Abstract
Sinus histiocytosis with massive lymphadenopathy, also known as Rosai-Dorfman disease is a rare disorder characterized by proliferation of distinctive histiocytes within lymph node sinuses and lymphatics, sometimes involving extranodal sites. However, clinical suspicion is difficult and there is also a lack of useful diagnostic markers for this disorder prior to histological confirmation. High elevation of serum ferritin is known to be a useful diagnostic marker for various hematologic diseases, including hemophagocytic lymphohistiocytosis and lymphoma. Here, we report a case of fever of unknown origin that presented along with highly elevated serum ferritin (5,780 ng/mL), and was finally diagnosed as Rosai-Dorfman disease by lymph node biopsy.
Sinus histiocytosis with massive lymphadenopathy (SHML), also known as Rosai-Dorfman disease [1], is a rare pathological condition characterized by fever and lymph node enlargement. Sometimes the disease involves extra-nodal sites such as the skin, upper respiratory tract, bone, and retro-orbital tissue [2-6]. Although most patients have prominent bilateral cervical lymph node involvement, some cases do not have such findings and present as fever of unknown origin (FUO). Presently, neutrophilia, high erythrocyte sedimentation rate (ESR), elevation of serum lactate dehydrogenase (LDH), rouleaux formation of red blood cells, polyclonal hypergammaglobulinemia, and hypermetabolism in lymph nodes and spleen on positron emission tomography-computed tomography (PET-CT) [7] are suggestive laboratory findings for the diagnosis. However, a useful, specific marker (prior to pathological diagnosis) suggestive of Rosai-Dorfman disease is still lacking for patients with unexplained fever, lymphadenopathy, or skin rash.
Serum ferritin is a useful marker for the diagnosis of hematologic disorders. Highly elevated serum ferritin (>500 ng/mL) is included in the diagnostic criteria of hemophagocytic lymphohistiocytosis, and is also observed in lymphoma, leukemia, and connective tissue disorders such as systemic lupus erythematosus and adult-onset Still's disease [8]. Recently, the diagnostic utility of ferritin in SHML has been suggested, based on a highly elevated serum ferritin level in a case [9].
Here, we describe a patient with FUO, skin rash, and highly elevated serum ferritin, who was finally diagnosed as having Rosai-Dorfman disease by lymph node biopsy.
A 40-yr-old Korean woman presented with fever and generalized erythematous rash, which had persisted for 17 and 14 days, respectively, prior to her visiting Chonnam National University Hospital (Gwangju, Republic of Korea), a 1,000-bed teaching hospital and referral center. She had visited local clinics and taken levofloxacin and metronidazole for 3 days, and doxycycline for 4 days for suspected uteritis or Tsutsugamushi disease. However, the fever and rash did not improve. She had no history of comorbidity. On physical examination, generalized small macular eruptions on her upper and lower extremities and trunk, palpable bilateral and cervical and inguinal lymph nodes, and fever (38.1℃) were observed. The initial laboratory examination showed a white blood cell count of 10,000/µL (neutrophils 78.1%, eosinophils 1.5%, lymphocytes 13.6%, and monocytes 6.4%); hemoglobin level of 10.1 g/dL, and platelet count of 319×103/µL. Aspartate aminotransferase and alanine aminotransferase were mildly elevated to 90 U/L and 41 U/L, respectively. LDH was elevated to 1,808 U/L; C-reactive protein (CRP), to 9.2 mg/dL; and ESR, to 76 mm/h. Serologic tests for Orientia tsutsugamushi, Leptospira, and Hantaan virus showed negative results. The serum iron level was 11 µg/dL, total iron-binding capacity was 234 µg/dL, and transferrin saturation was <15%, which are compatible with anemia of inflammation. However, the serum ferritin level was elevated to 5,780 ng/mL. Polyclonal hypergammaglobulinemia was also detected (by serum protein electrophoresis). Two sets of blood cultures were performed, but no organisms were isolated. Test results for autoimmune markers, including antinuclear antibody and rheumatoid factor, were negative. A tuberculosis-specific interferon-γ release assay (Quantiferon Tb; Cellestis Limited, Chadstone, Australia) gave a negative result.
Abdominal CT showed mild splenomegaly (maximum diameter, 13.5 cm). Thoracic CT showed scanty bilateral pleural effusion without enhancement or thickening. There was no mass, consolidation, or lymphadenopathy involving the thorax. However, PET-CT showed hypermetabolism in the spleen and lymph nodes in the cervical, abdominal, and inguinal areas (Fig. 1A).
Moderate normocytic normochromic anemia and red cell rouleaux formation were observed on peripheral blood smear examination. Superficial perivascular dermatosis was reported from a skin biopsy. Bone marrow biopsy, including iron staining, showed normocellular marrow and no abnormal findings. Tissue diagnosis for lymphadenopathy was performed using material from the right inguinal lymph node, which had the highest maximum standardized uptake value on PET-CT. Upon histological examination of an excisional lymph node biopsy, SHML was diagnosed (Fig. 1B). Molecular clonality assays for the diagnosis of lymphoma, including immunoglobulin heavy chain gene rearrangement and T-cell receptor rearrangement, showed negative results.
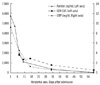
The fever began to subside without medication after 2 weeks of admission. She was discharged on day 18 of hospitalization, and her fever and skin rash were completely resolved. The levels of LDH, ferritin, and CRP also normalized with time (Fig. 2).
SHML, also known as Rosai-Dorfman disease, is a rare disorder of unknown etiology and is usually associated with lymph node enlargement at various superficial or deep sites. It can also involve extranodal sites, commonly the skin, upper respiratory tract, and bone. The involvement of the kidney, lower respiratory tract, or liver has been shown to indicate a poor prognosis. Clinical features of SHML mimic lymphoma, but the prognosis is different. Treatment is not necessary in most cases [10]. However, in the presence of vital organ compression and/or extranodal localization with important clinical signs, surgical debulking, radiotherapy, or chemotherapy are necessary [2].
SHML can be diagnosed by pathologic examination. It should be distinguished from other lymphohistiocytic infiltrative diseases, such as lymphoma, Langerhans cell histiocytosis, hemophagocytic lymphohistiocytosis, and other reactive histiocytosis. SHML shows emperiopolesis on lymph node biopsy and features of immunohistochemical staining that differ from other diseases: SHML is positive for S-100 and negative for CD1a. Although Langerhans cell histiocytosis is also positive for S-100, it is additionally characterized by Birbeck granules and positive staining for CD1a, which are not seen in SHML. And reactive histiocytosis shows no emperiopolesis [9].
Some abnormal laboratory findings, previously reported to be associated with SHML, such as an elevated ESR and polyclonal hypergammaglobulinemia, rouleaux formation of red blood cells and elevation of serum LDH [9], were also observed in the current case. A highly elevated serum ferritin level in a febrile patient limits the diagnostic possibilities to rheumatic disorders and hemato-oncologic disorders [8]. Among the neoplastic etiologies of FUO, highly elevated ferritin levels suggest a myeloproliferative disorder, pre-leukemia, lymphoma, or other lymphoreticular malignancies. Among the rheumatic etiologies of FUO, highly elevated serum ferritin levels are associated with flare of systemic lupus erythematosus, adult-onset Still's disease, or temporal arteritis [8]. The diagnostic utility of ferritin in febrile SHML has been suggested by Cunha et al. [9] based on a highly elevated serum ferritin level in one case. There have been other cases of Rosai-Dorfman disease without elevated or minimally elevated serum ferritin levels [11, 12]. However, in these cases, the patients had no fever when the ferritin was measured. The current case also shows that highly elevated serum ferritin level can be useful for narrowing the differential diagnostic categories and suspicion of SHML in FUO patients. However, the diagnostic usefulness of serum ferritin level in febrile Rosai-Dorfman disease needs to be determined based on data from more cases.
In summary, the current case suggests that Rosai-Dorfman disease should also be suspected in patients with unexplained fever, lymphadenopathy, or skin rash and highly elevated serum ferritin level.
Figures and Tables
 | Fig. 1(A) PET/CT scan. Diffuse hypermetabolism in the spleen (maximum standardized uptake value, 4.6) and hypermetabolism in the neck, inguinal, and intra-abdominal lymph nodes (maximum standardized uptake value, 8.4-10.6) were observed. (B) Histological results of a right inguinal lymph node biopsy. Left upper image: Prominent wide sinuses are observed (shown in the circled area) (H&E stain,×100). Right upper image: These sinuses are composed of histiocytes, lymphocytes, and plasma cells. Histiocytes engulfing lymphocytes are noted (emperiopolesis, indicated by arrow) (H&E stain,×400). Left lower image: On immunohistochemistry, the inter-digitating dendritic cells are positive for S-100 (×100). Right lower image: Biopsied tissue stains negative for CD1a immunohistochemical stain (×100). Lymph node tissue also had cells positive for CD68 and CD163 (antigens positive for monocytes/macrophages).
Abbreviations: PET/CT, positron emission tomography-computed tomography; CD, cluster of differentiation.
|
References
1. Rosai J, Dorfman RF. Sinus histiocytosis with massive lymphadenopathy, a pseudolymphomatous benign disorder. Analysis of 34 cases. Cancer. 1972. 30:1174–1188.
2. Pulsoni A, Anghel G, Falcucci P, Matera R, Pescarmona E, Ribersani M, et al. Treatment of sinus histiocytosis with massive lymphadenopathy (Rosai-Dorfman disease): report of a case and literature review. Am J Hematol. 2002. 69:67–71.

3. Chen J, Tang H, Li B, Xiu Q. Rosai-Dorfman disease of multiple organs, including the epicardium: an unusual case with poor prognosis. Heart Lung. 2011. 40:168–171.

4. Payne JF, Srivastava SK, Wells JR, Grossniklaus HE. Rosai-Dorfman disease simulating nodular scleritis and panuveitis. Arch Ophthalmol. 2011. 129:518–520.

5. Molina-Garrido MJ, Guillén-Ponce C. Extranodal rosai-dorfman disease with cutaneous and periodontal involvement: a rare presentation. Case Rep Oncol. 2011. 4:96–100.

6. Ju J, Kwon YS, Jo KJ, Chae DR, Lim JH, Ban HJ, et al. Sinus histiocytosis with massive lymphadenopathy: a case report with pleural effusion and cervical lymphadenopathy. J Korean Med Sci. 2009. 24:760–762.

7. Hock AT, Long MT, Sittampalam K, Eng DN. Rosai-Dorfman disease: FDG PET/CT findings in a patient presenting with pyrexia and cervical adenopathy. Clin Nucl Med. 2010. 35:576–578.
8. Cunha BA. Fever of unknown origin (FUO): diagnostic importance of serum ferritin levels. Scand J Infect Dis. 2007. 39:651–652.

9. Cunha BA, Durie N, Selbs E, Pherez F. Fever of unknown origin (FUO) due to Rosai- Dorfman disease with mediastinal adenopathy mimicking lymphoma: diagnostic importance of elevated serum ferritin levels and polyclonal gammopathy. Heart Lung. 2009. 38:83–88.
10. Komp DM. The treatment of sinus histiocytosis with massive lymphadenopathy (Rosai-Dorfman disease). Semin Diagn Pathol. 1990. 7:83–86.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download