Introduction
Women with stage IB1 cervical cancer are typically treated by radical hysterectomy and bilateral lymph node dissection. Radical hysterectomy includes removal of the parametrial tissue, as well as a third to half of the upper vagina. The removal of parametrial tissue is important in the treatment of cervical cancer because this area is the most frequently affected site of cancer spread. The tumor can spread to the parametrium through either direct microscopic extension or by tumor embolization from the primary lesion to lymph nodes in the parametrial tissue. The incidence of pathological parametrial involvement has been reported to be between 6% and 31% [
123]. Important prognostic factors in cervical cancer include tumor size, parametrial disease spread, lymphovascular space involvement (LVSI), and lymph node metastasis. However, parametrectomy is the main cause of postoperative complications which may include bladder dysfunction, sexual dysfunction, and anorectal mobility disorders attributable to partial denervation of the autonomic nerve supply to the pelvic organs which may occur during parametrial resection. Although, in the randomized controlled trial about nerve-sparing surgery to minimize these complications, nerve-sparing radical surgery was effective in preserving bladder function without sacrificing oncologic safety [
4], more data is necessary for this issue.
Some authors suggested that less radical surgery should be applied in patient populations with favorable prognostic factors and low risk of parametrial involvement. Kim et al. [
5] reported that stage IB1 patients with superficial invasion (<5 mm) have very low risk of parametrial involvement and thus, less radical surgery may be performed. Kodama et al. [
6] also demonstrated that stage IB1 patients with depth of invasion (DOI) less than 10 mm, no LVSI, and less than 50 years of age should be considered as potential recipients of modified radical hysterectomy, or simple hysterectomy with pelvic lymphadenectomy.
In the present study, we evaluated the clinicopathologic factors associated with pathologic parametrial involvement in patients with stage IB1 cervical cancer. In addition, we identified those patients at low risk for parametrial involvement who may benefit from less radical surgery.
Materials and methods
A retrospective study was performed using a database of patients who underwent type III radical hysterectomy between January 2002 and December 2007 with the approval of the Institutional Review Board. We found that 120 consecutive patients diagnosed with International Federation of Gynecology and Obstetrics (FIGO) stage IB1 were treated with type III radical hysterectomy and pelvic lymph node dissection, either with or without para-aortic lymph node dissection. Patients who received primary radiotherapy and chemotherapy were excluded from our study. Patients with microinvasive carcinoma and patients treated by type I simple hysterectomy or type II modified radical hysterectomy, were also excluded.
The histological diagnosis was made using either punch biopsy or cone excision. Tumor diameter was obtained from the pathological measurements at conization or using the hysterectomy specimen. Radical hysterectomy included complete resection of cervical fascia (anterior parametrium), and uterosacral and rectovaginal ligaments (lateral and posterior parametrium). The pelvic lymphadenectomy consisted of systematic dissection of the common iliac, internal and external iliac vessels, and the obturator nodes both above and below the obturator nerves. Para-aortic lymph node dissection was performed from the level of the aortic bifurcation to the inferior mesenteric artery. The para-aortic nodes were dissected if suspicious pelvic nodes were detected. Pathologic data was collected by review of the pathology report. All hysterectomy specimens were collected and processed in a routine manner. The parametrium was usually defined as the connective tissue of the pelvic floor extending laterally from the fibrous subserous coat between the layers of the broad ligament in the supracervical part of the uterus. The parametrial tissue from all excised specimens was processed and examined to evaluate possible microscopic tumor spread. Abstracted pathologic data included: histologic subtype, depth of tumor invasion, LVSI, parametrial tumor involvement, vaginal or uterine corpus involvement, lymph node status, and status of the margins of resection. DOI and tumor size after conization were not added to those of hysterectomy specimens.
The associations between these pathologic factors and parametrial tumor involvement were evaluated using either χ2 or Fisher exact tests. Multivariate analysis was performed using stepwise logistic regression analysis. A P-value under 0.05 was taken to indicate statistical significance, and all tests were 2-sided. The statistical analysis was performed using SPSS version 12.0 (SPSS Inc., Chicago, IL, USA).
Results
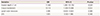
The study population consisted of 120 women with FIGO stage IB1 who underwent radical hysterectomy, and pelvic and/or para-aortic lymph node dissection. Patient characteristics are shown in
Table 1. Overall, 18 (15.0%) cases were observed to include parametrial tumor involvement. The median follow-up period was thirty-seven months (range, 1–81).
Table 1
Clinical characteristics of patients

|
Characteristics |
Patients (n=120) |
|
Age (yr) |
46 (22–77) |
|
DOI (mm) |
9 (2–28) |
|
Tumor size (mm) |
19 (4–75) |
|
Histologic subtype |
|
|
Squamous cell carcinoma |
100 (83.3) |
|
Adenocarcinoma |
15 (12.5) |
|
Adenosquamous |
5 (4.2) |
|
No. of lymph nodes removed |
34 (12–96) |
|
LVSI |
50 (41.7) |
|
Parametrial involvement |
18 (15.0) |
|
Lymph node metastasis |
17 (14.2) |
|
Positive resection margin |
4 (3.3) |
|
Uterine involvement |
10 (8.3) |
|
Vaginal involvement |
11 (9.2) |
|
Adjuvant treatment |
|
|
None |
45 (37.5) |
|
Radiotherapy |
11 (9.2) |
|
Chemotherapy |
37 (30.8) |
|
Chemoradiation |
27 (22.5) |

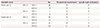
Patients with tumors larger than 2 cm had a 22.5% risk of parametrial involvement, compared with 0% for patients with tumors 2 cm or smaller (
P=0.002). Cases with invasion depths greater than 1 cm were significantly associated with parametrial spread. Patients with invasion depths greater than 1 cm had a 32.7% probability for parametrial tumor spread, while those with invasion depths lesser than or equal to 1 cm had only a 1.5% probability for tumor spread (
P<0.001). Uterine corpus involvement was also significantly associated with parametrial spread. Patients with uterine corpus involvement had a 70.0% probability of parametrial tumor spread, as compared to 10.0% for those without uterine involvement (
P<0.001). Lymph node status correlated highly with parametrial involvement. Parametrial involvement was associated with lymph node metastasis in 52.9% of patients, as compared to 8.7% association with negative lymph nodes (
P<0.001). Patients with LVSI had a 24.0% risk of parametrial involvement as compared to 8.6% of patients with negative LVSI (
P=0.038). Histologic grade and histology subtype had no significant effect on parametrial involvement (
Table 2). However, we had many missing data in histologic grade.
Table 2
Variables associated with parametrial involvement

|
Variables |
Parametrium |
P-value |
|
Negative (n=102) |
Positive (n=18) |
|
Mean age (yr) |
52.3 (22–71) |
55.1 (31–77) |
0.543 |
|
Tumor size (cm) |
|
|
0.002 |
|
≤2 |
40 (100.0) |
0 |
|
>2 |
62 (77.5) |
18 (22.5) |
|
DOI (cm) |
|
|
<0.001 |
|
≤1 |
67 (98.5) |
1 (1.5) |
|
>1 |
35 (67.3) |
17 (32.7) |
|
Corpus involvement |
|
|
<0.001 |
|
Negative |
99 (90.0) |
11 (10.0) |
|
Positive |
3 (30.0) |
7 (70.0) |
|
Vaginal involvement |
|
|
0.060 |
|
Negative |
95 (87.2) |
14 (12.8) |
|
Positive |
7 (63.6) |
4 (36.4) |
|
Resection margins |
|
|
0.096 |
|
Negative |
100 (86.2) |
16 (13.8) |
|
Positive |
2 (50.0) |
2 (50.0) |
|
Lymph nodes |
|
|
<0.001 |
|
Negative |
94 (91.3) |
9 (8.7) |
|
Positive |
8 (47.1) |
9 (52.9) |
|
LVSI |
|
|
0.038 |
|
Negative |
64 (91.4) |
6 (8.6) |
|
Positive |
38 (76.0) |
12 (24.0) |
|
Histologic grade |
|
|
0.395 |
|
Grade 1 |
27 (90.0) |
3 (10.0) |
|
Grade 2 |
30 (78.9) |
8 (21.1) |
|
Grade 3 |
5 (100.0) |
0 |
|
NA |
47 |
|
|
Histologic subtype |
|
|
0.302 |
|
SCC |
83 (83.0) |
17 (17.0) |
|
Non-SCC |
19 (95.0) |
1 (5.0) |

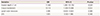
Tumor size more than 2 cm was considered for major factors associated with parametrial involvement, because a subgroup with tumor size smaller than 2 cm showed no parametrial involvement regardless of invasion depth or presence of LVSI. Therefore, multivariate analysis was performed for other clinicopathologic factors most associated with parametrial involvement except tumor size. After controlling for confounding factors, multivariate analysis for other factors showed invasion depth more than 1 cm (odds ratio [OR], 11.5;
P=0.029), and uterine involvement (OR, 10.1;
P=0.022), were significantly associated with parametrial involvement (
Table 3).
Table 3
Multivariate analysis of the risk factors for parametrial involvement
|
Variables |
OR |
95% CI |
P-value |
|
Invasion depth >1 cm |
11.460 |
1.290–101.792 |
0.029 |
|
Corpus involvement |
10.113 |
1.400–73.066 |
0.022 |
|
Lymph node metastasis |
3.499 |
0.826–14.823 |
0.089 |
|
LVSI |
1.925 |
0.502–7.386 |
0.340 |

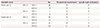
We identified a cohort of women with low risk for parametrial involvement using preoperatively accessible risk factors including tumor size, DOI, and LVSI (
Table 4). There was no parametrial spread for any of the 40 patients with tumor size less than or equal to 2 cm. However, one patient with a tumor size lesser than or equal to 2 cm, an invasion depth more than 10 mm and positive LVSI, had lymph node metastasis. Among the 80 patients with tumor size greater than 2 cm, 20 patients suffered an invasion depth less than or equal to 10 mm, negative LVSI and no parametrial involvement. One patient with a tumor size greater than 2 cm, an invasion depth less than or equal to 10 mm, and positive LVSI, suffered parametrial spread. Among 47 patients with tumor size greater than 2 cm and invasion depth greater than 10 mm, 17 patients had parametrial involvement regardless of LVSI.
Table 4
Relationship of depth of invasion, tumor size, and lymphovascular space involvement to parametrial disease and lymph node metastasis
|
Variables (cm) |
No. |
Parametrial involvement |
Lymph node metastasis |
|
Tumor size ≤2 |
DOI ≤1 |
LVSI (−) |
26 |
0 |
0 |
|
LVSI (+) |
9 |
0 |
0 |
|
DOI >1 |
LVSI (−) |
1 |
0 |
0 |
|
LVSI (+) |
4 |
0 |
1 |
|
Tumor size >2 |
DOI ≤1 |
LVSI (−) |
20 |
0 |
1 |
|
LVSI (+) |
13 |
1 |
1 |
|
DOI >1 |
LVSI (−) |
23 |
6 |
5 |
|
LVSI (+) |
24 |
11 |
9 |

Discussion
In the present study, we found that parametrial involvement occurred with an incidence of 15.0% in patients with FIGO stage IB1 cervical cancer. These findings are higher than those of previous studies which reported parametrial involvement incidences of 8.4%–10.7% in similar patient groups. It is plausible that the higher incidence of parametrial involvement observed in the present study results from the two third of patients (80 out of 120) having a tumor size greater than 2 cm, and patients with less advanced stage IA were included in the results of other studies. In the present study, the portion of chemotherapy only (30.8%) was higher than that of radiotherapy only (9.2%). The patients who received chemotherapy only were patients with intermediate risk factors of Sedlis criteria. According to the National Comprehensive Cancer Network guidelines, in case of absence of high-risk factors, observation or pelvic radiation with or without chemotherapy is recommended as post-operative adjuvant therapy. It is caused by the pattern of our institution for adjuvant treatment in cervical cancer patients with intermediate risk factors after radical surgery.
Spread of disease to parametrial tissue is associated with the size of the primary tumor. Winter et al. [
7] observed that the rate of parametrial involvement increased from 6.7% to 33.0% in tumors 5–20 mL in volume. Therefore, many patients with stage IB1 cervical cancer may be over treated with radical surgery. There is no evidence tying the extent of parametrium resection with prevention of recurrence. Large numbers of IB1 patients with small lesions or favorable prognostic factors are being prescribed unnecessary overtreatment. Kim et al. [
5] reported that stage IB1 patients with DOI less than or equal to 5 mm are at very low risk for parametrial involvement, and those patients are candidates for less radical surgery, omitting parametrectomy. Identification of useful predictors or factors associated with parametrial involvement allows clinicians to decrease the use of parametrial resection and reduce the occurrence and severity of its resultant complications. Using univariate analysis, our study showed that parametrial involvement was indicated with preoperative observations including, a tumor size more than 2 cm, an invasion depth greater than 1 cm, uterine involvement, lymph node metastasis, and positive LVSI. Patients with small tumors, negative LVSI, and invasion depth 1cm or less had a 0% risk for parametrial involvement in the subgroup analysis.
Previous studies including stage IA1–IIA patients have reported that large tumor size, higher histologic grade, presence of LVSI, and positive pelvic lymph nodes are associated with parametrial involvement in early stage of cervical cancer [
689101112]. Large tumor size strongly correlated with parametrial involvement in most previous studies. Kamimori et al. [
9] evaluated parametrial involvement in patients with stage IB1 disease and reported a 5.6% incidence. They suggested that parametrial involvement was found less frequently in patients with tumor diameter 20 mm or less, and preoperative tumor diameters imaged by magnetic resonance imaging (MRI) correlated well with parametrial involvement and other pathologic prognostic factors associated with FIGO stage IB1 cervical cancer. Most previous studies demonstrated that patients with parametrical involvement were more likely to have a primary tumor with a size larger than 2 cm [
9101112]. Wright et al. [
11] found that the incidence of parametrial involvement was only 0.4% in patients with negative nodes, no LVSI, and tumor size less than 2 cm. Frumovitz et al. [
10] also found that there was no evidence of parametrial involvement in patients with primary tumor size less than 2 cm and no LVSI. In the present study, patients with tumor size less than or equal to 2 cm had no parametrial disease involvement, and only one patient with an invasion depth greater than 10 mm and positive LVSI, resulted with lymph node metastasis. A previous study reported that patients with an invasion depth greater than 5 mm had no parametrial disease [
5]. Other investigators have presented 10 mm of invasion depth as the limit associated with parametrial spread [
1613]. They showed that the incidence of parametrial involvement was only 0.6%–1.1% in a subset of patients with 10 mm DOI, and without other prognostic factors.
Positive lymph nodes have been previously reported as predictive of parametrial involvement [
16810111314]. However, our study found that lymph node status was not associated with parametrial involvement by multivariate analysis, yet univariate indicated that lymph node status was associated with parametrial spread. It might be because there are several routes of parametrial involvement such as parametrial lymphovascular invasion, direct invasion, and parametrial lymphatic metastasis in cervical cancer [
15]. van den Tillaart et al. [
16] have found that only 50% of the parametrial invasion lesions are caused by direct invasion, whereas the other 50% of the lesions are not connected with primary lesions, which are distributed over the parametrium randomly. In the group of patients with lesions of pulsatility index that are not connected with primary tumors, van den Tillaart et al. [
16] have found that the metastasis lesions are often in lymph nodes and/or lymph vessels, but are rarely in the blood vessels or isolated lesions. And small number of the present study may be another reason of no association of lymph node metastasis and parametrial involvement in multivariate analysis. Covens et al. [
1] demonstrated that age and grade are also prognostic of parametrial invasion. However in our study, age and histologic grade did not have an association with parametrial disease spread.
Many authors have attempted to identify a cohort of women with early stage cervical cancer who are at low risk for parametrial involvement, and who are potential candidates for less radical surgery [
19101112]. Most of these subsets have tumor sizes smaller than 2 cm, negative lymph nodes, invasion depth less than 10 mm, and negative LVSI. These findings were confirmed by our study. We chose subgroup criteria for parametrial spread to include tumor size, DOI, and LVSI, because these factors can be preoperatively assessed by pathological examination of the cone biopsy specimen or imaging study. We showed that patients with tumor size less than 2 cm had no parametrial disease, regardless of invasion depth or presence of LVSI. Therefore, if clinicians may know the tumor size before surgery by imaging study, it may be helpful to decide less radical surgery. Further investigation is needed.
The justification for complete parametrectomy in stage IB1 disease for all tumor sizes is the assumption that parametrial metastases can occur equally in both the lateral and medial parametrial [
21718]. Less radical surgery, such as type I or II hysterectomy with lymph node dissection, may be a possible alternative in low risk candidates with clinical observations such as small tumor size, negative lymph node, superficial invasion, and negative LVSI. The primary goal of decreasing radical surgery is to prevent intraoperative complications such as ureteric injury, fistulas, blood loss, and long-term complications such as urinary dysfunction [
19]. A randomized study of type II and III radical hysterectomy cases demonstrated no difference in recurrence and survival rate, but the type II hysterectomy group had fewer postoperative complications [
20]. There are other advantages for patients in receiving less radical surgery in terms of shorter operative duration, lower volume of blood transfusion, shorter length of hospital stay, and reduced perioperative morbidity risk [
21].
The limitation of this study is the retrospective nature. Although, retrospective finding of parametrium involvement factor after surgery may be meaningful, these factors are already well-known. And more important point is to find out the factors associated with parametrial involvement before surgery such as preoperative tumor size on MRI.
In conclusion, this study shows the association of parametrial involvement with tumor size, lymph node status, invasion depth, uterine involvement, and LVSI, an association that has also been suggested in many other previous studies. Also, a subgroup with tumor size smaller than 2 cm showed no parametrial involvement, regardless of invasion depth or presence of LVSI, and therefore patients with these observations may be considered for less radical surgery. Stage IB1 patients should be evaluated in a larger, prospective study to include assessment of preoperatively accessible predictors of parametrial involvement, the extent of radical surgery performed, and postoperative complications.






 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download