This article has been
cited by other articles in ScienceCentral.
Abstract
Objective
To evaluate the feasibility of robot-assisted laparoscopic myomectomy in multiple myomas over 10.
Methods
A retrospective study was conducted for 662 patients who underwent robot-assisted laparoscopic myomectomy and open myomectomy by a single operator in a tertiary university hospital.
Results
A total of 30 women underwent removal of 10 or more uterine myomas by robotics and 13 patients were selected for this study. The average number of myomas removed was 13.7 (range 10–20). The maximum diameter of the myomas was 6.8 cm (range 5.0–10.0 cm). The sum of the diameters of each myoma was 34.7 cm (range 20.0–54.5 cm) and the mass of resected myomas for each case was 229.1 g (range 106.8–437.9 g). In no case was the robotic procedure converted into conventional laparoscopy or laparotomy, and all patients recovered without any major complications. In comparison with 13 cases of open myomectomy during the same period, robotic surgery took longer time than open surgery (360.5 vs. 183.8 minutes; P=0.001) but had shorter postoperative hospital days after surgery (mean 2.5 vs. 3.5 days; P=0.003).
Conclusion
Robot-assisted laparoscopic myomectomy could be an alternative to laparotomic myomectomy for numerous myomas over 10 in number.
Keywords: Leiomyoma, Uterine myomectomy, Minimally invasive surgical procedures, Robotic surgical procedures
Introduction
Uterine myomas occur in 20%–40% of women during the reproductive period [
12]. The relationship between uterine myomas and infertility has been a concern in gynecology, since myomas tend to have a negative influence on fertility [
2]. In the treatment of women with infertility unexplained other than the presence of myomas, myoma resection is a treatment option for fertility preservation [
3].
There are various methods to perform myomectomy. In cases of unfavorably located or numerous myomas, the majority of patients who undergo myomectomy select a laparotomic approach to preserve the uterus and maintain fertility. The most important reason for this approach is to ensure increased strength of the uterine scar after its repair [
45]. As with any surgical procedure, myomectomy carries risks of morbidity and complications that could necessitate future cesarean sections and pelvic adhesions that could contribute to subsequent infertility. For reducing infertility caused by adhesions, laparoscopic myomectomy has been a preferred method of treatment. However, bulk closure technique in laparoscopic repair can lead to an improper approximation of the myometrium because of the limitations in fixed port placement [
267].
Robotic surgical techniques have been developed as an alternative method for overcoming difficulties caused by traditional laparoscopic myomectomies, and its clinical advantages have been well documented over the years. Ascher-Walsh and Capes [
8] reported that robot-assisted laparoscopic myomectomy appears to be an improvement over laparotomy in operative and postoperative variables except for the mean duration of surgery. In their study, however, the pool of patients was limited to those with 3 or fewer myomas at the time of preoperative magnetic resonance imaging (MRI) assessment due to the absence of haptic perception in robotics.
In this study, we evaluated the feasibility and efficacy of robot-assisted laparoscopic myomectomy in patients with numerous myomas over 10 in number, and then compared the outcomes with those of open myomectomy. Preoperative MRI and intraoperative sonographic navigation of the myomas were performed to complement the absence of haptic sense of the robotic techniques.
Materials and methods
1. Study participants and design
A retrospective chart review was conducted on 662 patients who underwent robot-assisted laparoscopic myomectomy and open myomectomy by a single operator at Seoul St. Mary's Fibroid Center between October 1, 2010 and September 30, 2016. Among 30 candidates, 13 patients who had 10 or more uterine myomas removed were selected for this study. Preoperative MRI and operative findings were used to select the appropriate cases, and patients who underwent combined surgery for stage III/IV endometriosis or hysteroscopic surgery were excluded. Indications for robot-assisted laparoscopic myomectomy included patients with symptomatic leiomyomas whose uterus size was under 20 weeks of gestational age. As a result, 13 cases of robot surgery and 13 cases of open surgery were ultimately selected for this study. Patient information was collected in a manner as approved by the Clinical Trial Review Committee of Seoul St. Mary's Catholic Medical University Hospital.
A computerized database was created to record the demographic information as well as the characteristics of the removed myomas, including the maximum diameter of the myomas, the sum of the diameters of each myoma, and the mass of removed myomas. Another set of data was created to record operative and postoperative variables such as the following: mean operative time (minutes), mean console time (minutes), estimated blood loss (mL), change in postoperative hemoglobin level (g/dL), whether or not the patient received a transfusion, whether there were acute complications, and the length of the postoperative hospital stay (days).
2. Surgical procedures
Robotic surgeries were performed using the da Vinci robotic surgical system. Patients were placed in the head-down lithotomy position with pads on both shoulders under general endotracheal anesthesia. Four trocars were typically placed after pneumoperitoneum was obtained. A 12-mm trocar for the camera port was placed at or above the umbilicus, depending on the size of the uterus. Two 8-mm trocars that served as 2-operating arms were each placed in the left and right lower quadrants. A 5-mm trocar for the assist port was placed 4 centimeters vertically upward from the median point between the right lower quadrant port and the camera port. A bedside surgical assistant conducted the introduction of the suction-irrigation instruments and suture materials through the assist port. A surgical cart with 3 robotic arms was placed and docked on the right side of the patient to facilitate manipulation of the uterus, which was conducted between the patient's legs. A camera arm was attached to the umbilical or supraumbilical trocar. Two operating arms were attached to right and left lower quadrant trocars. After inspection for the operative field, we performed a tubal patency test with indigocarmine through the uterine manipulator. For hemostasis, a diluted solution of vasopressin (20 U in 200 mL of saline) was injected into the serosa and the myometrium surrounding the myoma by an aspiration needle through the assist port. A scissor on the right arm and forceps on the left arm were used for a cold-knife cut, through which the uterine serosa was incised without thermal damage. The myomectomy was conducted with scissors and a tenaculum on each robotic arm. The center of resected myomas was pierced and hung up on the umbilical ligament using a needle and PDS 2-0 (Ethicon, Somerville, NJ, USA) thread before starting morcellation so that the resected myomas may not be lost from the operative visual field. A 2-layered continuous suture was performed with PDS 2-0 to repair the myometrium, and the edge of the serosa was closed with a continuous “baseball” stitch with PDS 2-0. Intraoperative ultrasonography with ALOKA SSD-4000 (Hitachi Aloka Medical Ltd., Tokyo, Japan) was performed in real time to determine the location of the myomas and remnant myomas. After each robotic arm was undocked, the resected myomas were removed by power morcellation under conventional laparoscopy. In cases of severe degenerated myomas, we used contained power morcellation in specimen bags. After irrigating pelvis and abdomen, its fluid was suctioned and an adhesion barrier was placed. Finally, fascia and skin of the ports site used for the robotic arms and camera were sutured.
Laparotomic myomectomy was also performed by the same operator who performed robot-assisted laparoscopic myomectomy. Under general anesthesia, the patients were placed in supine position. The skin was incised through Pfannenstiel skin incision. After the removal of myomas, the remaining uterine myometrium and serosa were repaired using a multilayer sutured closure. Blood loss was estimated by noting the difference between volumes of suctioned and irrigated fluid.
3. Statistical analysis
Statistical analysis was performed with SPSS ver. 21.0 (IBM Corp., Armonk, NY, USA). We conducted a Shapiro-Wilk test to determine whether the data were normally distributed. Comparisons of patient characteristics and surgery outcomes between the laparotomy and the robotic groups were performed using Student's t-test and χ2 test for normally distributed data and Mann-Whitney U test for non-normally distributed data. A P-value of less than 0.05 was considered significant. Pearson's correlations were used to calculate the associations between the operative time and the characteristics (number, size, mass) of the myomas.
Results
Between October 1, 2010 and September 30, 2016, a total of 13 women underwent removal of 10 or more uterine myomas by robot-assisted laparoscopic myomectomy. The patient age was 37.0±3.3 years (range 32–43 years), and the patient body mass index was 21.6±2.8 kg/m
2 (range 17.7–26.1 kg/m
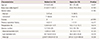
2). All of the patients were nulliparous and desired future fertility. The location and the type of the myomas were diverse (The International Federation of Gynecology and Obstetrics [FIGO] type 2–7 and hybrid type). The number of removed myomas for each case was 13.7 (range 10–20). The maximum diameter of the myomas was 6.8 cm (range 5.0–10.0 cm). The sum of the diameters of each myoma was 34.7 cm (range 20.0–54.5 cm) and the mass of resected myomas for each case was 229.1 g (range 106.8–437.9 g). There were no statistically significant differences in the baseline characteristics between the laparotomy group and the robotic surgery group, except for the sum mass of resected myomas (
Table 1).
Table 1
Baseline characteristics
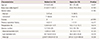
|
Characteristics |
Robot (n=13) |
Open (n=13) |
P-value |
|
Age (yr) |
37.0 (32–43) |
38.1 (33–45) |
0.437 |
|
Body mass index (kg/m2) |
21.6 (17.7–26.1) |
23.4 (19.4–29.4) |
0.103 |
|
Marital status |
|
|
0.185 |
|
Married |
2 (15.4) |
5 (38.5) |
|
Unmarried |
11 (84.6) |
8 (61.5) |
|
Gravida |
0 |
0 |
>0.999 |
|
Previous operation history |
3 (23.1) |
1 (7.7) |
0.277 |
|
Preoperative Hb |
12.8 (10.0–14.7) |
13.5 (11.0–15.1) |
0.614 |
|
Myoma number |
13.7 (10–20) |
13.5 (10–19) |
0.920 |
|
Maximal diameter (cm) |
6.8 (5.0–10.0) |
8.1 (5.0–11.5) |
0.125 |
|
Sum diameter (cm) |
34.7 (20.0–54.5) |
36.6 (20.5–45.8) |
0.574 |
|
Mass (g) |
229.07 (106.8–437.9) |
391.8 (122.0–899.6) |
0.036 |
In the robotic surgery, the mean operation time was 360.5 minutes, and the console time was 260.1 minutes. Changes in the postoperative hemoglobin level were calculated while excluding the cases of blood transfusion during operation, denoting the difference between the hemoglobin level upon admission and that on postoperative day. The change in the postoperative hemoglobin level was −2.4 mL. Blood transfusion was administered to 2 patients. No patient had any major complications or underwent a conversion to a conventional laparoscopy or laparotomy. The mean postoperative hospital stay was 2.5 days. All of the resected myomas underwent inspection and were confirmed as leiomyomas in the postoperative pathology report.
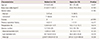
A comparison of the operative and postoperative variables between the robotic surgery group and laparotomy group is given in
Table 2. The operation time was significantly longer in the robotic surgery group (mean 360.5 minutes) than in the laparotomy group (mean 183.8 minutes), but robotic surgery had less risk of transfusion during operation (15.4% vs. 46.1%) and shorter postoperative hospital days than open surgery (mean 2.5 vs. 3.5 days).
Table 2
Operative and post-operative outcomes

|
Characteristics |
Robot (n=13) |
Open (n=13) |
P-value |
|
Mean operation time (min) |
|
|
|
|
Total |
360.5 (223–520) |
183.8 (115–250) |
0.001 |
|
Console time |
262.1 (143–450) |
0.006 |
|
Combined operation |
|
|
|
|
Total |
4 (30.8) |
1 (7.7) |
0.135 |
|
Endometriosis spot electrocoagulation |
3 |
1 |
|
|
Paratubal cystectomy |
1 |
0 |
|
|
EBL (mL) |
219.2 (70–700) |
323.1 (100–1,000) |
0.724 |
|
Δ Hemoglobin (g/dL)a)
|
2.4 (0.5–4.4) |
2.7 (0.3–4.7) |
0.528 |
|
No. of transfusion needed |
2 (15.4) |
6 (46.1) |
0.089 |
|
Postoperative abdominal drain |
4 (30.8) |
4 (30.8) |
>0.999 |
|
Length of stay (day)b)
|
2.5 (2–4) |
3.5 (3–5) |
0.003 |
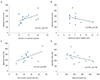
The maximum size of myoma and total mass of myomas tended to have a negative correlation with the operative time, while the number of resected myomas and the sum of each myoma size tended to have a positive correlation. However, there was no statistical significance in their relationship between the operative time and myoma characteristics (
Fig. 1).
Fig. 1
The relations between the operative time and the characteristics of the removed myomas. (A) The number of resected myomas, (B) the maximum diameter of the myomas, (C) the sum of the diameters, and (D) the mass of resected myomas were not significantly correlated with the operative time.
Discussion
Minimally invasive surgery has been leading the trend in diverse surgical fields and continues to evolve as a developing technology. Compared with myomectomy by laparotomy, laparoscopic approach is associated with shorter hospital stay, faster recovery, less postoperative pain, and reduced adhesion formation [
91011]. An extensive review of laparoscopic myomectomy concluded that a meticulous repair of the myometrium is essential for any women considering pregnancy after a laparoscopic myomectomy to minimize the risk of uterine rupture [
71213]. Because of the limitations in laparoscopic approach and suboptimal suturing results, laparotomic myomectomy is considered as an optimal treatment in cases of unfavorably located and numerous myomas. In such situations, we evaluated the feasibility and efficacy of robot-assisted laparoscopic myomectomy technique for patients with 10 or more myomas in comparison to laparotomic myomectomy.
The mean operative time (360 minutes) was statistically longer in robotic surgery group than in laparotomy group due to the increased setup time required in robotic surgery and the prolonged morcellation time. In fact, our mean operative time and mean console time were considerably longer than operative time reported in other studies regarding robot-assisted laparoscopic myomectomy. It would be rational to assume that the prolonged time of our surgery is attributed to the numerous number of myomas and the execution of intraoperative sonogram to localize small and deep intramural myomas. However, as shown in
Fig. 1A, there were no significant positive correlations between the operative time and the number of myomas in our experience of robot-assisted laparoscopic myomectomy of 10 or more myomas. While robotic surgery does require longer time to execute than open myomectomy, the number of myomas itself did not seem to be a factor that can serve as a limitation in application of robot-assisted laparoscopic myomectomy.
In addition, the operative and postoperative outcomes of robotic surgery were favorably comparable to those of laparotomic surgery. Robotic surgery had no major complications and shorter length of hospital stay. The number of patients who received transfusion was also less in robotic surgery group than in open surgery group, although there was no statistical significance due to the small number of reported cases. Advincula et al. [
11] further adds that the robotic approach has numerous significant societal benefits such as decreased estimated blood loss, complication rates, and length of stay which outweighs the possible financial burden of the surgery.
In spite of numerous benefits of robotic surgery, financial burden can be regarded as an important limitation. The cost of robotic surgery is about 4 or 5 times more expensive than conventional laparotomic myomectomy in Korea because the Korean National Health Insurance system does not cover robotic surgery. However, the patients who underwent Robot-assisted laparoscopic myomectomy were able to return to their daily activities and jobs faster than those who underwent laparotomic myomectomy. It can be argued that although an immediate hospital cost of the robotic surgery is more expensive than that of the open surgery, the robotic surgery may have a secondary financial benefit by providing lower complication rate and shorter length of hospital stay. As we did not perform a cost-benefit analysis in this study, cost-effective analysis will be needed in the future to confirm whether this is true.
Another important concern in myomectomy is a possibility of uterine rupture during pregnancy. It is possible to reduce the risk of uterine rupture during pregnancy by a surgical method that restricts the use of electrocautery and achieves multi-layer suturing of the myometrium instead of single-layer suturing. This can be done by providing good myometrial approximation [
14]. We incised the uterine serosa with a scissor without thermal damage that is called “cold-cut”. We also sutured the remnant myometrium in a 2-layered continuous method for full-thickness repair of the myometrium, and repaired the edge of the serosa with a continuous “baseball” stitch for prevention of adhesion. Among 13 patients of robotic surgery group in our study, 2 patients got pregnant post-surgery and delivered on full-term by cesarean section without any obstetric complications.
It is technically difficult to perform myomectomy on small myomas that are deeply situated, and this problem arises with laparotomy as well. The previous studies mentioned that robot-assisted laparoscopic myomectomy had limitation with small intramural myomas not visible on the surface because robotic surgery lacks equivalent haptic perceptions available in open surgery [
815]. For this reason, Ascher-Walsh and Capes [
8] were limited to cases with 3 or fewer myomas in robot-assisted laparoscopic myomectomy. However, we revealed that robot-assisted laparoscopic myomectomy is a possible treatment option in cases of numerous myomas over 10 or small deep intramural myomas. To overcome the absence of haptic sense of the robotics, we performed intraoperative sonographic navigation and palpation by an assistant as well as a preoperative MRI assessment to localize small and deep myomas.
The present study has several limitations. First, it was a retrospective chart review of a small pool of samples. There might be bias in analysis because only 13 patients of robotic surgery and 13 patients of open surgery were included in this study. Second, the information regarding outcomes of pregnancy was insufficient. Since only a few patients became pregnant after undergoing robot-assisted laparoscopic myomectomy, more studies will be needed in the future to fully evaluate and determine the effectiveness of robotic surgery in pregnancy outcomes.
All of the patients in this study were nulliparous women of childbearing age. They were recommended to receive abdominal myomectomy or even hysterectomy at other hospitals. Therefore, the satisfaction of patients who received robot-assisted laparoscopic myomectomy was remarkable. From this point of view, robotic surgery with supplementary techniques such as preoperative MRI, intraoperative sonographic navigation and palpation by an assistant to localize myomas could be suitable alternatives to an abdominal myomectomy.
In conclusion, a robot-assisted laparoscopic myomectomy is a feasible treatment option as a way to preserve fertility for patients with more than 10 myomas. In the future, additional evaluation with larger sample size will be needed to provide further details on long-term pregnancy outcomes of the patients who underwent robot-assisted laparoscopic myomectomy for numerous myomas.
Acknowledgements
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT and Future Planning (2012R1A1A3020083) and the Ministry of Education (2017R1D1A1B03028045). In addition, we would like to thank Jeeyune Park for English proofreading and Sol Kim and Hye-Sung Hwang for their support.
References
1. Practice Committee of the American Society for Reproductive Medicine. Myomas and reproductive function. Fertil Steril. 2004; 82:Suppl 1. S111–S116.
2. Somigliana E, Vercellini P, Daguati R, Pasin R, De Giorgi O, Crosignani PG. Fibroids and female reproduction: a critical analysis of the evidence. Hum Reprod Update. 2007; 13:465–476.

3. Pritts EA, Parker WH, Olive DL. Fibroids and infertility: an updated systematic review of the evidence. Fertil Steril. 2009; 91:1215–1223.

4. Seracchioli R, Rossi S, Govoni F, Rossi E, Venturoli S, Bulletti C, et al. Fertility and obstetric outcome after laparoscopic myomectomy of large myomata: a randomized comparison with abdominal myomectomy. Hum Reprod. 2000; 15:2663–2668.

5. Mais V, Ajossa S, Guerriero S, Mascia M, Solla E, Melis GB. Laparoscopic versus abdominal myomectomy: a prospective, randomized trial to evaluate benefits in early outcome. Am J Obstet Gynecol. 1996; 174:654–658.

6. Bedient CE, Magrina JF, Noble BN, Kho RM. Comparison of robotic and laparoscopic myomectomy. Am J Obstet Gynecol. 2009; 201:566.e1–566.e5.

7. Hurst BS, Matthews ML, Marshburn PB. Laparoscopic myomectomy for symptomatic uterine myomas. Fertil Steril. 2005; 83:1–23.

8. Ascher-Walsh CJ, Capes TL. Robot-assisted laparoscopic myomectomy is an improvement over laparotomy in women with a limited number of myomas. J Minim Invasive Gynecol. 2010; 17:306–310.

9. Chiou HY, Chiu LH, Chen CH, Yen YK, Chang CW, Liu WM. Comparing robotic surgery with laparoscopy and laparotomy for endometrial cancer management: a cohort study. Int J Surg. 2015; 13:17–22.

10. Dubuisson J, Botchorishvili R, Perrette S, Bourdel N, Jardon K, Rabischong B, et al. Incidence of intraabdominal adhesions in a continuous series of 1000 laparoscopic procedures. Am J Obstet Gynecol. 2010; 203:111.e1–111.e3.

11. Advincula AP, Xu X, Goudeau S 4th, Ransom SB. Robot-assisted laparoscopic myomectomy versus abdominal myomectomy: a comparison of short-term surgical outcomes and immediate costs. J Minim Invasive Gynecol. 2007; 14:698–705.

12. Parker WH, Einarsson J, Istre O, Dubuisson JB. Risk factors for uterine rupture after laparoscopic myomectomy. J Minim Invasive Gynecol. 2010; 17:551–554.

13. Nezhat C, Lavie O, Hsu S, Watson J, Barnett O, Lemyre M. Robotic-assisted laparoscopic myomectomy compared with standard laparoscopic myomectomy--a retrospective matched control study. Fertil Steril. 2009; 91:556–559.

14. Ten Broek RP, Kok-Krant N, Bakkum EA, Bleichrodt RP, van Goor H. Different surgical techniques to reduce post-operative adhesion formation: a systematic review and meta-analysis. Hum Reprod Update. 2013; 19:12–25.

15. Advincula AP, Song A. The role of robotic surgery in gynecology. Curr Opin Obstet Gynecol. 2007; 19:331–336.