Introduction
Considering the effects on perinatal morbidity and mortality, preterm labor is one of the most important problems in obstetrics, accounting for more than one-third of all preterm births [
12]. So far, ritodrine and magnesium sulfate are the most commonly used tocolytics for preterm labor. Ritodrine is an approved drug by Korean Food and Drug Administration and is the most commonly used medication as a tocolytics. However, side effects such as palpitations, pulmonary edema, hands tremors, hypokalemia, and hyperglycemia are known to occur [
34]. The Magnesium sulfate is not approved for tocolytics and is used as an off-label drug for a preterm labor, in addition to other purposes such as prevention of eclampsia and prevention of cerebral palsy in premature infants [
5]. Magnesium sulfate may also cause side effects such as nausea and vomiting, lethargy, dyspnea, headache, hypotension, and dizziness [
156]. Therefore, it may be needed to evaluate the safety of magnesium sulfate in comparison with ritodrine.
In terms of efficacy to inhibit uterine contractions, several previous studies have shown that the success rate in inhibiting preterm labor (within 48 hours or within 7 days) was not different between magnesium sulfate and ritodrine [
278]. However, there is a paucity of information regarding the efficacy of both medications after consideration of intra-amniotic infection, although numerous data suggest that intra-amniotic infection is one of the most important prognostic factors in patients of threatened preterm birth [
91011].
The objective of this study was to compare the efficacy and safety of magnesium sulfate with that of ritodrine in preterm labor, and to analyze the factors affecting the efficacy of the drug in patients for the treatment of preterm labor.
Materials and methods
1. Study population
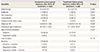
In this retrospective study, pregnant women who were treated with tocolytics (ritodrine or magnesium sulfate) with the diagnosis of preterm labor (24–33.6 weeks of gestation) and underwent amniocentesis to evaluate the presence of infection in the amniotic fluid or fetal lung maturation in Seoul National University Hospital were included between January 2005 and April 2015. Women diagnosed with premature rupture of membrane or pre-eclampsia were excluded. The study population was divided into ritodrine group and magnesium sulfate group according to the type of first-line tocolytics.
2. Definition
Preterm labor was defined as regular uterine contractions, and the choice of first tocolytics drug and the administration dosage of tocolytics was at the discretion of attending physician. Usually ritodrine was administered with an initial dose of 6.4 mg/hr with increment of 3.2 mg/hr every 15 minutes until the cessation of uterine contractions, and magnesium sulfate was given as a 0.004–0.006 g loading dose followed 1.2–3 g/hr of maintenance dose.
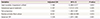
The efficacy of tocolytics was assessed in terms of inhibition of preterm birth within 48 hours, within 7 days, or within 37 weeks of gestation, and the frequency of changing to the second-line therapy was also evaluated. To compare the efficacy of both medications with consideration of other clinical factors, the patients were divided into treatment success group and failure group according to whether they were delivered within 48 hours or not. The gestational age of initiation of tocolytics administration, the gestational age of delivery, the frequency of second-line therapy needed, the duration of medication, the rate of twin pregnancy, maternal age, parity, the presence or absence of amniotic fluid infection, and maternal C-reactive protein (CRP) were compared between 2 groups of cases.
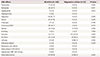
The side effects of the drugs were analyzed in women who used only one tocolytics, and women who needed second-line therapy were excluded from the analysis of side effects. In terms of adverse events, the tachycardia was defined as heart rate exceeding 110 rate/min, the tachypnea was defined as respiration rate exceeding 20 times/min, and the hypokalemia was defined as a plasma potassium level of less than 3.0 mEq/L. Hyperglycemia was defined as the state of above 200 mg/dL blood sugar level regardless of diet. Amniotic fluid infection was defined as a positive result in amniotic fluid culture.
3. Statistical analysis
Statistical analysis was performed using SPSS 23.0 for windows (IBM Corp., Armonk, NY, USA). Mann-Whitney U test was used to examine the differences between the 2 groups in terms of the continuous variables. The χ2 test was used to compare proportions. Multivariate logistic regression was done for analysis risk factors for treatment failure on the basis of significant factor affecting efficacy of tocolytics. P-value <0.05 was considered statistically significant.
Discussion
The principal finding of the current study was; 1) The efficacy (preterm delivery within 48 hours, 7 days, or 37 weeks of gestation and need for 2nd line therapy) was not different between ritodrine and magnesium sulfate; 2) In multivariate analysis, gestational age at treatment, twin gestation, intra-amniotic infection and maternal CRP was associated with treatment failure (preterm delivery within 48 hours), but the type of tocolytics was not significantly associated with treatment failure; 3) The type of side effect was different in the 2 groups, but the frequency of total adverse effect, need for discontinuation of therapy because of maternal adverse effect, and severe adverse effect were not different between the 2 groups of cases.
Until now, several medications have been used in preterm labor, and ritodrine and magnesium sulfate are the most frequently used tocolytics [
4712]. Magnesium sulfate is known to suppress the uterine contraction by antagonism to calcium ions [
5]. Ritodrine is a β-adrenergic agonist that binds to β-sympathetic receptors in the uterine smooth muscle cell membrane and relaxes the uterine smooth muscle by decreasing the concentration of calcium that causes muscle contraction [
12]. However, the problem with β-adrenergic agonists is that β-sympathetic receptors are distributed not only in the uterine muscle but also in the vascular wall, resulting in unintended side effects. The side effects caused by this include maternal cardiovascular side effects, hypokalemia, and hyperglycemia. The most common side effects of ritodrine administration are tachycardia, hypotension, and chest discomfort, but uncommon fatal side effects such as pulmonary edema and myocardial infarction have been reported [
13].
In this study, the safety and efficacy of magnesium sulfate, as an alternative tocolytis, was compared with that of ritodrine. As a result of specific mechanism of action of both tocolytics, side effects related with vital signs such as palpitations, hand tremor, tachycardia, chest discomfort, and tachypnea were significantly more frequent in ritodrine group whereas facial flushing, lethargy, and dizziness were much significantly occurred in magnesium sulfate group. The overall side effects showed different frequency of incidence according to each drug use, but there was no difference in severe side effects, in terms of discontinuation of drug use due to severe side effects and the fatal maternal side effects (maternal death, cardiac arrest, respiratory arrest, and intensive care unit admission). Therefore, it can be concluded that ritodrine and magnesium sulfate are similar in terms of safety.
In addition, in order to evaluate the efficacy of the tocolytics, treatment success (delay of delivery within 48 hours after drug administration) was analyzed. The type of first-line tocolytics (ridodrine vs. magnesium sulfate) was not significant determinant of treatment failure. Therefore, we might conclude that magnesium sulfate as a tocolytics in preterm labor patients is not different from ritodrine in terms of efficacy.
There have been several studies which showed that that the efficacy was not different between magnesium sulfate and ritodrine [
34]. Recently, Hwang et al. [
13] reported multicenter study on the practice pattern in management of threatened preterm labor in Korea. In this study, the effectiveness of ritodrine and magnesium sulfate was similar and the poor tolerance to therapy was comparable between the 2 tocolytics, and these results are consistent with the result of the current study. However, the comparison of efficacy after adjustment for intra-amniotic infection has not been well determined, although numerous studies have suggested that intra-amniotic infection is the major risk factor of preterm delivery [
91011]. In the current study, the efficacy of treatment success was not related to the type of first-line tocolytics, but was influenced by the gestational age of tocolytics administered, twin pregnancy, amniotic fluid infection, and maternal CRP.
This study was based on the retrospective study with patients who underwent amniocentesis among the inpatients due to preterm labor. Therefore, the number of magnesium sulfate used group was relatively small, and the decision on type of tocolytics was at the discretion of attending physician which might result in different indications for both tocolytics and in selection bias (for example, magnesium sulfate might be used as a first-line therapy especially for patients with medical disease such as hyperthyroidism, cardiac disease, or diabetes). Further studies through prospective randomization studies may be needed to evaluate the efficacy and safety of magnesium sulfate.
And about magnesium sulfate, there are 2 more important points. Magnesium sulfate has a neuroprotective effect for preterm birth before 32 weeks of gestation. So we should consider magnesium sulfate especially for patients who have high risk for preterm birth within 32 weeks [
5]. In addition, the concerns on its adverse effect of fetal bone should be kept in mind in patients who need magnesium sulfate for more than 7 days [
14].
In conclusion, the efficacy and safety of magnesium sulfate was similar to ritodrine, and can be a substitute tocolytics. Additionally, failure of tocolytic therapy was determined by gestational age at treatment, twin gestation, intra-amniotic infection and maternal CRP, not by the type of tocolytics.








 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download