C virus in Korea. Korean J Gastroenterol. 2008. 51:360–367.
17. Shin HR, Hwang SY, Nam CM. The prevalence of hepatitis C virus infection in Korea: pooled analysis. J Korean Med Sci. 2005. 20:985–988.

18. Lee H, Cho YK, Kim HU, Choi EK, Hyun S, Kang D, et al. Distribution of hepatitis C virus genotypes in Jeju Island. Korean J Hepatol. 2008. 14:28–35.

19. Kim YS, Ahn YO, Lee HS. Risk factors for hepatitis C virus infection among Koreans according to the hepatitis C virus genotype. J Korean Med Sci. 2002. 17:187–192.

20. Han CJ, Lee HS, Kim HS, Choe JH, Kim CY. Hepatitis C virus genotypes in Korea and their relationship to clinical outcome in type C chronic liver diseases. Korean J Intern Med. 1997. 12:21–27.

21. Park YS, Lee KO, Oh MJ, Chai YG. Distribution of genotypes in the 5' untranslated region of hepatitis C virus in Korea. J Med Microbiol. 1998. 47:643–647.

22. Choo QL, Kuo G, Weiner AJ, Overby LR, Bradley DW, Houghton M. Isolation of a cDNA clone derived from a blood-borne non-A, non-B viral hepatitis genome. Science. 1989. 244:359–362.
23. Bouchardeau F, Cantaloube JF, Chevaliez S, Portal C, Razer A, Lefrère JJ, et al. Improvement of hepatitis C virus (HCV) genotype determination with the new version of the INNO-LiPA HCV assay. J Clin Microbiol. 2007. 45:1140–1145.

24. Lu L, Nakano T, He Y, Fu Y, Hagedorn CH, Robertson BH. Hepatitis C virus genotype distribution in China: predominance of closely related subtype 1b isolates and existence of new genotype 6 variants. J Med Virol. 2005. 75:538–549.

25. Lee GC, Kim HG, Park NH, Won SY, Chung YH, Lee YS, et al. Distribution of hepatitis C virus genotypes determined by line probe assay in Korean patients with chronic HCV infection. Korean J Hepatol. 1998. 4:244–253.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download